To evaluate the results and efficacy of cementless total hip arthroplasty (THA) in octogenarians with osteoarthritis.
Material and methodsMatched case–control study with ratio 1:2. Consecutive selection of 54 octogenarians (55 hips), and 106 control patients (110 hips) with age ranging from 70 to 79 years. Mean follow-up of 7 years (range, 5–12). Before 5 postoperative years, 1 and 4 patients, respectively, died and they were excluded. Clinical assessment was performed using ASA grade, comorbidities, and Harris and Merle d’Aubigné hip scores, and radiographic, complications, and mortality evaluations were made.
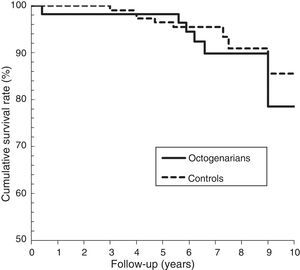
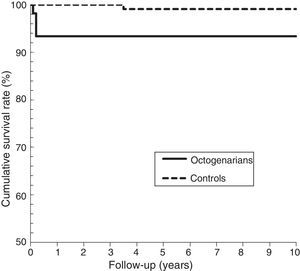
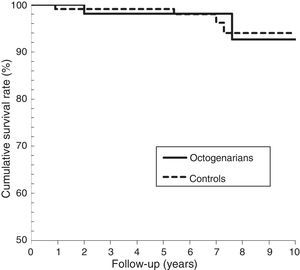
ResultsThere were no perioperative deaths in either cohort. The rates of postoperative medical complications (P=.601) and survival (P=.360) were similar. The survival at 7 years was 89.8% in octogenarian and 95.3% in controls, with no influence of the preoperative variables. There were no differences in postoperative functional outcomes (P=.761), but improvement with respect to the preoperative was higher in octogenarian (P=.002). In octogenarians there were 2 intraoperative fractures, 2 dislocations and 2 unstable stems, and in control patients 1 deep infection, 1 peri-prosthetic femoral fracture, 2 unstable cups and 4 unstable stems. The rates of aseptic complications, the need for revision, and arthroplasty survival (94% at 7 years) were similar in both cohorts.
DiscussionDue to improvement in health status, the octogenarian may have a life expectancy of at least 10 years. The cost arguments and an arbitrary age should not influence the selection of candidates for cementless THA.
ConclusionsCementless THA has been shown to be safe and effective in octogenarian patients with osteoarthritis. The notable increase found in functional outcomes justifies the continued use in these patients.
Valorar resultados y eficacia de la artroplastia total de cadera (ATC) no cementada en octogenarios con coxartrosis.
Material y métodosEstudio de caso-control con emparejamiento 1:2. Selección consecutiva de 54 octogenarios (55 caderas) y 106 controles (110 caderas) con edad 70-79 años. Seguimiento medio de 7 años (rango, 5-12). Antes de 5 años de seguimiento murieron 1 y 4 pacientes, respectivamente, siendo excluidos. Se realizó valoración clínica mediante ASA, comorbilidades, escalas de Harris y Merle D’Aubigné, y valoración radiográfica, de complicaciones y de mortalidad.
ResultadosEn ambas cohortes no hubo muertes perioperatorias, siendo similar la tasa de complicaciones médicas (p=0,601) y la supervivencia (p=0,360) que a 7 años fue 89,8% en octogenarios y 95,3% en controles, no influyendo las variables preoperatorias. No hubo diferencias en los resultados funcionales postoperatorios (p=0,761) pero los octogenarios tuvieron mayor incremento (p=0,002) respecto al preoperatorio. En octogenarios hubo 2 fracturas intraoperatorias, 2 luxaciones y 2 vástagos inestables. En los controles, 1 infección profunda, 1 fractura periprotésica femoral, e inestabilidad en 2 cotilos y 4 vástagos. Las tasas de complicaciones asépticas, de necesidad de revisión y de supervivencia de la artroplastia (94% a 7 años) fueron similares en ambas cohortes.
DiscusiónEl incremento en el estado de salud hace que los octogenarios tengan una expectativa de vida de al menos 10 años. El argumento de costes y una edad arbitraria no debe influir en la selección de candidatos a ATC no cementada.
ConclusionesLa ATC no cementada se ha mostrado segura y efectiva en los octogenarios con coxartrosis. El notable incremento encontrado en los resultados funcionales justifica el continuar utilizándola en estos pacientes.
Total hip arthroplasty (THA) is a common surgical procedure, especially in elderly people, with highly satisfactory results. Cemented fixation is still considered the reference standard due to the longer follow-up.1 The increase in life expectancy has made it so that elderly patients are more frequently candidates for THA. In younger patients, the advantage of a cementless prosthesis favors biological fixation through osseointegration so that the prosthetic lasts longer.2 In elderly patients, other potential advantages have been proposed, such as reducing the risk of embolism admitted in cemented prostheses, operative time, and blood loss.3 All of these factors are relevant for patients in a more fragile health state. Despite the fact that the objective of THA is to relieve pain and facilitate functioning, other decision factors have been introduced in the selection of implants for elderly patients, such as cost containment,4 even though there is evidence advising against making a selection based solely on age.2
Even though many studies have been published regarding the benefits of primary THA in octogenarian patients, most of them used cemented prostheses.5,6 The use of cementless primary prostheses in patients older than 80 years continues to be controversial,7 even though there are few studies in this respect. We only found 3 studies involving case series of primary arthroplasties,2,8,9 and none of them were comparative. Another study,7 although it presented results involving fixation in octogenarians, was weak in its design as it was a descriptive study based on a national registry of arthroplasties. Therefore, it did not present an adequate selection of cohorts for result comparison.
