Intracraneal bleeding is a rare complication after raquis surgery. It is believed to occur as a drop in the intracraneal pressure after a loss of CSF secondary to an iatrogenic dural tear. We report a patient who after surgery for lumbar stenosis presented a subarachnoid haemorrhage, an intraparenchymal haematoma, and a subdural haematoma. To our knowledge, this is the first report in the literature with such complications after this type of surgery.
La hemorragia intracraneal es una complicación poco frecuente tras la cirugía de raquis lumbar. Se cree que esta complicación se produce por una caída en la presión intracraneal tras una pérdida de líquido cefalorraquídeo a través de una brecha dural iatrogénica. Presentamos el caso clínico de una paciente que presentó una hemorragia subaracnoidea, un hematoma intraparenquimatoso y un hematoma subdural tras una intervención de estenosis de canal lumbar. No hemos encontrado en la literatura revisada sobre el tema ningún caso que presente tal asociación hemorrágica tras una cirugía de este tipo.
The most frequent complications of spinal surgery are local. They include injury to a nerve root, a visceral injury or durotomies that may be associated with the loss of cerebrospinal fluid (CSF). Another complication described as the result of the loss of CSF is intracranial bleeding. We present a case of intracerebral, subdural and subarachnoid bleeding in a patient operated for lumbar stenosis. To date this would be the first published case of the said association between haemorrhaging and lumber surgery.
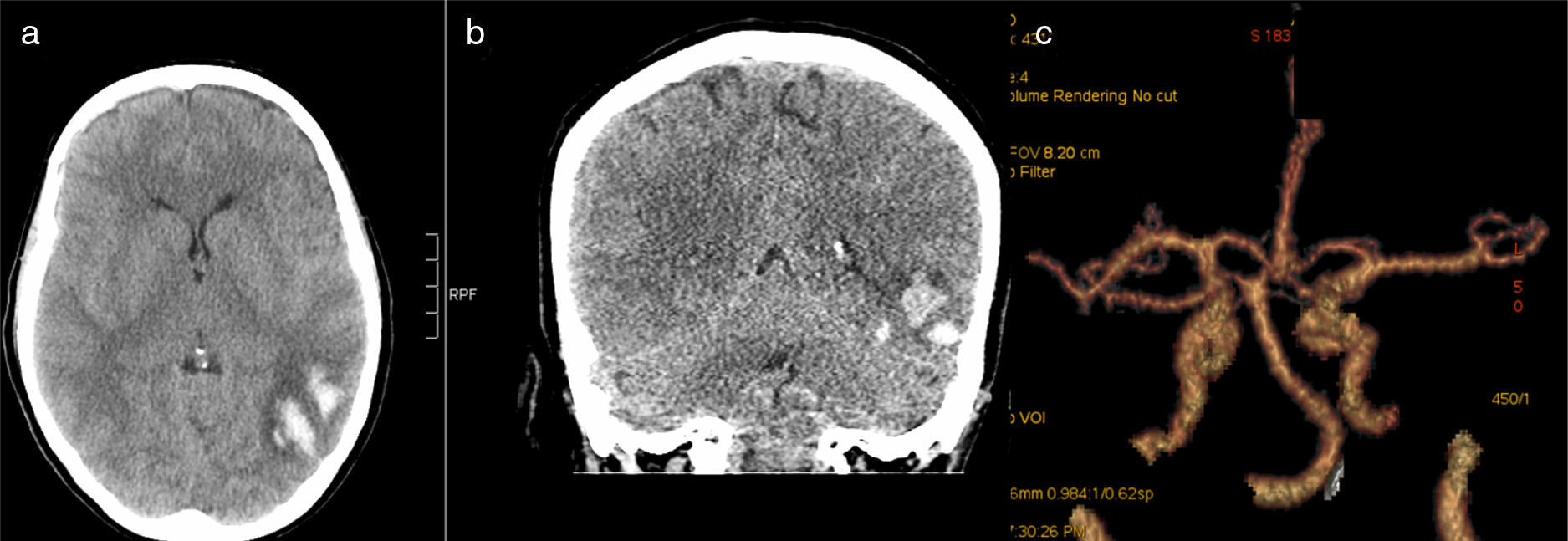
Material and methodsA 67 year-old female patient presented 9/10 analogue visual scale lumbar pain and bilateral radicular pain when resting in the area of L4–L5 accompanied by neurogenic claudication at 10m. Diagnosis by magnetic resonance imaging was lumbar stenosis at the level of L3–L4, L4–L5 and L5–S1, with grade 1 spondylolisthesis at L4–L5. Following months of conservative treatment that included invasive pain therapy it was decided to perform surgery. A laminectomy was performed at levels L3–L4 and L4–L5, with posterolateral arthrodesis at L3–L4, L4–L5, leaving suction drainage in the subfascial plane. Surgery was carried out apparently without complications, although after the operation the patient had a prolonged waking from the anaesthesia. During her stay in the post-anaesthesia recovery ward the tendency to sleep continued and she only responded to a painful stimulus. 