The sensory innervation of the hip joint is complex. The joint and sensory branch block of the obturator and femoral nerves is effective for treating the pain caused due to different hip diseases. This could be an option to be considered in certain circumstances such as, being a surgical-anesthetic high risk, or if there is significant overweight. It could also be useful on other occasions if the traumatoligist considers that it is better to delay hip replacement for a limited period.
La inervación sensitiva de la articulación de la cadera es compleja. El bloqueo intraarticular y de las ramas sensitivas de los nervios obturador y femoral es eficaz para tratar el dolor producido por diversas enfermedades de cadera, y pudiera ser una opción a considerar en determinadas circunstancias. Estas circunstancias pueden ser alto riesgo quirúrgico-anestésico por el estado basal del paciente o la existencia de sobrepeso importante, en otras ocasiones el médico traumatólogo considera que es mejor retrasar la artroplastia, al menos durante algún tiempo.
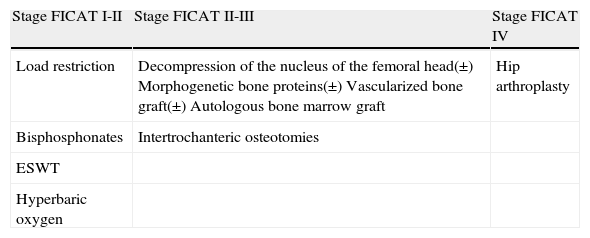
Avascular necrosis of the femoral head (ANFH) has a multifactorial etiology. It mainly affects young populations and, if not addressed timely, can lead to femoral head collapse, which will eventually entail a hip arthroplasty. Although early presentation can be painless, pain is common at later stages and can even limit active and passive hip movement. Femoral head irrigation comes mainly from the extraosseous systems of the circumflex and retinacular arteries.1 However, there is additional, less important vascularization, such as that originating from the round ligament artery. There are multiple treatment options2 which vary according to the stage of ANFH (Table 1).
Summary of the main treatments accepted for a vascular osteonecrosis of the femoral head.
| Stage FICAT I-II | Stage FICAT II-III | Stage FICAT IV |
| Load restriction | Decompression of the nucleus of the femoral head(±) Morphogenetic bone proteins(±) Vascularized bone graft(±) Autologous bone marrow graft | Hip arthroplasty |
| Bisphosphonates | Intertrochanteric osteotomies | |
| ESWT | ||
| Hyperbaric oxygen |
ESWT, extracorporeal shock waves therapy.
Sensory innervation of the hip joint is multiple and complex and comes from the sensory branches of the gluteal, obturator and sciatic nerves.3,4 Innervation of the hip originates from the sacral and lumbar plexuses. The hip, like other joints, follows Hilton's law, according to which, the nerves which innervate the muscles acting on the joint also innervate the joint itself. The femoral and obturator nerves innervate the anterior and anterolateral sides of the joint capsule, branches of the sciatic nerve innervate the posterior side of the capsule and branches of the quadratus femoris innervate the posteromedial side of the joint capsule. Lastly, joint branches of the gluteal nerve innervate the posterolateral portion of this capsule. The pain caused by this joint is mainly located in the inguinal region and extends to the thigh and trochanteric region.4
Peripheral nerve blocks act by interrupting the nociceptive pathway at its origin and the various afferent fibers which accompany the autonomous nerves, interrupting some algesic reflex mechanisms. Multiple types of blocks can be conducted, both neural and articular. According to their purpose, nerve blocks can be classified as diagnostic, prognostic and therapeutic. Diagnostic blocks attempt to confirm a suspected diagnosis through a reversible nerve block of the structure which is thought to cause the pain by means of a local anesthetic.5 All nerve blocks entail a risk of damaging the nerve, in a temporary or permanent manner.
