To demonstrate the effectiveness of functional treatment for the fractures of the metatarsal, which consisted of immediate or early weight bearing without immobilisation.
Material and methodologyWe prospectively studied 276 patients with simple or complex fractures of the metatarsal, treated with a functional method which consisted of immediate (before the 3rd day since the fracture) or early (between 3rd and 21st day) effective weight bearing.
Inclusion criteria were patients aged 16-65, both sexes, diagnosed with isolated or multiple, closed or opened type I metatarsal fractures who did weight bearing exercises during the first 21 days.
We analysed the effects of the steroid injection proposed for this treatment in the focus of the fracture, the days of weight bearing, rehabilitation and number of metatarsal fractures.
Results were evaluated using AOFAS (American Orthopaedic Foot and Ankle Society) scores, days of work incapacity and complications of the treatment.
ResultsThe AOFAS score for patients treated functionally was excellent and we found few complications with it.
DiscussionThe functional method is based on the function of ligaments and muscles of the forefoot and the aid of a rigid-soled shoe which allows early weight-bearing to avoid secondary displacement of the fractures.
The results show that immediate weight bearing provides better results than delayed bearing. Injection of steroid does not appear to have any benefit.
ConclusionsWe propose the functional method for all closed displaced or non-displaced metatarsal fractures, except for the displaced fractures on the base of the fifth metatarsal.
Mostrar la efectividad del tratamiento funcional de las fracturas metatarsianas consistente en apoyo completo inmediato o precoz sin inmovilización.
Material y métodoSe estudian de manera prospectiva 276 individuos con fracturas metatarsianas simples o complejas tratadas con el método funcional, consistente en realizar apoyo sin inmovilización de manera inmediata (antes del tercer día de la lesión) o precoz (desde el 3.° al 21.° día de la fractura).
Los criterios de inclusión fueron pacientes de 16 a 65 años, de ambos sexos, con fractura cerrada y abierta grado I de metatarsianos, aislada o múltiple, que realizaron carga efectiva en los primeros 21 días.
Se analizaron los efectos de la inyección de esteroide en foco propuesta para este tratamiento, el tiempo de descarga, la rehabilitación, el tipo de trabajo desempeñado por el paciente y el número de metatarsianos fracturados.
Los resultados se evaluaron mediante la escala AOFAS (American Orthopaedic Foot and Ankle Society), la duración de la incapacidad laboral y las complicaciones del tratamiento.
ResultadosSe obtuvo una puntuación excelente en la escala AOFAS y un bajo grado de complicaciones.
DiscusiónEste método se fundamenta en la función de sostén del sistema músculo-ligamentario y el uso de un zapato con suela rígida, que permiten un apoyo precoz sin desplazamiento secundario.
La carga inmediata proporciona mejor resultado que la diferida, y la infiltración de esteroide no aporta beneficios.
ConclusionesProponemos el método funcional como tratamiento para todas las fracturas cerradas del metatarso desplazadas o no, excepto para las fracturas desplazadas de la base del quinto metatarsiano.
The objective of this study was to demonstrate the effectiveness of functional metatarsal fracture treatment, consisting of accomplishing immediate or early weight-bearing. This procedure is carried out with the help of a stiff-soled orthopaedic shoe (Fig. 1), without immobilisation, orthosis or support bandage.
Functional treatment of metatarsal fractures stems from an adaptation of postoperative treatment principles for percutaneous surgical techniques of the foot1 (immediate weight-bearing with a stiff-soled shoe following percutaneous metatarsal osteotomies and corticoid infiltration), because the conservative treatment protocols were considered to protect fracture callused without providing any benefits.2,3 In fact, the musculoligamentous system of the metatarsal (dorsal and plantar interosseous muscles, lumbrical muscles, transverse and metatarsal ligaments) acts as a restraining system capable of maintaining the individual's biped position by itself.4 In addition, in the face of a fracture, it attempts to prevent any significant displacement of the fragments; using a shoe with a stiff, flat sole distributes the pressures between the metatarsal heads and the calcaneus equally, while early weight-bearing allows small movements in the area of the fracture focus stimulate bony callus formation.5,6
As occurs in the immediate postoperative period of percutaneous foot surgery, infiltrating corticoid and anaesthetics in the fracture zone have been used as an analgesic/anti-inflammatory measure that permits early weight-bearing to improve consolidation.
Material and methodThis was a prospective study that included a sample of 276 individuals treated with the functional method in the period between January 2004 and July 2009. The study covered all the patients (except those excluded from the sample because they did not fulfil the inclusion criteria) treated for simple or complex metatarsal fractures at the FREMAP hospital in Seville by a single observer (IUPH) who was the one who handled or controlled patient treatment until discharge.