2h after surgery she suffered a generalised grand mal seizure, due to which an urgent cranial CAT was performed. This showed a left temporal intracerebral haemorrhage and 2 foci of apparently subarachnoid bleeding in the right side, one in the occipital zone and the other in the frontal zone (Fig. 1a and b). A vascular study was undertaken by computed tomography angiography to rule out an arterial malformation in the base of the cranium as the cause of the bleeding (Fig. 1c). At this moment the drainage was withdrawn with a loss of approximately 300cc of haematic appearance.
(a, b) Postoperative cerebral CAT showing left posterior intra-axial haemorrhage with several hyperdense foci compatible with acute haemorrhage. It is accompanied by haematic occupation of a left temporal sulcus, the left posterior wall and right temporal fossa compatible with SAH. Right frontal laminar an extra-axial haematic accumulation, giving rise to the differential diagnosis between a subdural laminar haematoma and an extension of the SAH. (c) Angio CAT imaging performed after the operation ruled out malformations in the Willis polygon as the cause of bleeding.
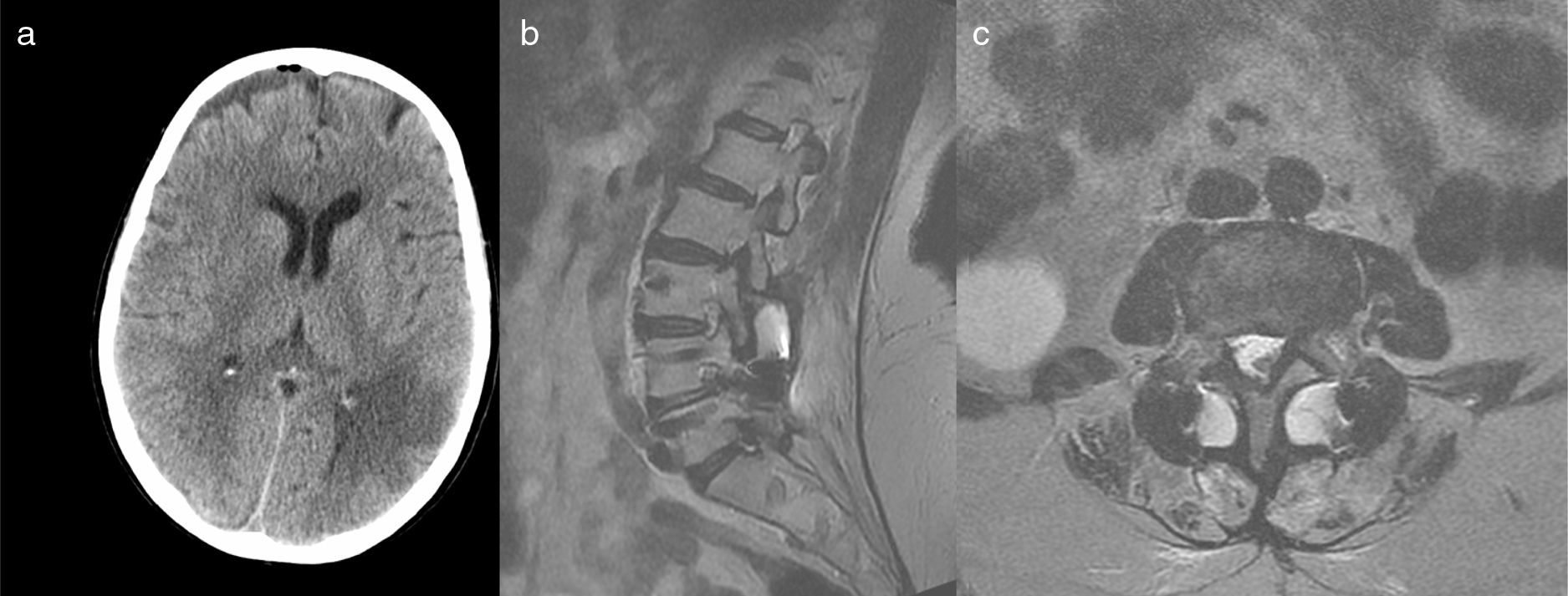
Due to this complication the patient remained in the intensive care unit for the following days with intracranial pressure monitoring, spontaneous respiration and normal blood pressure. Although she was in a stupor for the first 24h after the operation she gradually recovered her level of consciousness without any further complications. In neurological examination 2 weeks after surgery the patient had recovered her habitual level of consciousness and presented the symptoms of predominantly right tetraparesia and speech alterations. Imaging tests were conducted at this moment, confirming that the frontal focus of haemorrhaging corresponded to a small frontal subdural haematoma with slight pneumocephalus (Fig. 2a). The patient was seen regularly as an outpatient after the first month to continue with postoperative check-ups. At 6 months a new lumbar magnetic resonance imaging study was performed, showing a small pseudomeningocele at the level of the surgery (Fig. 2b and c).