The objective of this study was to assess the results, complications, and efficacy of elective cementless primary THA in a population 80 years or older.
Material and methodsThis work was designed as a retrospective, comparative, observational matched case–control study, approved by our institution's clinical research ethics committee. A minimum of 5 years of postoperative follow-up was required for the results analysis.
From our department's computerized arthroplasty registry, we identified a total of 712 cementless primary THAs performed by the 2 authors (ALU and JSR) in patients with hip osteoarthritis between January 2004 and December 2007. Of these, 55 consecutive THAs had been implanted in 54 patients 80 years or older. In our department, the use of both cementless components was routine in coxarthrosis, except in patients whose preoperative functional state predicted very limited ambulatory ability after the intervention. Three octogenarian patients were found to be in this situation; they received a cemented THA and were consequently not included in the study.
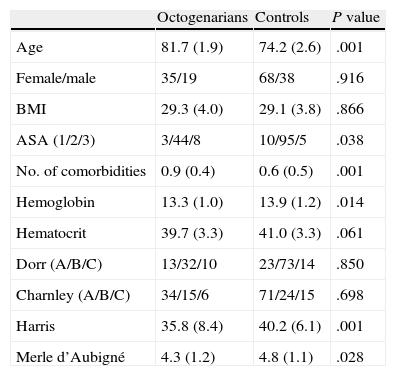
Using the same database, a control cohort was selected of patients aged 70–79 years that underwent a cementless THA operation due to hip osteoarthritis, 69 years being the median age for patients undergoing this surgery in our department. The study was initially designed with 1:2 matching (2 controls for each case) according to different preoperative variables (sex, body mass index [BMI], previous health state, previous functioning, bone quality of the proximal femur, etc.). However, given the difficulty in obtaining 2 appropriate controls, we decided to match with respect to only the following variables: sex, diagnosis, prosthesis design, surgery, and implantation date. The controls were 2 patients that complied with the criteria, undergoing the operation immediately after their respective case. Even though this matching was not very strict, the control group was comparable to that of the study group in many characteristics (Table 1).
Preoperative and demographic data.
| Octogenarians | Controls | P value | |
| Age | 81.7 (1.9) | 74.2 (2.6) | .001 |
| Female/male | 35/19 | 68/38 | .916 |
| BMI | 29.3 (4.0) | 29.1 (3.8) | .866 |
| ASA (1/2/3) | 3/44/8 | 10/95/5 | .038 |
| No. of comorbidities | 0.9 (0.4) | 0.6 (0.5) | .001 |
| Hemoglobin | 13.3 (1.0) | 13.9 (1.2) | .014 |
| Hematocrit | 39.7 (3.3) | 41.0 (3.3) | .061 |
| Dorr (A/B/C) | 13/32/10 | 23/73/14 | .850 |
| Charnley (A/B/C) | 34/15/6 | 71/24/15 | .698 |
| Harris | 35.8 (8.4) | 40.2 (6.1) | .001 |
| Merle d’Aubigné | 4.3 (1.2) | 4.8 (1.1) | .028 |
For continuous variables, the data are presented as mean (SD).
The mean age of the 54 octogenarian patients (55 hips) was 81.7 years (range: 80–87; standard deviation [SD]: 1.9), with 35 females and 19 males. The right hip was affected in 28 patients, the left in 23, and both in 2. The control cohort consisted of 110 hips in 106 patients, with a mean age of 74.2 years (range: 70–79; SD: 2.6), including 68 females and 38 males. The right hip was affected in 69 patients, the left in 33, and both in 4. As expected, there were significant differences between both cohorts with respect to age, American Society of Anesthesiologists (ASA) grades,10 number of comorbidities, and preoperative hip functioning; but not regarding sex, BMI, Charnley categories,1 or proximal femur types according to Dorr11 (Table 1).
Previous health state was assessed using ASA grades10 and the number of significant comorbidities for hip surgery in elderly patients, defined by Holt et al.12 Of the octogenarians, 50 hips were associated with 1 comorbidity or none at all, and 5 with 2 comorbidities, the most common being hypertension (85%), heart disease (7%), and chronic obstructive pulmonary disease (5%). Of the controls, 105 had 1 pre-existing comorbidity or none at all, and 5 had 2 comorbidities; the most common were hypertension (50%), chronic obstructive pulmonary disease (6%), and heart disease (3%). Based on comorbidity presence, the odds ratio for octogenarians was 3.52 (95% confidence interval [CI]: 1.70–7.24) and 0.63 (95% CI: 0.52–0.77) for controls. The octogenarians showed a 5.5 times higher risk of presenting comorbidity (P=.001). Preoperatively (Table 1), the octogenarians had a lower level of hemoglobin than the controls (P=.014), even though the 2 groups shared a similar hematocrit level (P=.061).