Inclusion criteriaPatients of both sexes who had received a diagnosis of metatarsal fracture, isolated or multiple, displaced or not, intra- or extra-articular, open or closed Gustilo grade I; whose age was within the range of 16 to 65 years (active work status); and who performed effective weight-bearing without a cast during the first 21 days after injury.
Exclusion criteriaPatients who did not belong to an active population (that is, outside of the age range of 16-65 years); who did not have short-term work disability status; who did not perform effective weight-bearing before 3 weeks after injury; those with concomitant diseases that lengthened the process; patients with open grade II or III fractures; and those with delayed diagnosis because the fracture was not recognised.
Study designThe study was approved by the Ethics Committee at the FREMAP hospital in Seville. All patients gave informed consent before undergoing the functional treatment. Likewise, they had previously been offered the chance to choose any of the possible treatments, being provided with protocol information on each of them, as well as the complications.
Several physicians handled the clinical and radiographic follow-ups, which was by general norm 1 weekly visit during the first 2 weeks, and then biweekly until discharge, a new assessment 4 weeks after the patient returned to work and a final assessment 1 year later. In the last 3 visits, American Orthopaedic Foot and Ankle Society (AOFAS) forefoot score (Kitaoka score3) was applied.
We instructed all the patients to perform complete weight-bearing immediately. In cases of hyperalgesia, we permitted them to defer the support or to walk with partial weight-bearing; however, full weight-bearing was always begun by the third week so as to be in action within the period of fibrous callus formation.5,6
Corticoid infiltration was carried out at the criteria of the physician who provided the first medical attention. This process was conditioned by the concurrence of diseases contraindicating it, the existence of a minimum inflammatory component or patient opposition. The protocol was as follows7: (1) infiltration of 2 cc of betamethasone (reservoir formula) with 1 cc of mepivacaine at 2% in each fracture area; (2) placement of the stiff-soled walking shoe and (3) immediate weight-bearing in accordance with the patient's pain tolerance.
The fractures were classified based on 3 parameters:
- –
The bone fractured: a classification pattern similar to that used for analysing the forefoot pressure areas was used,8 grouping the fractures into 4 categories: I: fractures of the first metatarsal; V: fractures of the fifth metatarsal; C: fractures of the central metatarsal; CC: complex fractures, as a combination of the previous categories.
- –
Structural continuity: Gustilo Grade I open and closed fractures.
- –
Fragment deviation: displaced and non-displaced fractures.
We analysed a series of variables: independent variables (type of treatment), dependent or result variables, and control variables.
Independent variableType of treatmentFunctional treatment was carried out in all patients, both in those who fulfilled conservative treatment criteria, as well as Rockwood's surgical criteria.9
Dependent or result variablesWe based the results on the AOFAS (Kitaoka) forefoot score applied at the time when the patient returned to work. The procedure for this score consists of a questionnaire in which, based on different items, foot pain, function and alignment are assessed. The maximum score is 100 points, classifying the results as follows: excellent (90-100 points), good (80-89 points), average (70-79 points) and poor (less than 70 points) (Table 1).
Kitaoka (AOFAS).
| Kitaoka score (AOFAS) | Score |
| A) Pain | 40 points |
| None | 40 |
| Occasional | 30 |
| Moderate, daily | 20 |
| Severe, almost always present | 0 |
| B) Function | 45 points |
| 1. Activities | |
| No limitations and no external support | 10 |
| No limitations in daily life, but limitations in sport, and no external support | 7 |
| Limitations in daily recreational life (crutch needed) | 4 |
| Severe limitations even with crutch | 0 |
| 2. Footwear requirements | |
| Any type of footwear | 5 |
| Only comfortable footwear or insole use | 3 |
| Special footwear or orthosis | 0 |
| 3. Walking (maximum distance) | |
| More than 2 km | 10 |
| Between 1.5-2 km | 7 |
| Between 0.5-1 km | 4 |
| Less than 350m | 0 |
| 4. Type of walking surface | |
| No difficulties on any walking surface | 10 |
| Some difficulties on uneven surfaces and stairs | 5 |
| Difficulties en on uneven surfaces and stairs | 0 |
| 5. Limp | |
| None | 10 |
| Mild | 5 |
| Obvious | 0 |
| C) Foot alignment | 15 points |
| Good: well aligned plantigrade foot | 15 |
| Average: plantigrade foot with some degree of misalignment, but asymptomatic | 8 |
| Poor: non-plantigrade foot and symptomatic | 0 |
| Total | Maximum 100 |
The variables studied, based on the duration of short-term disability (STD) from work, were the effects of: corticoid infiltration, immediate or late weight-bearing, treatment for rehabilitation, fracture type (according to the metatarsal fractured) and type of work performed by each subject (A: sedentary; B: prolonged standing on 2 feet and walking on flat surfaces; and C: walking on irregular surfaces).
