Diaphyseal fractures of the forearm comprise 6%–10% of all fractures in children. The treatment depends on the age and type of displacement, and conservative and surgical management with fixation of intramedullary nails, among other techniques, is valid. The aim is to show the radiological and functional outcomes, and complications of intramedullary fixation with Kirschner nails in children.
Materials and methodsA retrospective descriptive case series of patients treated with intramedullary fixation of forearm fractures. The radiological and functional results, and complications are correlated.
ResultsOf the 117 patients operated, 59 met the inclusion criteria. The average age was 10 years. Eighty-four point seven percent were males and the left side was the most affected (62.7%). In 88.1% both bones were fractured and 11 cases had open fractures. An open reduction was performed in 72.8% of the cases, the main indications for this being instability, failed reduction and refracture. There were 52 excellent outcomes, 2 good, and 4 regular and 1 bad. There were 13.5% minor complications.
DiscussionThis study shows that intramedullary fixation with Kirschner nails in radius and ulna diaphysis fractures in children is a safe, low-cost procedure and offers adequate short and medium term functional outcomes, with a low prevalence of serious complications with only 6 cases of non-consolidation and refracture. Larger preoperative angulations in the anteroposterior and lateral planes, and lateral postoperative angulations, could be considered predictors of less satisfactory functional results.
Las fracturas diafisarias del antebrazo constituyen el 6-10% de todas las fracturas en niños. El tratamiento depende de la edad y el tipo de desplazamiento y son válidos el manejo conservador y quirúrgico con fijación de clavos intramedulares entre otros. El objetivo es mostrar los resultados radiológicos y funcionales, y las complicaciones de la fijación intramedular con clavos de Kirschner en niños.
Materiales y métodosEs una serie de casos retrospectiva descriptiva de pacientes operados con fijación intramedular de fracturas de antebrazo. Se correlacionan los resultados radiológicos y funcionales y las complicaciones.
ResultadosDe 117 pacientes operados, 59 cumplían criterios de inclusión. La edad promedio fue 10 años. El 84,7% de ellos fueron hombres y el izquierdo el lado más afectado (62,7%). El 88,1% de ambos huesos estaban fracturados y 11 casos tenían fracturas abiertas. Se realizó reducción abierta en el 72,8% de los casos cuyas principales indicaciones fueron inestabilidad, reducción fallida y refractura. Se tuvieron 52 resultados excelentes, 2 buenos, 4 regulares y uno malo. Hubo un 13,5% de complicaciones menores.
DiscusiónEste estudio muestra que la fijación intramedular con clavos de Kirschner en fracturas de diáfisis de radio y cúbito de niños es un procedimiento seguro, de bajo costo y que ofrece a corto y mediano plazo adecuados resultados funcionales, con una prevalencia baja de complicaciones graves, con solo 6 casos de no consolidación y refracturas. Las angulaciones preoperatorias mayores en los planos anteroposterior y lateral, y angulaciones posoperatorias en el plano lateral, podrían considerarse predictores de resultados funcionales menos satisfactorios.
Fractures of the radius and ulna are the third most common fractures in children and constitute 13%–40% of all fractures.1,2 Historically, most of these fractures were treated conservatively or orthopaedically. There has been a tendency recently towards surgical treatment in an effort to improve results.3 Treatment depends on the child's age and type of fracture displacement, among other factors. Bearing in mind a child's physeal growth potential, some degree of angulation can be accepted depending on the age of the child and their remodelling capacity.
Immobilisation of the forearm with splints or circular casts is still a treatment option for many fractures that are within acceptable alignment parameters. Surgical treatment is recommended for fracture lines that do not meet these parameters.3,4 The surgical options include fixation with plates or with intermedullary nails. There has been growing interest lately in establishing the treatment that provides the best outcomes, but there remains debate as to the optimal treatment.4,5
It is common in our environment to see diaphyseal fractures of the radius and ulna treated with intramedullary Kirschner wire fixation. Some reports endorse this technique.3–5 The objective of this study was to review the indications, and clinical and radiological outcomes in a series of children treated with intramedullary Kirschner wire fixation for diaphyseal fractures of the forearm.