Surgical protocolAll surgeries were carried out in a laminar flow clean room, using low spinal anesthesia, and with the same standard surgical technique using a modified Hardinge13 lateral approach. In all cases, both cementless components were used. Two THA systems were implanted according to the surgeon's preference. One was the Duofit® system (cup and stem; Samo, Bologna, Italy) and the other was a Vitalock® cup with a Meridian® stem (both from Stryker, Mahwah, USA). Both systems had similar geometry. The stems were straight and without a neck, composed of titanium alloy, the upper third coated in circumferential plasma-spray, and they had holes for additional stability with screws. In all cases – octogenarian and control – 2 divergent screws were used. All femoral heads were 28mm, modular, and made of cobalt chromium. All the inserts were polyethylene with a high molecular weight and 12° elevation, sterilized by gamma irradiation.
All patients followed the same standard postoperative protocol. Perioperative antibiotic prophylaxis with first generation cephalosporin was done within 24h. Thromboprophylaxis with low molecular weight heparin was given within 1 month. Patients underwent a postoperative blood transfusion if their hemoglobin was less than 8g/dl. Prophylaxis was not used for heterotopic ossification in any cases. Patients were allowed ambulatory freedom the day following the intervention, if tolerated.
EvaluationsOur department's registry of arthroplasties has clinical and radiographic data for all patients treated with arthroplasties. Follow-up was prospective and standardized, with postoperative assessments at 6 weeks, 1 year, and then annually until at least 5 years after the operation. Medical registries of patients were reviewed to extract relevant information regarding diagnosis, surgery details, postoperative hospital stay, functional and radiographic results, complications, and mortality. With respect to the last factor, all patients were also contacted by telephone.
Before their operations, all patients were examined – and medically treated if necessary – by an internal medicine doctor and an anesthesiologist. Preoperative health state was defined by ASA grades10 and the number of pre-existing comorbidities.12 Patients were classified by their functioning according to the Charnley categories.1 The objective preoperative assessments and the postoperative follow-ups were done by trained residents. For clinical functioning, the Harris14 and Merle d’Aubigné15 scales were used. Anterior thigh pain was assessed as absent, mild, moderate, or severe using the same criterion as that used in the pain category from the Harris scale.
Standard AP and lateral X-rays were taken preoperatively and at each postoperative evaluation. Before the operation, bone quality and proximal femur morphology were determined according to Dorr et al.11 The 6-week postoperative X-rays were compared to those from the last evaluation done in order to determine component stability. To localize radiolucent lines, osteolysis, or bone remodeling, DeLee and Charnley zones16 were used for the acetabular component, while Gruen17 zones were used for the femoral component. Radiolucent lines were categorized as absent or greater than 1mm, and osteolyses were considered to be greater than 5mm. The position of the cup was determined according to the Massin et al.18 criteria, and its stability according to criteria proposed by González Della Valle et al.19 for cementless cups. Acetabular weakening was considered when there was a position change of at least 2mm or 2°, continuous radiolucency of 1mm or greater, or periacetabular osteolysis or osteolysis around the screws. With respect to the femoral component, stability was determined according to criteria from Engh et al.20 for cementless stems. They were considered weak if there was progressive subsidence greater than 5mm, angular position change of 3° or more, radiolucency width greater than 2mm, or osteolysis. Heterotopic ossification was evaluated according to Brooker et al.21
Statistical analysisThis analysis was done using version 15.0 of the SPSS® program (SPSS Inc., Chicago, USA). P values equal to or less than 0.05 were considered significant. In order to determine normal distribution, the Kolmogorov–Smirnov test was used. For comparisons between cohorts, univariate analyses were carried out for categorical variables using the Chi-squared test in variables with normal distribution, or the Mantel–Haenszel test for non-parametric data. The Student t or Mann–Whitney U tests were used for continuous variables. In comparing pre- and postoperative data, the Student t (for paired samples) or Wilcoxon Signed-Rank tests were used. Multivariate analyses were then carried out, using the variables that showed a significant difference in the univariate analysis as independent variables and mortality, resultant functioning, or prosthetic failures as dependent variables. Logistic regression analysis was used when the independent variable was dichotomous, while Cox regression was used when it was not. The odds ratio (OR) or hazard ratio (HR) were calculated with 95% confidence intervals. Kaplan–Meier analysis was used to calculate cumulative survival and the log-rank test was used to compare survival curves.