ResultsThe patient is currently undergoing rehabilitation, and the neurological deficits she suffered are evolving favourably. Her lumbar pain has improved and now scores 2/10 on the visual analogue scale. The irradiating pain when resting has disappeared, as has the neurogenic claudication. Except for the neurological complication the patient is satisfied with the result of the surgery.
DiscussionIntracranial haemorrhage following lumbar spinal surgery is not a frequent event. In a review Pham et al.1 found an incidence of 0.4% for complications of this type. Similarly Khalatbari et al.2 found 4 cases among 1077 patients. The most widely accepted cause to explain this severe complication is the production of intracranial hypertension as the result of loss of CSF through a dural injury, giving rise to herniation of the cephalic mass and bleeding from vessels due to traction and breakage.3–6 The majority of cases described presented cerebral and subdural bleeding, while intracerebral bleeding was rare. The typical pattern of cerebral bleeding visible in tests has been denominated the zebra sign.5–7
No injury to the dura mater was detected in our patient during surgery, although magnetic resonance imaging carried out 6 months after surgery showed the existence of a pseudomeningocele at the level of the operation. This leads to the suspicion that there was accidental durotomy with secondary loss of CSF that went unnoticed during the operation. Accidental durotomies are one of the complications described in lumbar spinal surgery.7 It is possible that a slight and unnoticed loss of CSF during surgery becomes larger following the positioning of suction drainage, thereby causing significant intracranial hypotension.3,6 We believe that this may have occurred in our patient, giving rise to the described complication.
The habitual symptom following intracranial hypotension is intense cephalea which starts 24–48h after the injury occurs, and which worsens when standing. It is often accompanied by nausea and vomiting. The clinical symptoms are usually self-limiting and cease after a few days of bed rest.
