The aim of the study is to evaluate the functional outcome, complications and general health in patients undergoing knee arthrodesis.
MethodsEighteen patients undergoing knee arthrodesis due to contraindication of primary or revision of a total knee arthroplasty (TKA). Anatomical arthrodesis was performed if there was a good contact of the two bone surfaces, whereas if it was not possible to achieve adequate femoral-tibial contact, artificial arthrodesis was performed. Function was assessed using the WOMAC score, and the health status using the SF-36.
ResultsFour patients were diagnosed with anatomical non-union arthrodesis and required a secondary surgical procedure to achieve fusion. Patients with artificial fusion did not have any secondary procedure. Patients less than 65 years old and the patients with anatomical fusion had a better outcome in the physical role and body pain area using the SF-36 score. WOMAC index outcomes were similar in all patients, regardless of age and fusion type.
ConclusionsAnatomical and artificial arthrodesis of the knee achieved pain relief, acceptable function of the limb and an adequate quality of life, with the best results in patients less than 65 years old.
Evaluar el resultado funcional, la incidencia de complicaciones y el estado general de salud de los pacientes con artrodesis de rodilla.
Pacientes y métodosEstudio retrospectivo de 18 pacientes con artrodesis de rodilla, en los que debido al fallo irreparable del aparato extensor, problemas de cobertura cutánea o afectación severa de la superficie ósea no estaba indicada una prótesis total de rodilla. Se realizó una artrodesis anatómica si había un buen contacto de las 2 superficies óseas. Si no era posible un contacto adecuado femoro-tibial se realizó una artrodesis artificial. Al final del seguimiento se hizo una valoración funcional con el cuestionario WOMAC y del estado general de salud con el SF-36.
ResultadosDe los 13 pacientes con artrodesis anatómica de rodilla consiguieron la fusión primaria 9 (69,2%) y 4 (30,7%) presentaron seudoartrosis los cuales necesitaron un procedimiento quirúrgico secundario para conseguir la fusión. Ninguno de los pacientes con artrodesis artificial precisó otro procedimiento. Los pacientes con artrodesis anatómica y los menores de 65 años obtuvieron la puntuación más alta en la esfera de rol físico, vitalidad y dolor corporal del SF-36. Los resultados del cuestionario WOMAC fueron parecidos en todos los pacientes independientemente de la edad y del tipo de artrodesis.
ConclusionesLa artrodesis de rodilla es una opción en cirugía de rescate, logrando con ambos métodos de artrodesis (artificial y anatómica) el alivio del dolor, una correcta función de la extremidad y una calidad de vida aceptable, consiguiendo los mejores resultados en los pacientes menores de 65 y en aquellos con artrodesis anatómica.
Knee arthrodesis is indicated in patients with knee pain and joint instability secondary to septic failure of a primary total knee arthroplasty (1TKA) or in patients who are not candidates for joint reconstruction, following severe damage to the bone surface, joint instability, inadequate soft tissue coverage, irreparable damage to the extensor apparatus, infection by resistant microorganisms or polymicrobial infection.1–4
There are various surgical techniques which achieve primary tibiofemoral fusion (external fixation, compression with plates and screws or intramedullary nails). Anatomic arthrodesis is that which requires a precise contact between the bone surfaces of the distal femur and the proximal tibia. In cases with significant bone loss, artificial arthrodesis5 is carried out with intramedullary systems which do not require contact between the bone surfaces. Neither type of arthrodesis (anatomic or artificial) has proven superior.
There are few studies evaluating the functional outcomes, postoperative complications and consequences on the quality of life of patients with either technique.
The hypothesis of this work is that knee arthrodesis is a good rescue option for patients with failure of total knee arthroplasties (TKA) who are not candidates for joint replacement.
The objective of this study was to evaluate the functional outcome, the incidence of complications and the overall health status of patients with knee arthrodesis.
Patients and methodsWe performed a retrospective study which included patients undergoing knee arthrodesis between March 1992 and March 2009. We excluded those patients with a follow-up period below 24 months and those whose medical records could not be obtained.
The total number of patients included in this study was 18 (13 females and 5 males). The mean age at the time of arthrodesis was 64.8 years (95% CI: 58.8–70.7). The affected knee was the right in 11 patients and the left in the remaining 7. The mean follow-up period was 6.3 years (range: 2.3–19.8 years).