Material and methodsA retrospective, descriptive case series of patient treated with intramedullary fixation for fractures of the radius and/or ulna, from 2009 to 2014. Skeletally immature patients and patients with diaphyseal fractures to the radius and/or ulna, treated surgically with closed and/or open reduction and intramedullary Kirschner wire fixation, with a minimum follow-up of 6 months, were included in the study. Skeletally mature patients, distal and proximal fractures of the radius and/or ulna (metaphyseal, Moneggia and Galeazzi fractures), those who were treated surgically with closed and/or open reduction with intramedullary fixation using elastic nails or plates, and those treated in a different institution were excluded.
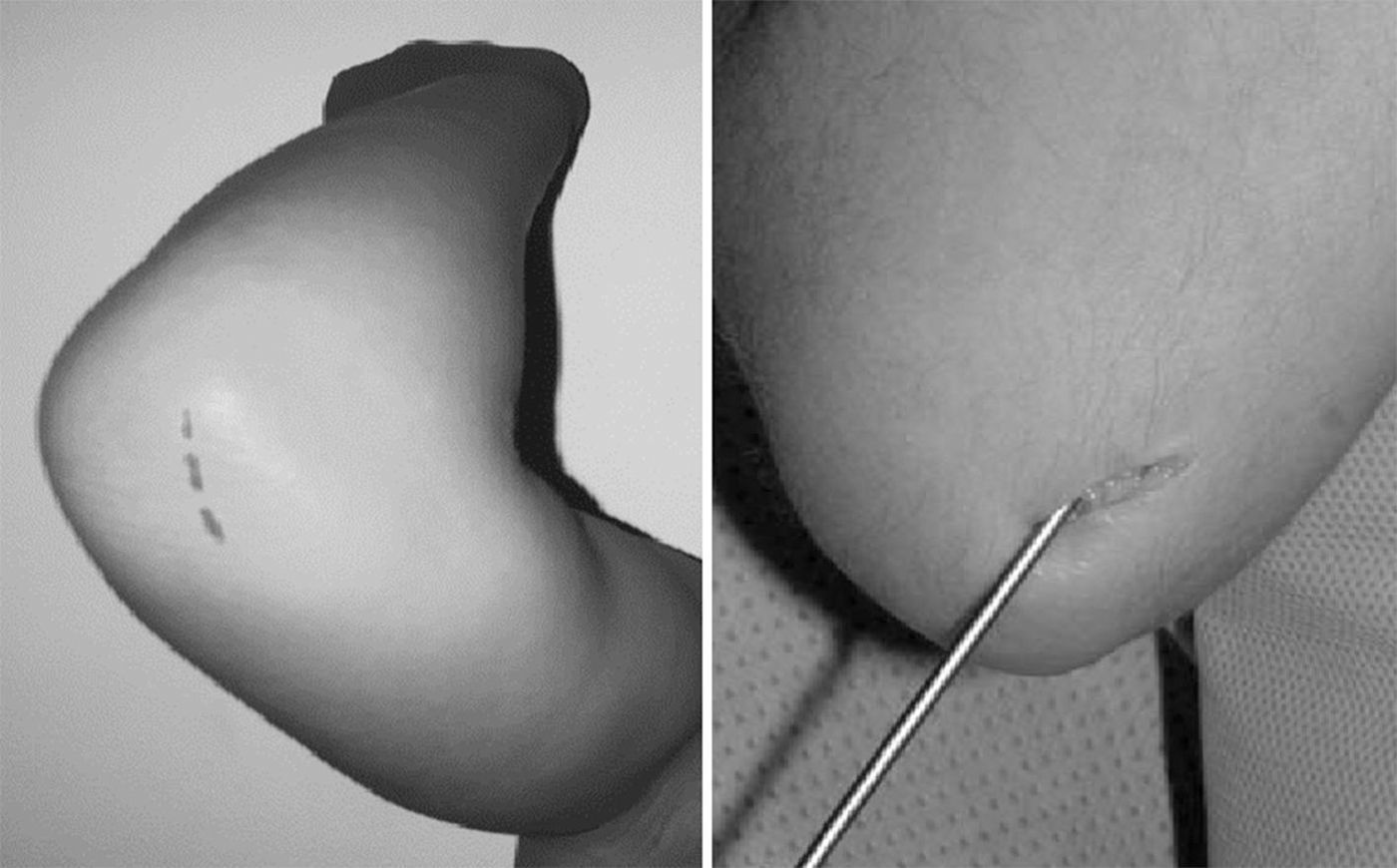
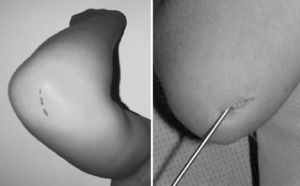
The data were collected from clinical histories. Pre- and postoperative X-rays (Fig. 1) were measured. The demographic variables, displacement and initial angulation of the fracture and displacement and final angulation of the fracture, Gustilo-Anderson for open fractures, type of surgical technique, duration of intramedullary wire fixation, type and duration of external immobilisation, duration of follow-up, range of motion at final follow-up, time to union of each bone, and complications were recorded with a goniometer. The clinical outcomes were assessed using the scale developed by Price et al.,6 described for orthopaedic treatment, which can be extrapolated for patients undergoing