Conventional radiofrequency is an ablative interventionist technique consisting in the emission through an electrode of radiofrequency waves capable of producing heat in the surrounding tissue, generating a lesion in the sensory nerves and interrupting the nervous impulse. There is a second modality, known as pulsed radiofrequency, in which no heat is produced and instead the analgesic effect is produced by the radiofrequency waves blocking electrical conduction of the sensory fibers which transmit pain. This type of block is indicated in patients suffering coxarthrosis with no possibility of surgical treatment, cases in which hip arthroplasty is deferred for any reason, in patients with hip prostheses with local pain in whom a surgical reintervention is ruled out, cases of avascular necrosis of the femoral head and cases of local bone metastasis.
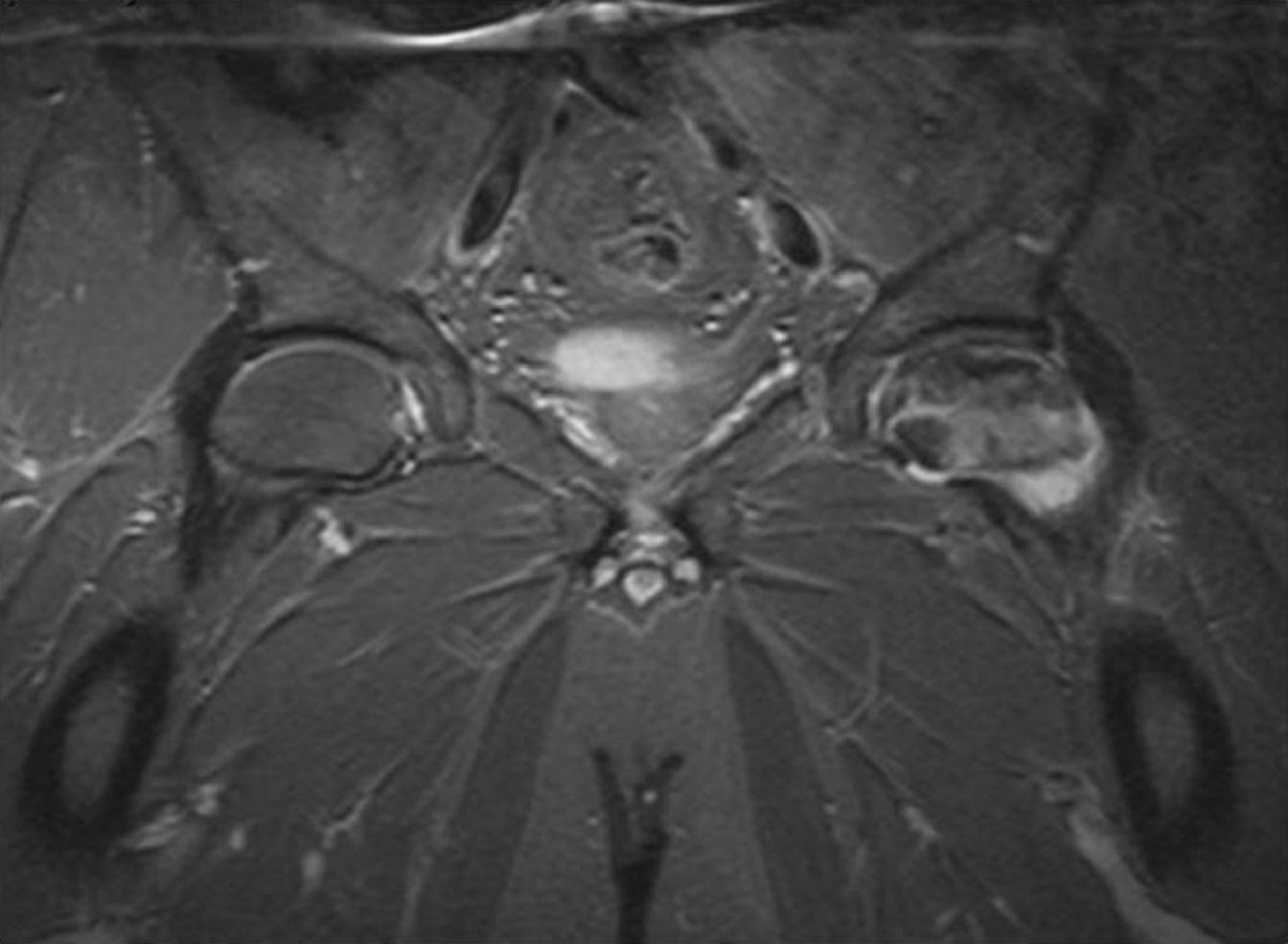
Case report n.° 1The patient was a 42-year-old male with no personal history of interest except for bilateral ANFH of unknown etiology. The laboratory data obtained enabled us to rule out an alteration of coagulation which could have explained the presence of bilateral ANFH, as well as possible episodes of fatty embolisms, atherosclerosis and adipose hypertrophy. Both hips presented the same level of involvement, grade IV according to the radiographic classification by Arlet and Ficat.6 Osteonecrosis was confirmed by magnetic resonance imaging (MRI). Fig. 1 shows the radiographic image. The patient reported severe limitations for work and everyday activities, such as climbing stairs, walking, getting dressed and personal hygiene. Due to his age, we decided to attempt analgesic options to delay hip arthroplasty temporarily. The pain on the right hip was the most incapacitating, so we decided to carry out a nerve block on that side. Oral analgesic treatment prior to the intervention consisted in oxycodone 30mg/12h, nabumetone 1g/12h and paracetamol 1g/8h. In spite of the high analgesic doses employed, the hip pain was so intense that it prevented physiotherapy.