The indication for arthrodesis in these patients was septic loosening of 1TKA (6 cases), septic loosening of a total knee arthroplasty replacement (TKAR) (4 cases), aseptic loosening of 1TKA (2 cases), sequela of osteoarticular tumour resection (3 cases), sequela of posttraumatic septic arthritis (2 cases) and joint instability as a sequela of poliomyelitis (1 case). None of the patients was a candidate for placing a 1TKA or a TKAR due to irreparable damage to the extensor apparatus, skin coverage problems or severe damage to the bone surface. Up to 7 patients had a history of associated musculoskeletal condition: 2 contralateral total hip arthroplasties, 1 ipsilateral femoral osteotomy, 3 contralateral 1TKA and 1 double arthrodesis of the ipsilateral foot (Table 1).
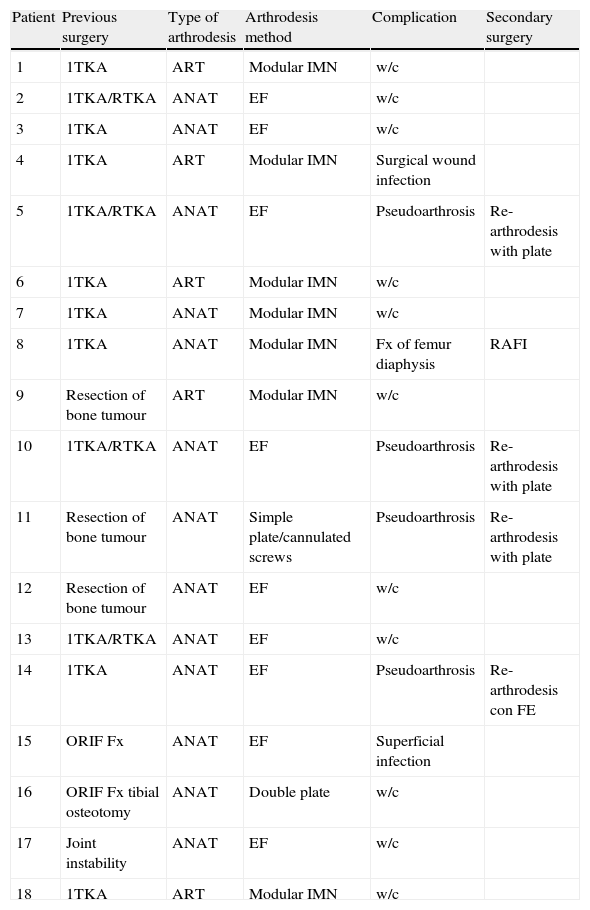
Characteristics of patients.
| Patient | Previous surgery | Type of arthrodesis | Arthrodesis method | Complication | Secondary surgery |
| 1 | 1TKA | ART | Modular IMN | w/c | |
| 2 | 1TKA/RTKA | ANAT | EF | w/c | |
| 3 | 1TKA | ANAT | EF | w/c | |
| 4 | 1TKA | ART | Modular IMN | Surgical wound infection | |
| 5 | 1TKA/RTKA | ANAT | EF | Pseudoarthrosis | Re-arthrodesis with plate |
| 6 | 1TKA | ART | Modular IMN | w/c | |
| 7 | 1TKA | ANAT | Modular IMN | w/c | |
| 8 | 1TKA | ANAT | Modular IMN | Fx of femur diaphysis | RAFI |
| 9 | Resection of bone tumour | ART | Modular IMN | w/c | |
| 10 | 1TKA/RTKA | ANAT | EF | Pseudoarthrosis | Re-arthrodesis with plate |
| 11 | Resection of bone tumour | ANAT | Simple plate/cannulated screws | Pseudoarthrosis | Re-arthrodesis with plate |
| 12 | Resection of bone tumour | ANAT | EF | w/c | |
| 13 | 1TKA/RTKA | ANAT | EF | w/c | |
| 14 | 1TKA | ANAT | EF | Pseudoarthrosis | Re-arthrodesis con FE |
| 15 | ORIF Fx | ANAT | EF | Superficial infection | |
| 16 | ORIF Fx tibial osteotomy | ANAT | Double plate | w/c | |
| 17 | Joint instability | ANAT | EF | w/c | |
| 18 | 1TKA | ART | Modular IMN | w/c |
1TKA, primary total knee arthroplasty; ANAT, anatomic; ART, artificial; EF, external fixator; IMN, intramedullary nail; ORIF Fx, open reduction and internal fixation of fracture; RTKA, replacement total knee arthroplasty; w/c, without complication.