surgical treatment, with outcomes considered as follows: excellent, for no symptoms on strenuous physical activity and/or pronosupination loss <10°; good, for mild symptoms on vigorous activity and/or 11°–30° loss in forearm rotation; fair, for symptoms during daily activities or rotation loss of 31°–90°, and poor, for all other outcomes with a pronosupination loss >90°. The comparison was made with the unaffected forearm (Fig. 2).
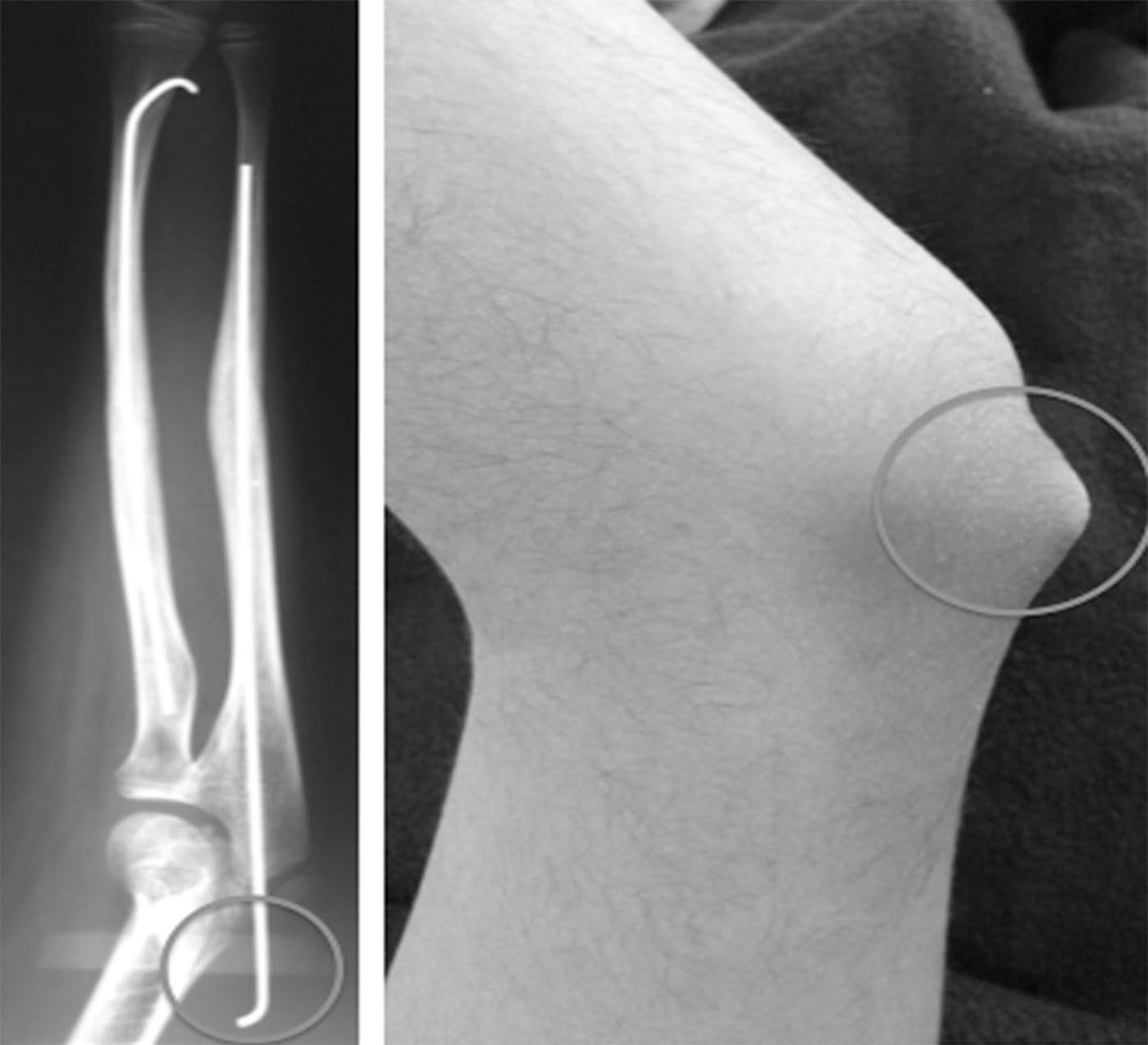
Within the technical details of the surgery,7,8 the radius is fixed retrogradely with a wire of an appropriate diameter and advanced through a hole made proximal to the distal physis of the radius (Fig. 3). The ulnar fracture is fixed with a wire that is inserted in an anterograde fashion through the olecranon (Fig. 4). The tip of the radial wire should be inclined approximately 15°–30° to enable passage through the medullary cavity. The length of the wire is measured under an image intensifier. The diameter of the Kirschner wire ranges from 1.5 to 2mm, depending on the diameter of the medullary cavity. If the manoeuvre is not possible with closed reduction under image intensifier, it is performed open with a minimal incision and fluoroscopic control. The ends of the wire are left under the skin.
At the end of the operation, a sugar-tong plaster splint is placed to protect the forearm for 4–6 weeks, at this time free movement of the elbow and wrist is started, occasionally assisted with physiotherapy.