Case report n.° 2The patient was a 79-year-old female with extensive associated comorbidity (non-insulin dependent diabetes mellitus, arterial hypertension, hyperlipidemia, obesity, repeated cerebrovascular accident, ischemic heart disease with severely depressed ejection fraction and chronic kidney failure). The usual treatment was applied, which included repaglinide 1mg/8h, nifedipine 30mg/24h, simvastatin 20mg/24h, furosemide 40mg/12h, 10mg nitroglycerine transdermal patch for 12h/day, acenocoumarol 4mg/24h and acetylsalicylic acid 100mg/24h. The patient also suffered ANFH with several years evolution of grade III in the Arlet and Ficat classification, which caused a significant decrease in quality of life due to pain in the inguinal region and thigh upon any physical activity, but a surgical intervention was ruled out by the patient after being informed of the high anesthetic-surgical risk (Fig. 2). The patients also presented poor tolerance to major and minor opiates (tramadol 150mg/24h, orally) after various administration patterns of these drugs (transdermal buprenorphine 52.5 mcg/h, transdermal fentanyl 25 mcg/h and oxycodone 20mg-naloxone 10mg/12h) due to vomiting, obnubilation and constipation. Poor analgesic control with nabumetone 1g/24h, metamizole 1g/8h and paracetamol 1g/8h.
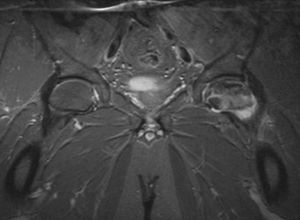
MRI scan of the hips. Intraarticular hemorrhage extending through the capsule. Marked alteration of the signal of the femoral head of the neck and the intertrochanteric region of the left hip; all this region appears hypointense in T1 and hyperintense in T2 with fat suppression. Bone edema with minimal left acetabular edema. Studies compatible with advanced left hip osteonecrosis.
The patient was a 33-year-old male with a history of ANFH of idiopathic etiology, of grade II in the Arlet and Ficat classification (Fig. 3), with no other associated medical comorbidities. He suffered incapacitating pain for everyday activities despite oral analgesic treatment with tapentadol 100mg/12h, paracetamol 1g/8h and amitriptiline 25mg/24h. He had been previously treated with load restriction and oral bisphosphonates (alendronic acid 70mg/weekly for 12 months) with a poor response. He was included in the surgical waiting list to carry out a decompression of the nucleus of the femoral head.