In the 10 patients suffering septic loosening, the bacteriological study confirmed the presence of Staphylococcus aureus in 5 cases and of Staphylococcus epidermidis in the other 5.
Surgical methodAntibiotic prophylaxis with 2g of intravenous (iv) cefazolin was administered in all cases.
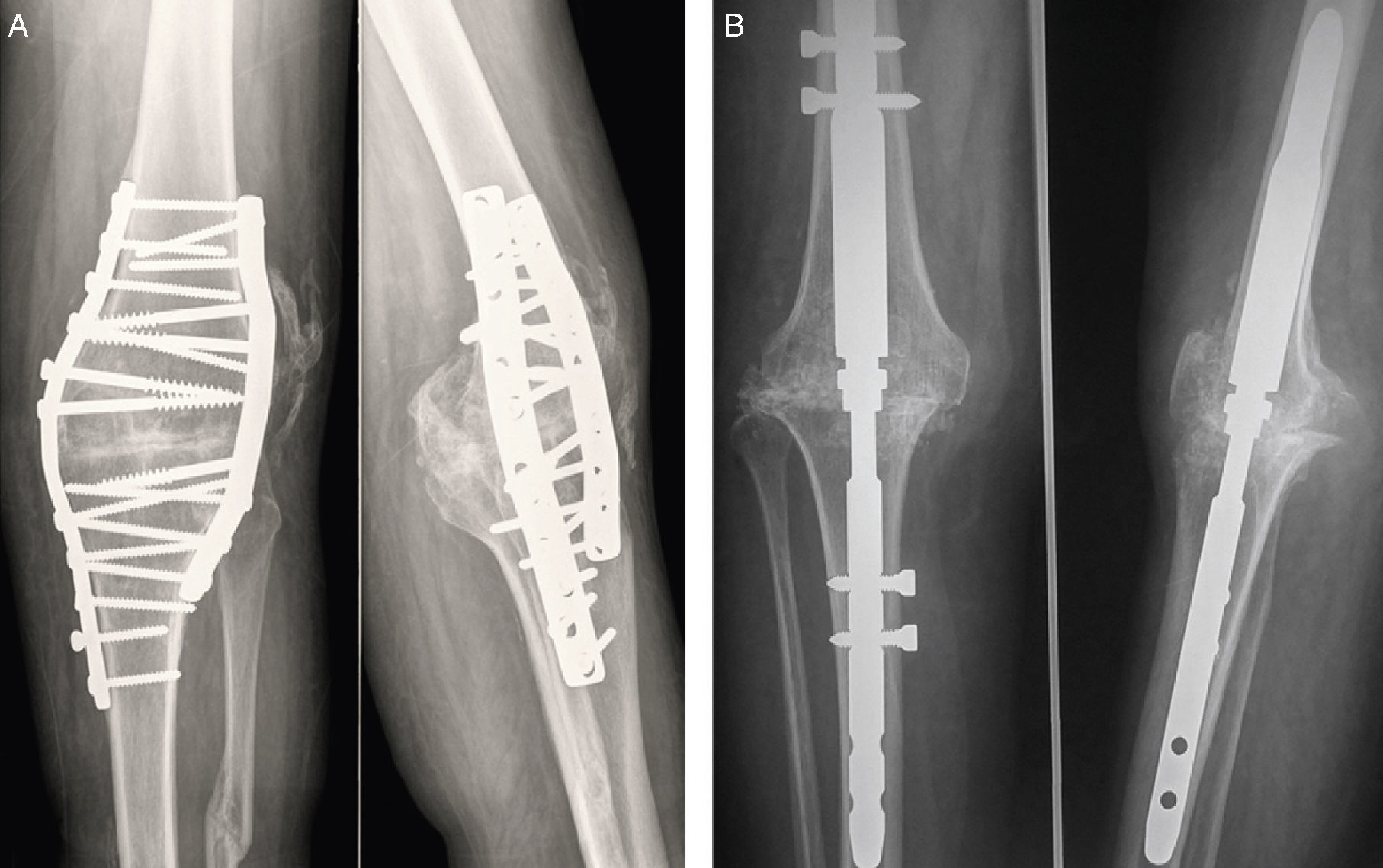
Patients with an adequate contact of the tibiofemoral bone surface underwent anatomic arthrodesis (13 cases). In 2 cases we employed compression by plates (Fig. 1A), in another 2 we used the Wichita® modular intramedullary nail (Stryker Howmedica Osteonics, Allendale, NJ, USA) with proximal and distal locking (Fig. 1B) and in 9 we employed external fixation: Hoffman ii® type (Stryker Howmedica Osteonics, Allendale, NJ, USA) in 3 patients, Wagner® type (Germany) in 3 patients, Orthofix® type (Orthofix, Verona, Italy) in 2 patients and Charnley system in 1 patient. In 10 of these patients we also used autologous bone taken from the patella or the iliac crest, and in 3 cases we associated demineralised bone matrix.