The data were analysed using Social Sciences statistical software (SPSS version 15, Chicago, Illinois, U.S.A.). A multivariate analysis was performed to study the associations between the variables. A p value <.05 was selected as significant.
The paper was approved by the ethics committee of the university heading the study.
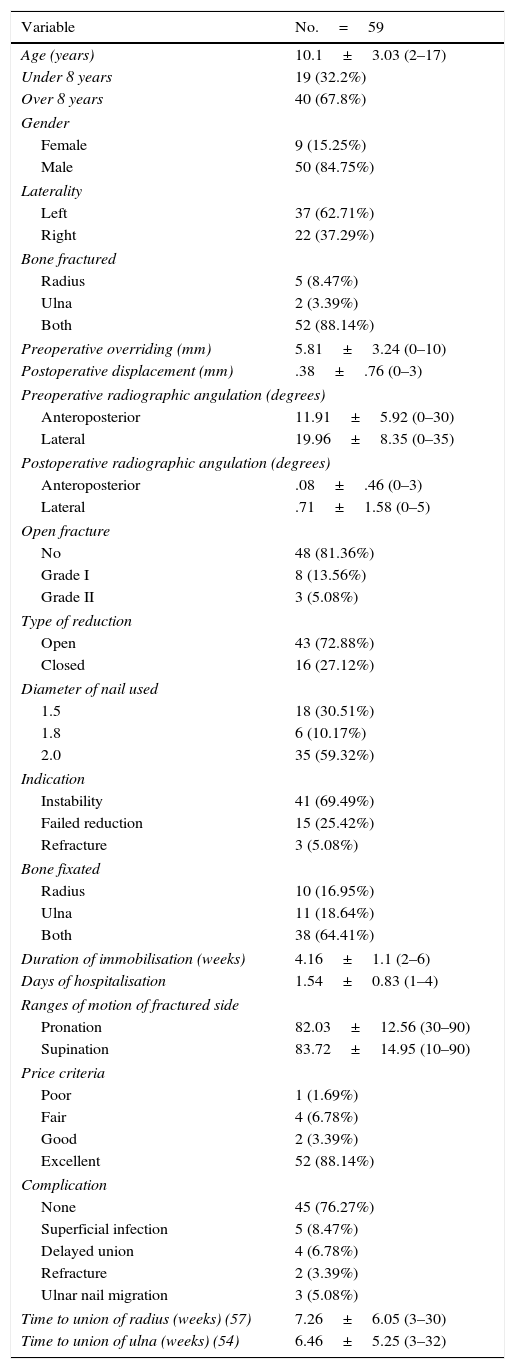
ResultsWe found 1877 patients who presented with forearm fractures, during the period 2009–2014. A total of 117 were treated surgically for diaphyseal fractures of the radius and/or ulna. Of these, 59 patients (50 males and 9 females) met the inclusion criteria (Table 1). The sample was aged between 2 and 17 years (mean±standard deviation of 10.1±3.03). Twenty-two patients (37.2%) had a fracture to the right forearm, and 37 (62.7%) to the left.
Characterisation of variables.
| Variable | No.=59 |
|---|---|
| Age (years) | 10.1±3.03 (2–17) |
| Under 8 years | 19 (32.2%) |
| Over 8 years | 40 (67.8%) |
| Gender | |
| Female | 9 (15.25%) |
| Male | 50 (84.75%) |
| Laterality | |
| Left | 37 (62.71%) |
| Right | 22 (37.29%) |
| Bone fractured | |
| Radius | 5 (8.47%) |
| Ulna | 2 (3.39%) |
| Both | 52 (88.14%) |
| Preoperative overriding (mm) | 5.81±3.24 (0–10) |
| Postoperative displacement (mm) | .38±.76 (0–3) |
| Preoperative radiographic angulation (degrees) | |
| Anteroposterior | 11.91±5.92 (0–30) |
| Lateral | 19.96±8.35 (0–35) |
| Postoperative radiographic angulation (degrees) | |
| Anteroposterior | .08±.46 (0–3) |
| Lateral | .71±1.58 (0–5) |