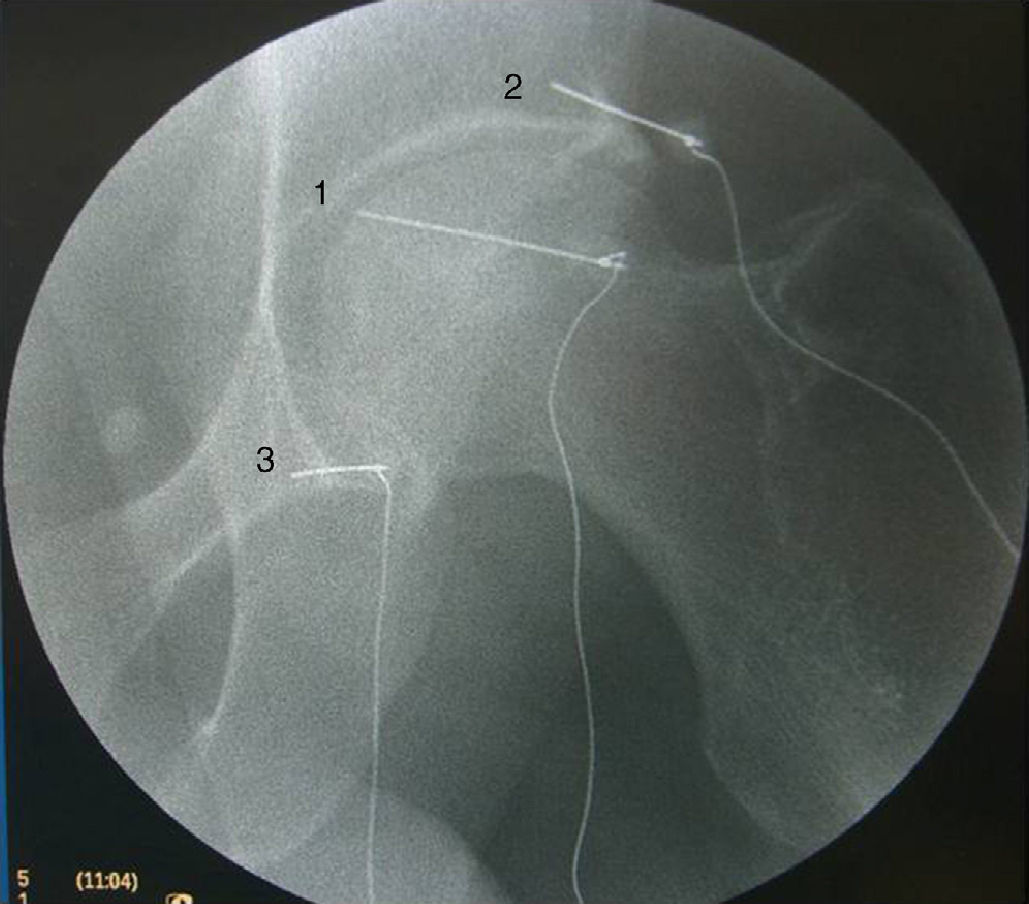
After signing an informed consent form, all cases underwent the technique in an operating room under local anesthesia and sedation, with standard monitoring, radioscopic control and under sterile conditions throughout the entire procedure. In the second case, oral anticoagulants were replaced by low molecular weight heparins prior to the technique. We also administered midazolam (2mg) and intravenous fentanyl (0.1mg) to improve comfort during the procedure. Patients were placed in a supine position. In order to block the articular branch of the obturator nerve, the needle was placed in the anteromedial side of the extraarticular portion of the hip joint, medial to the femoral artery and under the inguinal ligament. The tip was directed towards the union between the ischium and pubis. In the case of the articular branch of the femoral nerve, the needle was placed under the anteroinferior iliac spine, in the anterolateral side of the extraarticular portion. The tip rested under the anteroinferior iliac spine, near to the anterolateral margin of the hip joint. Sensory and motor stimulation were conducted after placing the needles as indicated, prior to conducting the diagnostic nerve block. Sensory stimulation was carried out at 50Hz and aimed to reproduce the pain suffered by patients at 0.3–0.5V. Subsequently, we performed motor stimulation at 2Hz, which should be negative at 1.5–2V, in order for the block to be more effective. Initially, a diagnostic block with 0.25% levobupivacaine was carried out, and significant pain relief was obtained in both cases, albeit temporarily, so a second block was carried out through radiofrequency with a Cosman G4 (Cosman Medical, Inc. Burlington MA, US) radiofrequency generator, so as to obtain a thermal lesion at 90°C for 90s with 3 cannulae of caliber 22 GA, 10cm with a 10mm active tip (RFK-CC10102-P; Radionics, Burlington, MA, US), placed following the same technique described for diagnostic nerve blocks.