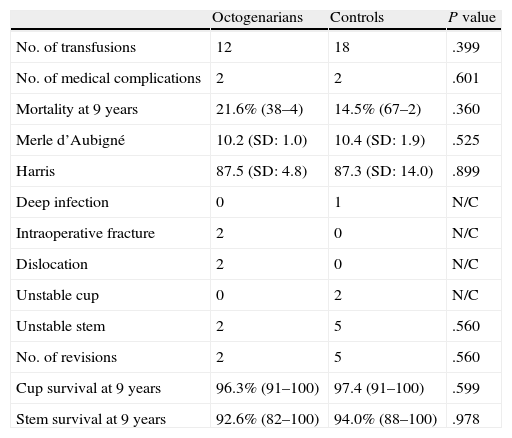
ResultsWe reviewed 54 octogenarian patients (55 hips), of which 1 died of colon cancer 5 months after the operation without premature hip complications. This patient was excluded from the results analysis. In the control cohort, there were 106 patients (110 hips), of which 4 died within 5 postoperative years (range: 3.0–4.7 years) from causes unrelated to the hip (lung cancer, digestive cancer, leukemia, heart attack). These 4 patients were also excluded from analysis. Other octogenarian and control patients died after 5 postoperative years. However, given the initial advanced age of these patients, they were not excluded from results analysis, as they complied with the minimum criteria. There were no other follow-up losses. Therefore, 53 octogenarian patients (54 hips) and 102 controls (106 hips) remained for analysis of results. The average postoperative follow-up was 7.1 years (range: 5–12; SD: 1.2) among the octogenarians and 7.3 years (range 5–12; SD: 1.4) in the controls (P=.366) (Table 2).
Postoperative results and complications.
| Octogenarians | Controls | P value | |
| No. of transfusions | 12 | 18 | .399 |
| No. of medical complications | 2 | 2 | .601 |
| Mortality at 9 years | 21.6% (38–4) | 14.5% (67–2) | .360 |
| Merle d’Aubigné | 10.2 (SD: 1.0) | 10.4 (SD: 1.9) | .525 |
| Harris | 87.5 (SD: 4.8) | 87.3 (SD: 14.0) | .899 |
| Deep infection | 0 | 1 | N/C |
| Intraoperative fracture | 2 | 0 | N/C |
| Dislocation | 2 | 0 | N/C |
| Unstable cup | 0 | 2 | N/C |
| Unstable stem | 2 | 5 | .560 |
| No. of revisions | 2 | 5 | .560 |
| Cup survival at 9 years | 96.3% (91–100) | 97.4 (91–100) | .599 |
| Stem survival at 9 years | 92.6% (82–100) | 94.0% (88–100) | .978 |
Survival rate (95% CI); SD: standard deviation; N/C: cannot be calculated.
The mean hospital stay for the octogenarians was 7.5 days (range: 4–13), and 7.3 days (range: 3–16) for the control cohort (P=.701). All patients came from their homes and were sent directly to them afterward.
Medical complications and postoperative mortalityPreoperatively, no blood transfusions were necessary for any patient. Postoperatively, transfusions were required in 12 (12.8%) octogenarians and in 18 (16.3%) control patients (P=.399).
The postoperative medical complication rate was not significantly different between the 2 cohorts (P=.601). Complications were present in 2 (3.7%) octogenarians (2 urinary infections) and in 2 (1.9%) controls (pneumonia and deep vein thrombosis without pulmonary embolism). As for the presence of medical complications, with the limited number of patients available, neither cohort was influenced by sex, ASA grade, or number of pre-existing comorbidities (P>.05).
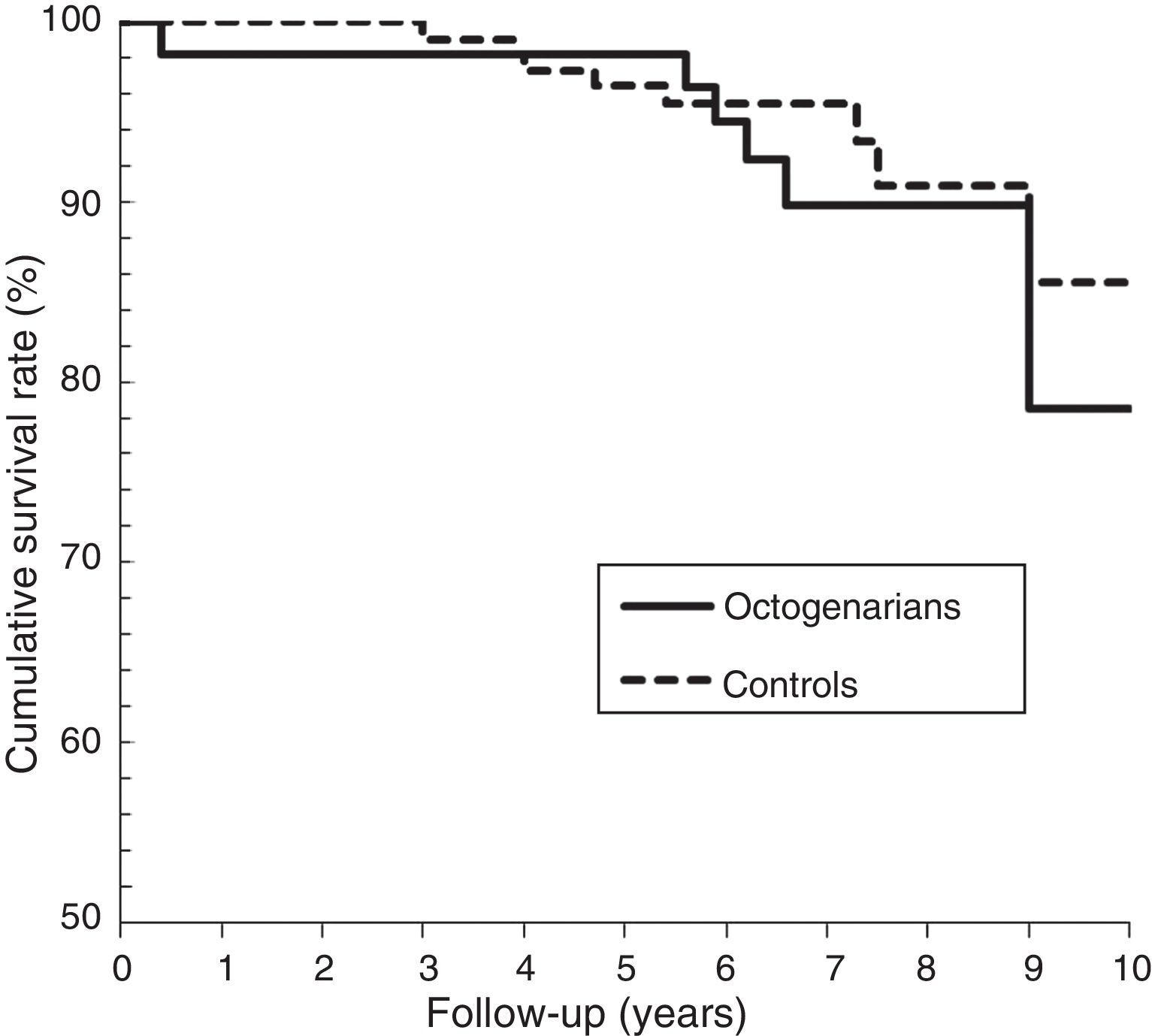