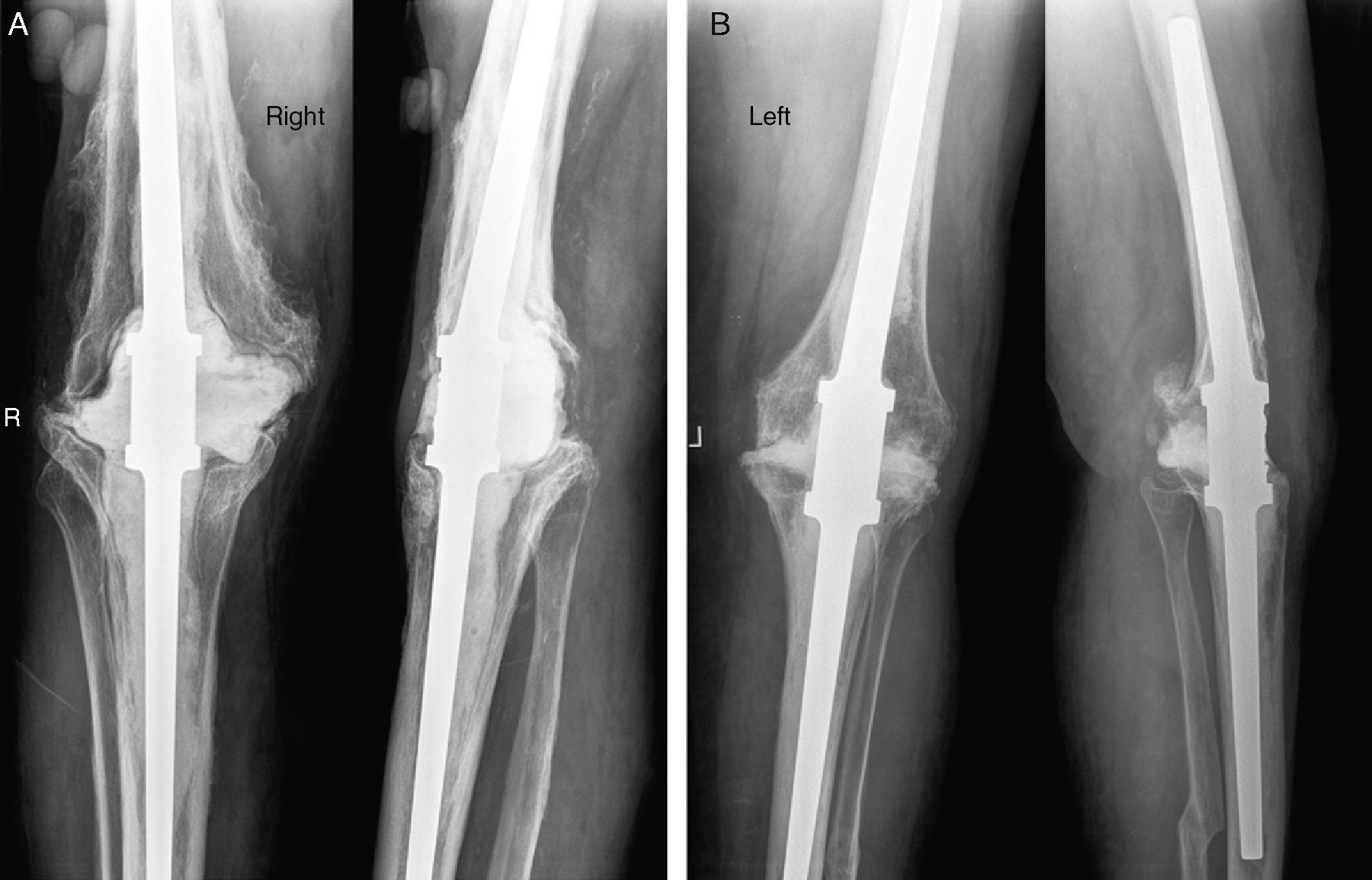
In patients with severe involvement of the bone surface and low physical demands in whom it was not possible to achieve good tibiofemoral contact, we performed artificial arthrodesis (5 cases) using an Endo-Model® type modular intramedullary nail (Waldemar Link GMBH&Co., Hamburg, Germany) with cement (Fig. 2).