No postoperative complications took place in the first and third cases. In the second case, a small anesthetized area appeared after the technique was conducted, which persisted over time.
We achieved a reduction of pain in the right hip at 4 weeks after the procedure, with a decrease in the visual analog scale of 75%, 50% and 80%, respectively, maintained at 6 months after the procedure, despite a reduction in the daily intake of analgesics. In the first case, once pain in the hip ceased it appeared in the right sacroiliac joint, and then remitted after infiltration of the sacroiliac joint and nerve block of the right S1-S2-S3 sacral nerves. Subsequently, in view of the results of the infiltration, this patient underwent the same treatment on the left hip, obtaining a relief of 100% of left coxalgia.
In all cases, the application of conventional radiofrequency improved capacity for physical activities like walking, along with a significant decrease of hip pain.
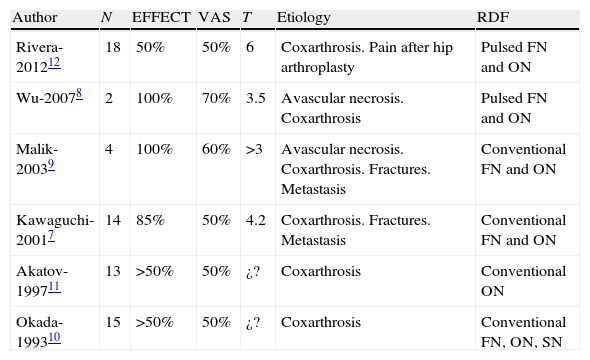
DiscussionThe main finding in our case reports was that blocking the sensory branches of the obturator and femoral nerves innervating the hip could be an adequate alternative for patients in whom surgery is to be delayed temporarily or is contraindicated due to a high anesthetic-surgical risk. It could be an additional treatment option to improve quality of life in cases of ANFH. In the past 30 years, performing this technique with local anesthetics has become increasingly popular, but its use with radiofrequency has been reported by very few authors. Our results agree with those reported by these few articles, which only include short series of case reports.7,8Table 2 presents the various works published in English on the use of pulsed or conventional radiofrequency for the symptomatic treatment of coxalgia. In this regard, the works of Kawaguchi and Wu reported an improvement of over 50% for various months after conducting conventional and pulsed radiofrequency of the sensory branch of the femoral and obturator nerves, although the first author only studied 14 cases and the second author 2 cases.
Series of case reports with pulsed or conventional radiofrequency for the treatment of coxalgia of diverse etiology.