| Open fracture | |
| No | 48 (81.36%) |
| Grade I | 8 (13.56%) |
| Grade II | 3 (5.08%) |
| Type of reduction | |
| Open | 43 (72.88%) |
| Closed | 16 (27.12%) |
| Diameter of nail used | |
| 1.5 | 18 (30.51%) |
| 1.8 | 6 (10.17%) |
| 2.0 | 35 (59.32%) |
| Indication | |
| Instability | 41 (69.49%) |
| Failed reduction | 15 (25.42%) |
| Refracture | 3 (5.08%) |
| Bone fixated | |
| Radius | 10 (16.95%) |
| Ulna | 11 (18.64%) |
| Both | 38 (64.41%) |
| Duration of immobilisation (weeks) | 4.16±1.1 (2–6) |
| Days of hospitalisation | 1.54±0.83 (1–4) |
| Ranges of motion of fractured side | |
| Pronation | 82.03±12.56 (30–90) |
| Supination | 83.72±14.95 (10–90) |
| Price criteria | |
| Poor | 1 (1.69%) |
| Fair | 4 (6.78%) |
| Good | 2 (3.39%) |
| Excellent | 52 (88.14%) |
| Complication | |
| None | 45 (76.27%) |
| Superficial infection | 5 (8.47%) |
| Delayed union | 4 (6.78%) |
| Refracture | 2 (3.39%) |
| Ulnar nail migration | 3 (5.08%) |
| Time to union of radius (weeks) (57) | 7.26±6.05 (3–30) |
| Time to union of ulna (weeks) (54) | 6.46±5.25 (3–32) |
Forty-three patients (72.8%) required open reduction after attempts at closed reduction. The others were treated with the closed technique. Follow-up was an average 23 months (between 9 and 72 months). The time to union of the fracture, defined as the presence of callus visible on anteroposterior and lateral X-rays during radiological follow-up, was 7.2 weeks on average for the radius (interval of 3–30), and 6.4 weeks for the ulna (interval of 3–32).