There were no perioperative deaths in either cohort. In the octogenarian group, 7 patients (12.9%) died in a mean postoperative period of 6.5 years (range: 5 months to 9 years), of which 6 patients died 5 or more years after the operation. In the control cohort, 9 patients (8.4%) died in a mean postoperative period of 6.0 years (range: 3–9 years), of which 5 patients died 5 or more years after the operation. No patient died from causes related to the hip surgery. The odds ratio (OR) for death in the octogenarian cohort was 1.35 (95% CI: 0.74–2.48), and it was 0.84 (95% CI: 0.53–1.29) for the controls, the difference being non-significant (P=.406). With the Kaplan–Meier analysis (Fig. 1), and considering death from whatever cause as an ending point, the cumulative survival rate was 98.1% (95% CI: 96.1–100) in the octogenarians between 1 and 5 postoperative years, and 78.4% (95% CI: 61.7–96.3) at 9 postoperative years. Furthermore, the rates for the controls were 99.0% (95% CI: 97.2–100) between 1 and 5 postoperative years and 85.5% (95% CI: 33.4–98.3) at 9 postoperative years. The log-rank analysis showed no significant differences between the cohorts (P=.360). Cox regression analysis revealed that, in both cohorts, the following were not significant independent predictors of mortality: sex, BMI, ASA grade, number of comorbidities, necessity for transfusion, postoperative medical complications, and type of prosthetic (P<.05).
Hip function resultsThe mean Merle d’Aubigné15 score increased from 4.3 (range: 2–7) preoperatively to 10.2 (range: 8–12) for the octogenarians in the last postoperative follow-up (P=.001), while the mean score on the Harris14 scale went from 35.8 points (range 20–54) to 87.5 (range: 77–96) (P=.001). According to the Harris criteria, 14 hips were classified as having excellent results, 38 with good results, 1 fair, and 1 poor result. Five patients reported mild thigh pain that did not affect their daily activities. Of the sample, 51 patients could walk outside of their home and 2 could only walk inside; 48 (90.5%) patients used walking support before the operation and 26 (49%) after the operation (P=.001).
The mean score for the control cohort on the Merle d’Aubigné scale increased from 4.8 (range: 2–8) preoperatively to 10.4 (range: 4–12) in the last postoperative follow-up (P=.001), while the mean Harris score went from 40.2 points (range: 24–53) to 87.3 (range: 44–98) (P=.001). According to the Harris criteria, 64 hips were classified as having excellent results, 36 with good results, 3 fair, and 3 poor results. Five patients reported mild thigh pain and 4 reported moderate or continuous pain that affected their functioning. Of the sample, 99 patients were able to walk outside of the house and 3 could only walk inside; 70 (66%) patients used walking support before the operation and 31 (29.2%) after the operation (P=.001).
There were no significant differences between the 2 cohorts in relation to thigh pain (P=.471), ability to walk (P=.399), or use of walking support (P=.175). In addition, there were no significant differences found in relation to postoperative Harris score (P=.899), Merle d’Aubigné score (P=.525), or type of prosthetic (P=.761). However, the octogenarians showed a significantly higher postoperative increase on the hip function scales compared to the controls (P=.002).