| Author | N | EFFECT | VAS | T | Etiology | RDF |
| Rivera-201212 | 18 | 50% | 50% | 6 | Coxarthrosis. Pain after hip arthroplasty | Pulsed FN and ON |
| Wu-20078 | 2 | 100% | 70% | 3.5 | Avascular necrosis. Coxarthrosis | Pulsed FN and ON |
| Malik-20039 | 4 | 100% | 60% | >3 | Avascular necrosis. Coxarthrosis. Fractures. Metastasis | Conventional FN and ON |
| Kawaguchi-20017 | 14 | 85% | 50% | 4.2 | Coxarthrosis. Fractures. Metastasis | Conventional FN and ON |
| Akatov-199711 | 13 | >50% | 50% | ¿? | Coxarthrosis | Conventional ON |
| Okada-199310 | 15 | >50% | 50% | ¿? | Coxarthrosis | Conventional FN, ON, SN |
EFFECT, success rate of the procedure; FN, sensory branch of the femoral nerve; N, number of cases; ON, sensory branch of the obturator nerve; RDF, type of radiofrequency; SN, sensory branch of the sciatic nerve; T, duration of improvement of symptoms (in months); VAS, visual analog scale.
The study by Malik et al.9 reported a success rate close to 90% with some cases improving for up to 11 months among a series of 18 patients with unilateral hip osteoarthritis. This author highlighted the vital importance of a correct diagnosis of the etiology of pain in order to achieve high effectiveness rates. We also consider this aspect to be crucial, since it could explain the varying success rates of the technique in different series, as hip pain can be caused by discal, facet, sacroiliac and neurovascular disorders, as well as tendinopathy, intestinal hernia, myofascial alterations (piriform, quadratus lumborum and/or psoas), etc. In this regard, Okada10 and, to a lesser extent, Akatov,11 proposed a personalized ablation of the different nerve branches depending on the symptoms of each patient. In 2012, Rivera et al.12 published a series of 18 patients with medical contraindications for hip arthroplasty with excellent results.
In our cases, diagnostic nerve block provided a very temporary pain relief, but enabled us to identify responsive patients for a subsequent session of radiofrequency. In this regard, there are contradictory studies on the effectiveness of nerve blocks in the hip region with local anesthetics. Some authors consider the technique as an adequate analgesic option13,14 due to a hypothetical improvement of adductor muscle spasms which could entail a slight repositioning of the femoral head, whilst other works15 conclude that nerve block of the hip region with local anesthetics is not an effective technique, in agreement with our experience. In this sense, it seems logical that a simple block with local anesthetics should not produce pharmacological neurolysis maintained over time.
Radiofrequency is an interventionist technique consisting in the emission through an electrode of radiofrequency waves capable of generating heat and an electromagnetic effect in the surrounding tissue. The importance of this technique is that it is a scarcely invasive, percutaneous method which can be conducted on an outpatient basis. Therefore, this percutaneous denervation through radiofrequency can be applied to patients with high associated comorbidity, significant obesity and also in cases in which a delay of hip arthroplasty is considered opportune, like the patients presented in this work. In technical terms, it is a simple procedure with a minimal learning curve, although it is more complex in obese and anticoagulated patients. Figs. 3 and 4 present the correct location of the needles in a patient treated at our unit. In such cases, we recommend a non-perpendicular approach, which is more complex but entails a lower probability of damaging the femoral vessels and could also increase the effectiveness of radiofrequency by increasing the nerve surface in contact with the cannulae.16
Open sky section of the obturator nerve has been previously carried out for the treatment of painful hip osteoarthritis, but poor results and residual deficits have led the technique to be abandoned. This ablative technique is not without risks, including the appearance of disafferentiation syndromes, motor deficits and neuritis.17 One of our patients reported a small anesthetized area after the technique was applied.
In summary, sensory innervation of the hip joint is complex.1,4,14 Blocking the sensory joint branches of the obturator and femoral nerves through conventional radiofrequency could be an effective method to treat pain caused by hip disease and, therefore, could represent an option under certain circumstances. Additional studies with high methodological quality, preferably randomized and with a long follow-up period, are required to confirm the results obtained in this work.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Please cite this article as: Cortiñas-Sáenz M, Salmerón-Velez G, Holgado-Macho IA. Bloqueo intraarticular y de ramas sensoriales de los nervios obturador y femoral en cuadro de osteonecrosis y artrosis de cabeza femoral. Rev Esp Cir Ortop Traumatol. 2014;58:319–324.