After an episode of intracranial bleeding the clinical signs usually commence swiftly, during the first 10h, with signs of neurological deficits,2,6,7 as we saw in our case. In a patient who has been subjected to surgery the symptoms of a neurological deficit may go unnoticed in the initial phase. Instead of these symptoms the patient may display difficulty in waking up from the anaesthetic, cephalea, dizziness and vomiting. In agreement with Kaloostian et al.8 we believe that the anaesthesia itself together with opiate analgesia, if used in an operation of this type, may cause similar adverse effects. Due to this, special attention must be paid in the differential diagnosis of patients subjected to spinal surgery who display the said symptoms, more so if any injury to the dura mater was noticed during the operation.
The usual risk factors for non-traumatic intracranial haemorrhage, such as hypertension and anticoagulants among others, are considered to be potential causes of postoperative bleeding.5–7 Although our patient had no risk factors for haemorrhage, older patients with lumbar spinal stenosis and advanced arthrosis of the lumbar facets (conditions which were present in our patient) are at greater risk according to Floman et al.7 of suffering a dural injury during surgery, and consequently a loss of CSF. The risk of accidental durotomy varies from 3.1% to 14%.6,7 Other causes of intracranial bleeding, such as vascular malformation of the Willis polygon, can be ruled out by CAT after surgery (Fig. 1c).
Some authors consider Intraoperative losses of CSF or ones through drainage to be the main risk factor for intracranial complications.1–3,6 Kaloostian et al.8 found a certain degree of association between the amount of loss through the drainage and cranial haemorrhaging complications. A risk factor for such complications is the daily postoperative loss of more than 221ml of serohaematic fluid through the drainage, even when no losses were detected during surgery. Intracranial haemorrhaging complications have also been reported following lumber puncture for spinal anaesthesia.3,4,8,9
The majority of intracranial bleeding cases described following spinal surgery tend to be cerebral and subdural haemorrhages. Intraparenchymal haemorrhaging5,8 such as we describe in this paper occurs less frequently. Although our patient also had a small pneumocephalus, we cannot be sure that this was connected with the surgery, as air may have entered the subarachnoid space during the insertion or withdrawal of the intracranial pressure detector. Additionally, in the literature that was reviewed we found only one description of a case of pneumocephalus as a complication of spinal surgery, so we therefore believe it be a rare event.10 We found no other possible cause of pneumocephalus, given that at the time of surgery anaesthetic epidural catheters were not used according to protocol in our hospital, nor were any other techniques that could have injured the dura mater.
We agree with Hempelman y Mater4 that asymptomatic cases of intracranial bleeding may exist, or ones with few symptoms such as cephalea or dizziness, so that given the lack of more striking suspicious symptoms no imaging tests are performed so that the lesion goes unnoticed. This condition may therefore be under-diagnosed and occur more frequently that is believed. This does not seem to justify the use of imaging tests in all patients operated to rule out postoperative intracranial bleeding.1,4,7,8 We believe this to be the first published case to date that associates the said haemorrhaging complications with previous surgery for lumbar stenosis.
ConclusionIntracranial haemorrhage is a complication which may arise following spinal surgery, especially if there was also dural injury. If a patient displays unexpected neurological deterioration after surgery of this type, this should not be attributed solely to intracranial hypotension caused by CSF loss. The possibility of intracranial bleeding must be considered, and imaging tests should be performed for diagnosis. Swift diagnosis may help to ensure early treatment and avoid possible consequences.
Level of evidenceLevel of evidence V.
Ethical disclosuresProtection of people and animalsThe authors declare that for this research no experiments were performed on human beings or animals.
Data confidentialityThe authors declare that they followed the protocols of their centre of work for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
FinancingThis work received no financing whatsoever.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sierra JJ, Malillos M. Complicación intracraneal tras cirugía de raquis lumbar. Rev Esp Cir Ortop Traumatol. 2018;62:153–156.