Radiographic resultsAccording to the classification used by Dorr et al.,11 there were 12 type A hips, 32 type B, and 10 type C among the 54 valid octogenarian hips; and among the 106 controls, there were 21, 71, and 14, respectively (P=.850). Clinical results were independent of bone type in both cohorts (P>.05).
In the octogenarians, the mean postoperative acetabular angle was 43.6° (range: 42–62°). In the acetabular components, there were no radiolucent lines greater than 1mm. Migration of the acetabular component was observed in 1 patient that had had a cup fracture during the operation, which resulted in the cup being considered unstable. There were no cases of osteolysis or screw breaks. Osseointegration was observed in the rest of the acetabular components. There were no radiolucent lines or osteolysis surrounding the femoral component, but 2 stems presented subsidence greater than 5mm, and were consequently considered unstable. According to the Engh et al.20 criteria, the other 52 stems presented osseointegration.
In the control group, the mean postoperative acetabular angle was 42.9° (range: 38–62°). There were radiolucent lines less than 1mm in 4 acetabular components, all of them confined to a single zone (1 and 2) and none of them were progressive. Another acetabular component had continuous radiolucency greater than 1mm, and still another showed migration, causing both to be deemed unstable. There were no cases of osteolysis or screw breaks. At the femoral level, there were radiolucencies less than 2mm in 12 stems, of which 4 were located in zone 1, 5 in zone 3, and 3 in zone 7. Four other stems showed progressive radiolucencies greater than 2mm. Two of those presented 3° migration and the other 2 showed subsidence of 5 and 6mm, all of them consequently considered unstable. According to the Engh et al.20 criteria, the rest of the femoral components were stable, 101 with osseointegration and 1 with asymptomatic stable fibrous fixation at 8 years.
In the octogenarians, there was 1 patient with Brooker et al.21 grade II heterotopic ossification, while the control cohort presented 2 cases of grade I ossification, 1 grade II, and 1 grade III. The ossifications presented in both groups had no clinical significance.
Orthopedic complications and surgical reviewsOne octogenarian patient had persistent drainage of the wound, which required early superficial cleaning and antibiotics, resulting in a final score of 91 points on the Harris14 scale. In the control cohort, 1 patient had a deep infection, treated with 2-step revision at 16 months, with a final functional result of 44 points.
Among the octogenarians, there was 1 patient with early dislocation treated using closed reduction, with a final functional result of 80 points. Another patient presented recurrent dislocation that only required switching from the acetabular to a well-placed cementless component at 2 months after the operation, with a functional result of 86 points. There were no dislocations in the control cohort.
There were intraoperative fractures in 2 octogenarian patients. In 1 case, it was an acetabular fracture seen at 1 month after the operation, which just required switching from the acetabular to a cementless component, resulting in a score of 80 points. The other was a diaphyseal fracture treated with cerclage, which resulted in 6mm stem subsidence at 2 years postoperative and with a functional result of 77 points. This patient rejected stem replacement. A third patient presented subsidence and femoral radiolucencies at 7.6 years after the operation, with a functional score of 80 points, and refused surgical revision.
In the control cohort, there were no intraoperative fractures. One patient suffered a periprosthetic femoral fracture from a fall 2 years after the operation, which was treated with open reduction and internal fixation, resulting in a functional score of 66 points. Of the other 4 stems considered unstable, 1 was revised at 11 months postoperatively with a functional result of 43 points. In the other 3, instability was detected at 5.4, 7.3, and 9.0 years postoperatively and the cups were not revised due to the patients’ refusal. These patients had functional scores of 61, 72, and 68 points, respectively. At the acetabular level, the 2 cups considered unstable were revised using cementless cups at 3.5 and 10.7 years postoperatively, with a final functional result of 66 and 62 points, respectively.