The results according to Price's criteria were excellent in 52 patients (88.1%), good in 2 patients (3.3%), fair in 4 (6.7%), and poor in 1 (1.6%). The patient with the poor result had 40° pronation and 70° supination. The average immobilisation after the operation was 4.1 weeks and the osteosynthesis material was removed between 2 and 21 months (mean 6.5±4) (Fig. 5).
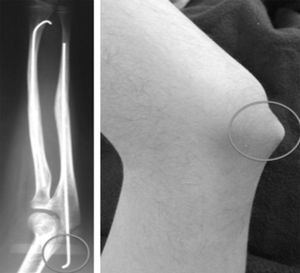
Eight patients (13.5%) had minor complications, such as superficial infection on the skin of the olecranon (5 patients) and external migration of the ulnar nail (3 patients) (Fig. 6). The cases of superficial infection were treated with oral antibiotics, without additional complications. Six patients (10.1%) had complication such as delayed union and refracture. Complications such as physeal injury, angular or rotational deformity, synostosis, nerve damage, compartment syndrome, deep infection or restricted movement of the elbow were not encountered.
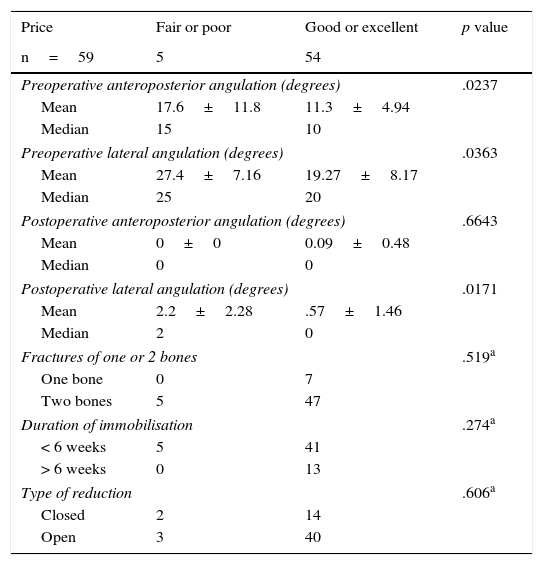
Multivariate analysis of radiological angulation and functional outcomes (Table 2): the associations between the angulation in both planes of the fracture lines both before and after surgical treatment were studied. To that end, the patients were put into groups of excellent and good results as the ideal outcome, and the others with fair and poor results grouped as the opposite outcome.
Functional results. Preoperative angulations behave as a normal angulation therefore the Student's t-test was performed.
| Price | Fair or poor | Good or excellent | p value |
|---|---|---|---|
| n=59 | 5 | 54 | |
| Preoperative anteroposterior angulation (degrees) | .0237 | ||
| Mean | 17.6±11.8 | 11.3±4.94 | |
| Median | 15 | 10 | |
| Preoperative lateral angulation (degrees) | .0363 | ||
| Mean | 27.4±7.16 | 19.27±8.17 | |
| Median | 25 | 20 | |
| Postoperative anteroposterior angulation (degrees) | .6643 | ||
| Mean | 0±0 | 0.09±0.48 | |
| Median | 0 | 0 | |
| Postoperative lateral angulation (degrees) | .0171 | ||
| Mean | 2.2±2.28 | .57±1.46 | |
| Median | 2 | 0 | |
| Fractures of one or 2 bones | .519a | ||
| One bone | 0 | 7 | |
| Two bones | 5 | 47 | |
| Duration of immobilisation | .274a | ||
| < 6 weeks | 5 | 41 | |
| > 6 weeks | 0 | 13 | |
| Type of reduction | .606a | ||
| Closed | 2 | 14 | |
| Open | 3 | 40 | |
Given that postoperative angulations did not distribute according to the normal curve, a non-parametric test was required (Mann–Whitney U test).