In patients with septic failure, the conversion to arthrodesis was performed in 2 stages. In the first stage we removed the prosthetic components, performed a meticulous debridement and placed a spacer or cement chain with gentamycin. These patients received antibiotic treatment for a mean period of 3–6 months, depending on the bacterium and antibiogram. In the second stage we performed the definitive arthrodesis.
All patients received subcutaneous antithrombotic prophylaxis with low molecular weight heparin (LMWH).
We reviewed the medical records to study complications, operating time and secondary surgical procedures. The following postoperative complications were considered: pseudoarthrosis (nonunion), superficial infection (cellulitis or surgical wound infection) and peri-implant fracture.
Evaluation of patientsBone fusion time was assessed in patients with anatomic arthrodesis. This was deemed correct when a bridge of bone trabeculae could be observed in the fusion site in both anteroposterior and lateral radiographs.
A subjective functional assessment was conducted at the end of the follow-up period using the Western Ontario and McMaster Universities (WOMAC)6 and Short Form-36 (SF-36)7 questionnaires. The WOMAC questionnaire consists of 24 items exploring 3 dimensions: pain (5 items), rigidity (2 items) and level of difficulty of physical activities (17 items). Each item is scored from 0 to 4, with 0 being the absence of the symptom and 4 its maximum intensity, so the final score in the pain dimension is from 0 to 20, in the rigidity dimension from 0 to 8 and in physical function from 0 to 68. The lowest score in each of the 3 dimensions is considered the best result. The general health status was assessed through the SF-36 questionnaire, which assesses 8 different dimensions with scores from 0 (worst health) to 100 (best health) in order to evaluate the effect of the arthrodesis on physical, mental and emotional health. A score over 50 points is considered as a good quality of life.
Statistical analysisThe software package SPSS® for Windows® version 14.0 (SPSS Inc., Chicago, IL, USA) was used for the descriptive statistical study.
ResultsPrimary fusion was achieved in 9 (69.2%) of the 13 patients who underwent anatomic arthrodesis. The median (Md) period for primary fusion in these patients was 14.3 weeks (range: 9–24). A secondary surgical procedure was required to achieve fusion in the remaining 4 patients.
All patients who underwent artificial arthrodesis reported an improvement of symptoms and joint stability, without requiring any secondary surgical procedures.
Postoperative complications were observed in 7 (38.8%) of the 18 patients. In the anatomic arthrodesis group they were observed in 6/13 (46.1%) patients: 4 cases of pseudoarthrosis (the plate compression system had been employed in 1 case, which required re-arthrodesis with a new plate, whereas in the 3 remaining cases external fixation was used, requiring an autologous bone substitute from the iliac crest and re-arthrodesis, 2 with a plate and 1 with an external fixator), 1 case of cellulite at the entry point of the external fixator pins and 1 case of femoral diaphysis fracture in a patient in whom a Wichita® type modular intramedullary nail had been used and who required open reduction and osteosynthesis with a plate and cerclage without nail removal.
One complication was observed (20%) in the artificial arthrodesis group. The patient presented an infection of the surgical wound (Table 1).