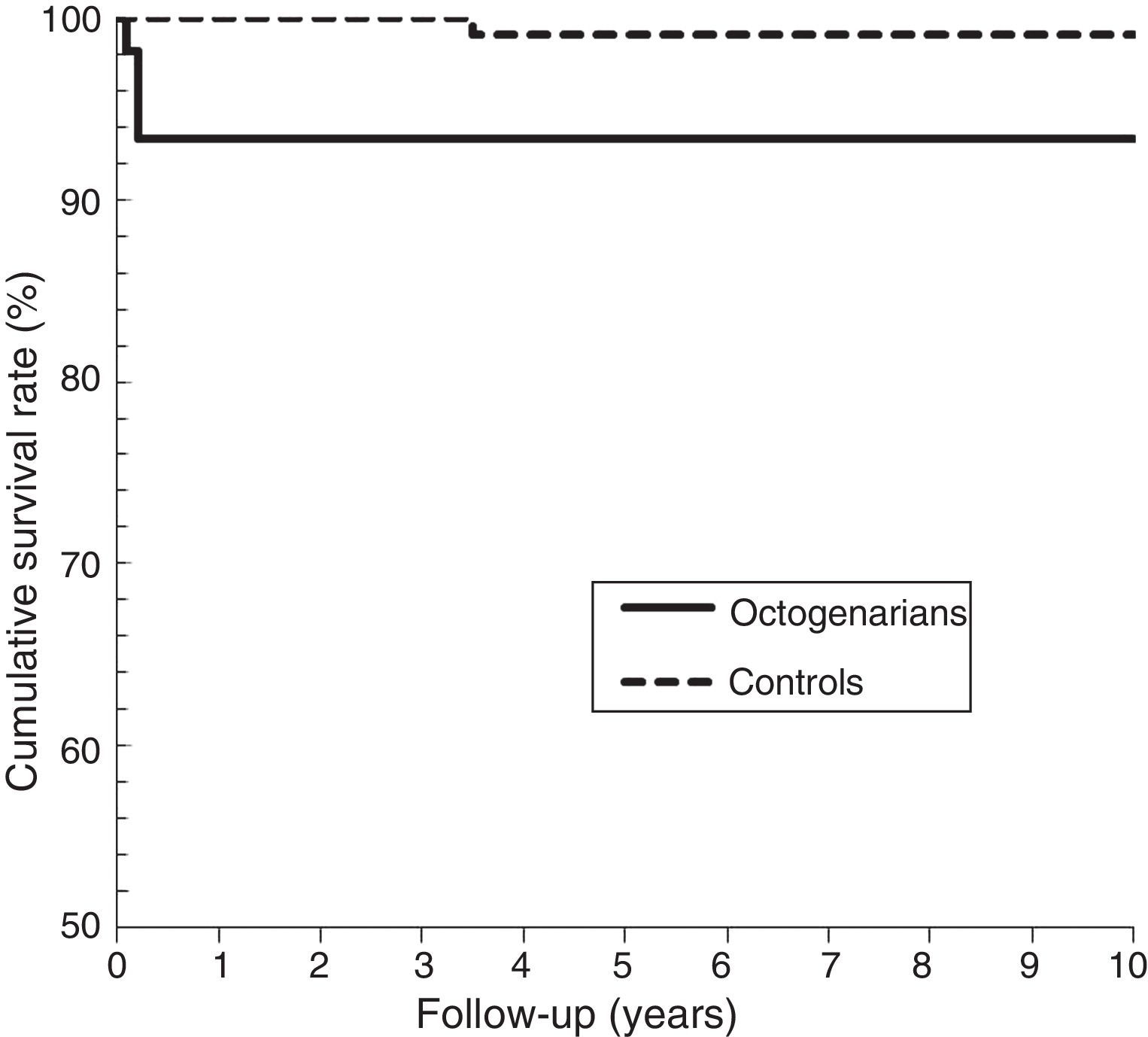
In summary, there were 4 (7%) hips (2 cups and 2 stems) in the octogenarian cohort and 7 (6.6%) hips (2 cups and 5 stems) in the control cohort with aseptic revision or need of it. The survival rate of the prosthesis at 9 years, with the final point being revision or need of it – not including the cases of septic revision or periprosthetic fracture – was 89.2% (95% CI: 78–100) in the octogenarian cohort and 86.3% (95% CI: 69.6–100) in the control cohort (log-rank, P=.728). For the acetabular component (Fig. 2), the survival rate was 96.4% (95% CI: 91–100) in the octogenarians and 97.4% (95% CI: 91.3–100) in the control cohort (log-rank, P=.599). For the femoral component (Fig. 3), the survival rate was 92.6% (95% CI: 82–100) in the octogenarians and 94.0% (95% CI: 88–100) in the control cohort (log-rank, P=.978). Cox regression analysis revealed that prosthesis failure, sex, BMI, Dorr category, and prosthesis type were not significant independent predictors in either cohort (P>.05).
DiscussionWe have not found comparative studies on the efficacy of the primary cementless prosthetic hip in patients older than 80 years. Consequently, our results could only be discussed with respect to other case series studies. The main weakness in our study was its retrospective design. Furthermore, even though our patients were consecutive, there could be an implicit selection process in the surgery indication, given that patients showed relatively good preoperative medical condition overall: 86% fell under grades 1 and 2 of the ASA.10
Total hip replacement has shown to be greatly advantageous in elderly patients,1 which is why it has been advised that the selection of candidates for this surgery not be done solely based on age.22,23 In previous studies carried out in our institution, we observed satisfactory results with cementless prostheses in young patients, at both the acetabular24 and femoral25 component levels. Nonetheless, there is controversy7 surrounding the type of fixation used in elderly patients. The convenience of cemented fixation at an arbitrary age has been postulated because of poor bone quality,11,26 as well as for economic reasons4 based on less physical demand and lower life expectancy for the patient. Our study indicated that the patient's age does not have to be a deciding factor in selecting the type of fixation for THA, as the increase in functional results showed its efficacy and the complication rates were similar in patients whose ages were within the range of our normal surgical practice.