Statistically significant differences were found in the case of preoperative anteroposterior angulation (p=.0237), where the greater the patient's angulation, the poorer their functional outcome. Likewise, for preoperative (p=.0363) and postoperative (p=.0701) lateral plane angulations.
All of the patients who underwent intramedullary fixation of only one bone of the forearm had good or excellent functional outcomes, and those who underwent fixation of both forearm bones had less favourable outcomes (90.38%). However, this difference was not notably significant (p=.519).
When the association was analysed between immobilisation time, patients and functional outcome at the end of the treatment, no significant difference was found (p=.274) between those who were immobilised for less than 6 weeks and those immobilised for longer.
The association of open or closed reduction for fixation with the functional outcome at the end of treatment was studied, but no statistically significant difference was found between either group (p=.606).
In total there were 11 reports of open fractures. In turn, 5 cases of superficial infection were recorded. A statistically significant relationship was found between grade IIopen fractures and the onset of infection (p=.006). It was clarified that the infections were superficial at the entry point of the ulnar wire.
No statistically significant relationship was found (p=.118) between the 5 cases of superficial infection and the type of reduction used.
Four cases of delayed union were reported. When these cases were related with the type of reduction, no difference was found in their proportion or in the significance of their association (p=.705).
DiscussionMost fractures of the forearm in paediatric patients can be treated orthopaedically by closed reduction and appropriate imobilisation.3,9–11 Those that occur in the middle and proximal third of the diaphysis do not remodel in a predictable fashion and therefore require more anatomical reduction.11 There is some controversy as to how much angulation, displacement and rotation constitutes an acceptable reduction. Young patients can tolerate deformity more than older children.9,10 Several authors have indicated that reduction is not acceptable if the patient has an angulation greater than 10° or complete displacement.3,9 Parameters exist for accepting poor rotational alignment up to 45°, but some authors have indicated that remodelling of rotation is not as efficient.9,12,13
Sinikumpu et al. recommend surgical intervention for diaphyseal fractures of the forearm with angulations greater than 10°, because potential remodelling is limited in this area of the bone and its residual deformities affect movement of the forearm.14 Mathews et al. demonstrated in cadavers that angular deformities of the forearm of 10° do not result in significant loss of pronosupination, but that an amount of 20° will restrict rotation of the forearm by approximately 30%.12 Another study in cadavers showed that an angulation of only 5°, located in the mid shaft of the forearm, might lead to a pronation loss of up to 27%.15
When indicated, surgical fixation of these fractures in children is effective, irrespective of the method used,1,3–5,9,16,17 flexible intramedullary fixation being the preferred method.18–20 Most studies show good to excellent results using this method. Flexible wires are expensive and are not readily available in most hospitals. In this study, we obtained good functional outcomes with Kirschner wires, as elastic nailing, with 91% excellent and good outcomes, comparable with similar studies. This technique was first described by Pérez Sicilia et al. in 1977.3,9,21–24
Yalcinkaya et al., in 45 cases assessed using Price's criteria, found excellent and good results in all of the patients.13 Shoemaker et al., in a group o f32 patients treated exclusively with Kirschner wires, obtained good and excellent results in 100%.25 Parajuli et al. had excellent and good outcomes in all their patients.15 Altay et al., reported excellent functional outcomes in 96% of 48 patients.26
Because Kirschner wires are less malleable, the tip is more difficult to insert, compared to titanium nails.
Similar functional outcomes have been reported for patients who underwent closed or open reduction before intramedullary fixation,13,27,28 with a similar profile of complications as well. In this study, 43 patients required open reduction due to soft tissue interposition and in the majority of these the functional results were excellent or good. Moreover, there was no statistical difference between this group and the closed reduction group.