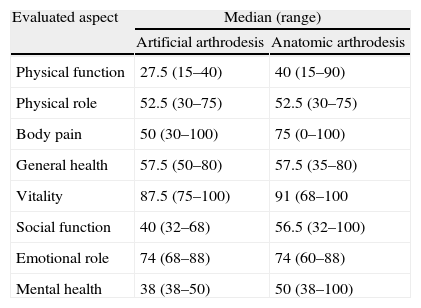
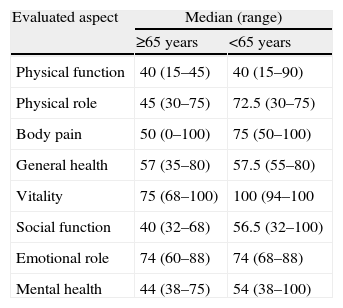
The SF-36 and WOMAC questionnaires were completed by 10 patients (55.5%): 4 cases with artificial arthrodesis (Endo-Model® intramedullary nail) and 6 with anatomic arthrodesis (1 Wichita® intramedullary nail, 2 plates and 3 Hoffman® type external fixators). Of the 8 patients who did not complete the surveys, 2 had died from causes unrelated to the knee arthrodesis, 3 were lost during follow-up and 3 did not complete the questionnaires. When studying the results in the 8 dimensions of the SF-36 questionnaire, the highest scores were obtained in the field of vitality, emotional role and body pain (Table 2). When assessing the results according to the age of patients, it was found that those aged less than 65 years had a higher median (Md) score in the aspects of vitality Md=100 (range: 54–100), body pain Md=75 (range: 50–100), physical role Md=72.5 (range: 30–75) and physical function Md=56.5 (range: 32–100) (Table 3). When comparing the results by type of fusion, those with anatomic arthrodesis showed the best results in the fields of body pain Md=75 (range: 0–100), vitality Md=91 (range: 68–100), emotional role Md=74 (range: 60–88) and physical function Md=56.5 (range: 32–100) (Table 4).
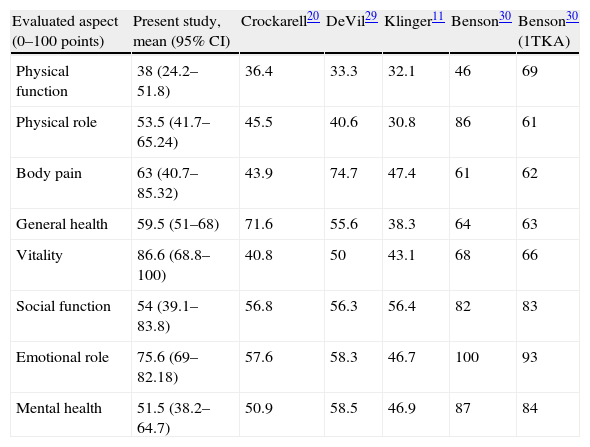
Comparison of the mean scores in the SF-36 questionnaire in our series obtained after 6.3 years follow-up, with those obtained in other series.
| Evaluated aspect (0–100 points) | Present study, mean (95% CI) | Crockarell20 | DeVil29 | Klinger11 | Benson30 | Benson30 (1TKA) |
| Physical function | 38 (24.2–51.8) | 36.4 | 33.3 | 32.1 | 46 | 69 |
| Physical role | 53.5 (41.7–65.24) | 45.5 | 40.6 | 30.8 | 86 | 61 |
| Body pain | 63 (40.7–85.32) | 43.9 | 74.7 | 47.4 | 61 | 62 |
| General health | 59.5 (51–68) | 71.6 | 55.6 | 38.3 | 64 | 63 |
| Vitality | 86.6 (68.8–100) | 40.8 | 50 | 43.1 | 68 | 66 |
| Social function | 54 (39.1–83.8) | 56.8 | 56.3 | 56.4 | 82 | 83 |
| Emotional role | 75.6 (69–82.18) | 57.6 | 58.3 | 46.7 | 100 | 93 |
| Mental health | 51.5 (38.2–64.7) | 50.9 | 58.5 | 46.9 | 87 | 84 |
1TKA, primary total knee arthroplasty; 95% CI, 95% confidence interval.
Results of the SF-36 questionnaire according to the type of arthrodesis after 6.3 years follow-up.
| Evaluated aspect | Median (range) | |
| Artificial arthrodesis | Anatomic arthrodesis | |
| Physical function | 27.5 (15–40) | 40 (15–90) |
| Physical role | 52.5 (30–75) | 52.5 (30–75) |
| Body pain | 50 (30–100) | 75 (0–100) |
| General health | 57.5 (50–80) | 57.5 (35–80) |
| Vitality | 87.5 (75–100) | 91 (68–100 |
| Social function | 40 (32–68) | 56.5 (32–100) |
| Emotional role | 74 (68–88) | 74 (60–88) |
| Mental health | 38 (38–50) | 50 (38–100) |
Results of the SF-36 questionnaire according to age after 6.3 years follow-up.