Economic arguments for restricting the use of cementless prostheses in elderly patients have been refuted by other studies. Barrack et al.4 and Laupacis et al.27 determined the difference in costs between a cementless and cemented prosthesis to be irrelevant with the current cementation systems (costs of cementing, mixing device, pressurization, gun, cement cap, pulsating irrigation device). They also posited that in many cases, the current cost of a modern cemented prosthesis may be higher than a cementless one. Furthermore, cementless prostheses reduce intervention time and rates of hypotensive crisis, embolism, and, in general, adverse effects known as bone cement implantation syndrome.3 The increase in costs derived from the potential failure rate and consequential surgical revision for the cementless prosthetic in octogenarians is not supported by the lack of significant difference between that cohort and these rates in younger patients, as shown in our study and in those by other authors.2
In our study, there were no differences between the 2 groups regarding the risk of requiring postoperative transfusion, and the medical complications rate was similar, as reported by other authors.2,9 No perioperative deaths were observed and the mortality rate in the octogenarians after a mean follow-up of 7 years was 12.9%, which was not significantly different from that of the control group. Using cementless prostheses in octogenarians, Badhe et al.9 reported an 11% mortality rate at 7 years in 60 patients, and Keisu et al.2 reported no perioperative deaths and a mortality rate of 6% at 2 years in 114 patients. Using cemented prostheses in octogenarians, Ekelund et al.28 reported a 2% mortality rate in the first 3 months after the operation in a series of 162 patients.
In our octogenarian cohort, there were no cases of deep infection, 2 dislocations, 2 intraoperative fractures, and no weakening of acetabulum or aseptic stem weakening, all these figures being similar to those in the control cohort. There was a 7% rate of surgical revision or need of it. All this was similar to other studies with cementless prostheses in octogenarians.2,8,9 Other authors12 reported that there might have been defects in fixation due to poor bone quality. In our octogenarian group, all of the acetabulum showed osseointegration and only 1 stem was unstable because of subsidence. Badhe et al.9 reported 57 osseointegrated stems and 2 with subsidence, although asymptomatic, in their series of 59 octogenarians with a mean postoperative follow-up period of 7 years. In this study, all the cups were stable except for 2 asymptomatic fibrous ones. Keisu et al.2 reported that all acetabular and femoral components showed osseointegration in their series of 114 octogenarians with a mean follow-up of 7 years.
In our octogenarian group, the survival rate at 7 years, for aseptic reasons, was 96% for the acetabular component and 98% for the stem. Badhe et al.9 found a survival rate of 98% and 100%, respectively, at 7 years. Keisu et al.2 found a survival rate of 100% for both components at 5 years. Using cementless prostheses in younger patients, 65 years or older, Engh et al.20 reported a survival rate of 98% for the prosthesis at 8 years, and McAuley et al.29 reported 92% at 12 years. Ogino et al.7 carried out a descriptive study of the Finnish registry of arthroplasties, finding 6989 registered THA implants in patients older than 80 years between 1980 and 2004. Of this sample, there was some information regarding 195 (2.8%) that resulted in revision due to failure, the principal causes being aseptic weakening (1.2%), recurrent dislocation (0.5%), periprosthetic fracture (0.3%), and deep infection (0.3%). However, no data were provided as to the initial diagnosis or the type of fixation used in the primary prosthesis in which the failure occurred. According to those data, they found that the survival rate for the prosthesis at 5 years after using hybrid fixation was 98%, 97% for cemented, and 96% for cementless; although they reported no significant difference between the latter 2 types, there was a significant difference between the hybrids and the cementless. They therefore recommended using cemented stems for patients with advanced age. However, the study presented significant weaknesses in our opinion, as the data available were limited and incomplete. Furthermore, 392 different prosthetic systems were used in the study, and 30% of the procedures were done with prostheses designed at least 20 years ago.
In our study, the mean score increase among the octogenarians, between pre- and postoperative scores, was 6 points on the Merle d’Aubigné scale and 52 points on the Harris scale. All of the octogenarians, except for 2, had excellent or good results, which was similar to the control group. In our study, this demonstrated the efficacy of cementless prostheses in patients in this age range. Other authors reported similar increases on the hip function scales for octogenarians with cementless prostheses.2,8,9 Several authors30,31 found no differences in incidence of anterior thigh pain from using cementless stems or cemented ones in elderly patients,. With cemented THA in octogenarians, a recent study32 reported a 48% rate of satisfactory results after a mean follow-up of 2.5 years, finding that regular and poor function results were associated with concomitant affectation of other joints.
In our study, cementless total hip arthroplasty was shown to be safe and effective in octogenarian patients with coxarthrosis, with a component survival rate similar to that in younger patients. The notable increase found in functional results justifies the continued use of cementless prostheses in patients with advanced age.
Ethical responsibilitiesHuman and animal protectionThe authors declare that no experiments were carried out on humans or animals for this study.
Data confidentialityThe authors declare that they followed the protocols of their work center regarding publication of patient data, and that all patients included in the study received sufficient information and gave their informed consent in writing to participate in the study.
Right to privacy and informed consentThe authors declare that this article does not present any patient data.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Lizaur-Utrilla A, Sanz-Reig J. Artroplastia total de cadera primaria electiva no cementada en octogenarios. Estudio de caso-control. Rev Esp Cir Ortop Traumatol. 2013;57:186–93.