The complications in this study were comparable to those of other studies. Flynn et al. demonstrated a 14.6% overall complication rate in patients who underwent intramedullary fixation.3 The most common complications were: delayed consolidation, compartment syndrome, infection, skin irritation caused by the osteosynthesis material and migration of same. Yalcinkaya et al. encountered minor complications in 4.44% of their patients.13 Shoemaker et al. had major complications in 2 patients.25 Parajuli et al. encountered 16% minor complications.15 Altay et al. reported 22% minor complications, and 8% highly complex complications.26
In our series, we found minor complications in 13.55% of the cases (5 superficial infections and 3 migrations of the wire, both in the olecranon). There were 2 patients with refracture (3.3% of the cases). Although this complication is rarely reported in the literature, van Egmond et al. record an occurrence of 2.3%.22 No pseudoarthrosis occurred, but there were 4 cases of delayed consolidation, with no statistical difference between the closed and open reduction groups. Flynn et al. reported that in patients over 10 years of age delayed union was more common, and required surgical reintervention,3 and they had poorer functional outcomes. We found no statistical difference in terms of functional outcomes according to the age groups above and below 8 years in our study.
Loss of rotation of the forearm is reported with this technique, principally pronation. In our study the average motions were 82±12.5° and 83.7±14.9° pronation and supination respectively, and 54 patients had excellent and good outcomes (91.5%).
Studies show that a loss of reduction and residual deformities affect the function of the forearm.13,17 We report statistically significant differences in the functional outcomes of the patients with preoperative angulations greater than 17° in the anteroposterior plane and greater than 27° in the lateral plane, which could be considered predictors of less satisfactory functional outcomes. Likewise for patients with postoperative angulations in the lateral plane as small as 2°, although an error factor to consider is the probable manipulation of the forearm before admission of the patient or while the X-rays were taken.
When we examined the impact on functional results if one or both bones were fractured and fixated, no representative differences were found, or when immobilisation periods of more than 6 weeks were compared.
Some authors state that pseudoarthrosis is a very rare complication in intramedullary fixation with flexible wires in the bones of the forearm, and suggest open fractures, open reduction, refracture, hypotrophic consolidation callus formation, fracture of the middle diaphyseal third, unstable osteosynthesis, premature removal of the osteosynthesis material and infection as predisposing factors.16,21,23
When open reduction and internal fixation with plates are compared, no differences are found in the onset of complications.21,29 And when Kirschner wires are compared with elastic nails, the clinical and functional outcomes and the complications rate are also similar, despite the methodological weaknesses of this type of study.
As mentioned earlier, an open reduction technique is considered a predictor for delayed union. In a case and control study, open reduction was found to be the most significant predictor for delayed union, reporting a statistically significant association.9 We found no statistical difference between either group in this study.
Another concern regarding the technique used in these cases is that the nails are placed crossing the distal physis of the radius and proximal physis of the ulna. Yung et al. recorded no alterations in the growth plate in any of the forearm bones in 84 patients.30 With a reproducible technique, which almost always crossed the physis of the olecranon tip, we recorded no growth alterations in our study either. There were no vicious unions or deep infections. No significant differences were found between onset of infection and open fractures.
This study has several limitations. It is a retrospective study where the study group was treated by various surgeons within a certain period, therefore, decision-making and criteria might have varied according to each surgeon.
ConclusionsWhen indicated, intramedullary fixation with Kirschner wires of displaced and unstable forearm fractures in children provides good radiological and functional outcomes. It is a minimally invasive procedure, with good biological and cosmetic outcomes. Kirschner wires are affordable and readily available in most hospitals.
The complications encountered were minor, generally did not affect the final outcome and are comparable with other studies. Larger preoperative angulations in the anteroposterior and lateral planes, and postoperative angulations in the lateral plane, could be considered predictors of less satisfactory functional outcomes.
Level of evidenceLevel of evidence iv.
Ethical disclosuresProtection of people and animalsThe authors declare that the research was carried out according to the ethical standards set by the responsible human experimentation committee, the World Medical Association and the Helsinki Declaration
Data confidentialityThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mahecha-Toro M, Vergara-Amador E, González Ramírez M. Fracturas diafisarias del antebrazo en niños: tratamiento con fijación intramedular con clavos de Kirschner. Rev Esp Cir Ortop Traumatol. 2018;62:71–79.