| Evaluated aspect | Median (range) | |
| ≥65 years | <65 years | |
| Physical function | 40 (15–45) | 40 (15–90) |
| Physical role | 45 (30–75) | 72.5 (30–75) |
| Body pain | 50 (0–100) | 75 (50–100) |
| General health | 57 (35–80) | 57.5 (55–80) |
| Vitality | 75 (68–100) | 100 (94–100 |
| Social function | 40 (32–68) | 56.5 (32–100) |
| Emotional role | 74 (60–88) | 74 (68–88) |
| Mental health | 44 (38–75) | 54 (38–100) |
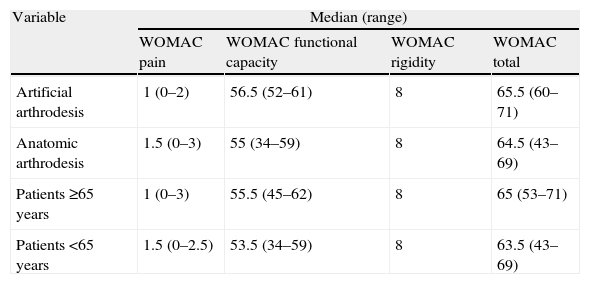
According to the WOMAC questionnaire, patients with an anatomic arthrodesis had Md=1.5 points (range: 0–3) in the pain dimension, while those who underwent artificial arthrodesis had Md=1 point (range: 0–2). Patients older than 65 years showed discreetly lower results compared to those under the age of 65 years, Md=1 point (range: 0–3) and 1.5 (range: 0–2.5), respectively. In the dimension of functional capacity, the WOMAC questionnaire result was 55 points (range: 34–59) among those patients with an anatomic arthrodesis, and 53 points (range: 34–59) among those under 65 years, with no significant differences between patients with an artificial arthrodesis and those over 65 years (Table 5).
Results of the WOMAC questionnaire according to the type of arthrodesis and the age of patients after 6.3 years follow-up.
| Variable | Median (range) | |||
| WOMAC pain | WOMAC functional capacity | WOMAC rigidity | WOMAC total | |
| Artificial arthrodesis | 1 (0–2) | 56.5 (52–61) | 8 | 65.5 (60–71) |
| Anatomic arthrodesis | 1.5 (0–3) | 55 (34–59) | 8 | 64.5 (43–69) |
| Patients ≥65 years | 1 (0–3) | 55.5 (45–62) | 8 | 65 (53–71) |
| Patients <65 years | 1.5 (0–2.5) | 53.5 (34–59) | 8 | 63.5 (43–69) |
Of the 10 patients, 3 were able to walk without the use of an assistive device, 4 used a cane, 2 used 2 canes and 1 patient used a walking frame.
DiscussionAt present, knee arthrodesis is a rescue surgery.8–11 In the series presented in this work we obtained a mean primary fusion time of 14.2 weeks (range: 9–22) and a primary fusion rate of 69.2% (9/13), excluding the 5 patients who underwent artificial arthrodesis.
The primary fusion time and rate depend on the technique used, age, prior surgical procedures and the indication for arthrodesis. A primary fusion time between 9 and 32 weeks8 and primary fusion rate between 33% and 100%10,11 have been reported previously. Ellingsen et al.12 considered that the fusion rate was not related to the number of previous procedures, absence of infection or type of TKA. Wilde et al.9 indicated that the fusion rate decreased as a function of metaphyseal bone loss.
There is controversy regarding the adequate time and surgical technique for the indication. Bargiotas et al.8 considered that in the case of TKA or RTKA septic failure, eradicating the infection was fundamental to the success of a knee arthrodesis. Therefore, they recommended performing it in 2 steps and reported a success rate of 83.3%. Other authors note that even in 2 steps, up to 55% of cases present positive cultures at the time of the arthrodesis.9
The rate of complications following knee arthrodesis varies between 20% and 84%.9 The most common is pseudoarthrosis, observed in up to 11% of cases.13,14 Others such as persistent infection, osteomyelitis, peroneal nerve palsy, deep vein thrombosis and peri-implant fracture are less common. These complications can lead to failure of the tibiofemoral fusion. The supracondylar amputation rate following failure of knee arthrodesis has been reported to be between 8% and 11%.8,12
In our series there were 4 cases (24.3%) of pseudoarthrosis. Of these, 3 cases had undergone a procedure with external fixators and external compression plates. There were 2 cases (12%) of persistent infection and 1 case (6%) of fracture in the middle third of the femoral diaphysis. None of these cases required amputation surgery.
Different surgical techniques have been used to achieve anatomic arthrodesis: external fixators,1,15–17 compression through plates and screws,18,19 anterograde intramedullary nails,8,12,20,21 short modular intramedullary nails,2,21–24 and non-modular nails.25,26 Modular intramedullary nails have the advantage of being specifically manufactured according to the anatomical characteristics of each patient.
It is not uncommon to find large bone defects. These defects are observed mainly in elderly patients, after RTKA or after resection of a bone tumour. In these cases, the methods employed to achieve anatomic arthrodesis will fail due to poor contact between the bone surfaces. Voss5 introduced the concept of artificial arthrodesis as an alternative in cases of TKA septic failure and severe involvement of the bone surface. This type of arthrodesis does not require contact between bone surfaces and instead places a cement spacer with gentamycin at the level of the bone defect. Other authors have used modular nails with metallic, polyethylene or cement with gentamycin spacers around the central coupler.27
In the present study we indicated anatomic arthrodesis in 13 cases. In 9 cases we used an external fixator, in 2 cases plates and screws and in 2 cases modular intramedullary nails. Artificial arthrodesis was indicated in 5 cases, using an Endo-Model® type modular intramedullary nail and placing a cement spacer with gentamycin around the central coupler.
Different methods have been used to assess the functional level and quality of life of patients undergoing knee arthrodesis. Harris et al.28 evaluated the functional activity of each patient after undergoing an arthrodesis, resection arthroplasty or knee amputation and found that functional outcomes following femoral supracondylar amputation or resection arthroplasty were poor and unacceptable for most patients. However, patients who underwent knee arthrodesis were able to perform physical work and certain types of recreational activities. Crockarell et al.20 used the Knee Society Functional Assessments Average and obtained a result of 49 points (range: 35–50) at 7 years follow-up. Bargiotas et al.8 used the WOMAC scale and obtained a mean score of 64 points (range: 40–72) at 2 years follow-up. These authors analysed the total score and did not carry out an assessment of each of the dimensions considered by the questionnaire. In the series presented in this study, the median total score according to the WOMAC was 65 points (range: 43–71), with the pain dimension obtaining an index of 1.5 (range: 0–3) and the functional capacity dimension an index of 55 (range: 34–61). The results were similar when analysed by age and type of arthrodesis. It was noted that patients had more difficulty in climbing stairs, bending over, putting on socks and performing heavy work. However, all were able to bathe, dress and perform light activities such as walking on smooth surfaces or shopping with a stable knee and without pain.
Several studies have reported subjective quality of life results using the SF-36 questionnaire10,19,28,29 similar to those obtained in our series. The main effect was observed in the aspects corresponding to physical function, physical role and mental health. However, the mean scores in the dimensions of vitality, emotional role and body pain were 86.6, 75.6 and 63, respectively, with better results being obtained among patients younger than 65 years who underwent anatomic arthrodesis.
Crockarell20 and DeVil29 assessed the results according to the dimensions of the SF-36 in 15 and 19 patients, respectively, who underwent anatomic arthrodesis with anterograde intramedullary nails. They found statistically significant differences in all dimensions when compared to the values of the general population, with the most notable effects being found in physical function, physical role and vitality, after 7 and 5 years follow-up. Benson et al.30 compared the results obtained with the SF-36 in 9 patients who underwent anatomic arthrodesis with external fixation following TKA failure with those from patients who underwent 1TKA after a mean follow-up period of 3.3 years and found no significant differences in any dimension except for physical function.
Some limitations of this study include it being retrospective and covering a long period, the sample size, the lack of functional evaluation in 45% of patients and the non-uniformity in both the indication of arthrodesis and in the surgical technique employed, making it difficult to compare the results obtained with the different techniques used.
ConclusionsKnee arthrodesis is a valid option in rescue surgery following septic or aseptic failure of a TKA or after resection of a bone tumour. Both methods of arthrodesis (artificial and anatomic) achieve pain relief, correct function of the limb and acceptable quality of life, with the best results being obtained among patients younger than 65 years and those with an anatomic arthrodesis.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of human and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interest to declare.
The authors wish to thank the team of orthopaedic surgeons at Hospital Sant Rafael for their dedication to teaching and to the speciality.
Please cite this article as: Ramazzini-Castro R, Pons-Cabrafiga M. Artrodesis de rodilla en cirugía de rescate: estudio de 18 casos. Rev Esp Cir Ortop Traumatol. 2013;57:45–52.