To avoid bias in analysing the variables infiltration, weight-bearing and rehabilitation based on STD duration in the group of patients that underwent functional treatment, we excluded from the sample those that fulfilled Rockwood surgical indication criteria (50 patients). This exclusion was based on the fact that not all the physicians who participated in the prospective study applied the functional treatment technique in these cases (Tables 2–4).
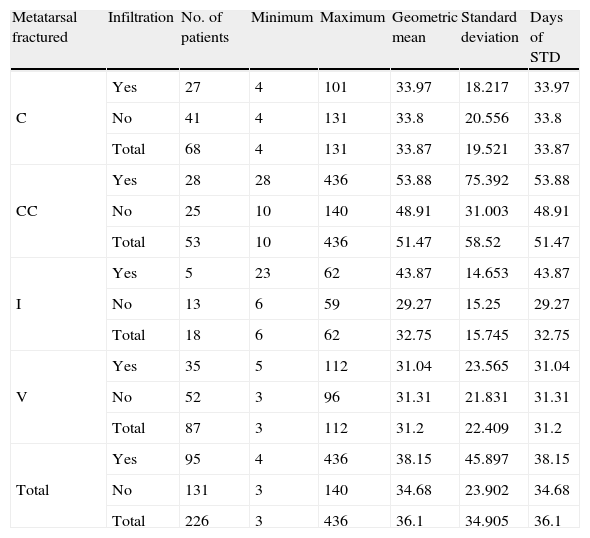
Short-term disability by area infiltration.
| Metatarsal fractured | Infiltration | No. of patients | Minimum | Maximum | Geometric mean | Standard deviation | Days of STD |
| C | Yes | 27 | 4 | 101 | 33.97 | 18.217 | 33.97 |
| No | 41 | 4 | 131 | 33.8 | 20.556 | 33.8 | |
| Total | 68 | 4 | 131 | 33.87 | 19.521 | 33.87 | |
| CC | Yes | 28 | 28 | 436 | 53.88 | 75.392 | 53.88 |
| No | 25 | 10 | 140 | 48.91 | 31.003 | 48.91 | |
| Total | 53 | 10 | 436 | 51.47 | 58.52 | 51.47 | |
| I | Yes | 5 | 23 | 62 | 43.87 | 14.653 | 43.87 |
| No | 13 | 6 | 59 | 29.27 | 15.25 | 29.27 | |
| Total | 18 | 6 | 62 | 32.75 | 15.745 | 32.75 | |
| V | Yes | 35 | 5 | 112 | 31.04 | 23.565 | 31.04 |
| No | 52 | 3 | 96 | 31.31 | 21.831 | 31.31 | |
| Total | 87 | 3 | 112 | 31.2 | 22.409 | 31.2 | |
| Total | Yes | 95 | 4 | 436 | 38.15 | 45.897 | 38.15 |
| No | 131 | 3 | 140 | 34.68 | 23.902 | 34.68 | |
| Total | 226 | 3 | 436 | 36.1 | 34.905 | 36.1 |
Fracture: C, central metatarsal; CC, complex; I, first metatarsal; V, fifth metatarsal.
Temporal disability in terms of weight-bearing.
| Metatarsal fractured | Weight-bearing | No. of patients | Minimum | Maximum | Geometric mean | Standard Deviation | Days of STD |
| C | Delayed | 28 | 4 | 131 | 33.72 | 22.79 | 33.72 |
| Immediate | 40 | 4 | 101 | 33.97 | 17.17 | 33.97 | |
| Total | 68 | 4 | 131 | 33.87 | 19.521 | 33.87 | |
| CC | Delayed | 12 | 28 | 436 | 62.45 | 112.299 | 62.45 |
| Immediate | 41 | 10 | 140 | 48.64 | 26.393 | 48.64 | |
| Total | 53 | 10 | 436 | 51.47 | 58.52 | 51.47 | |
| I | Delayed | 6 | 34 | 59 | 42.39 | 10.113 | 42.39 |
| Immediate | 12 | 6 | 62 | 28.79 | 17.48 | 28.79 | |
| Total | 18 | 6 | 62 | 32.75 | 15.745 | 32.75 | |
| V | Delayed | 33 | 10 | 96 | 37.1 | 22.233 | 37.1 |
| Immediate | 54 | 3 | 112 | 28.06 | 22.372 | 28.06 | |
| Total | 87 | 3 | 112 | 31.2 | 22.409 | 31.2 | |
| Total | Delayed | 79 | 4 | 436 | 39.21 | 49.747 | 39.21 |
| Immediate | 147 | 3 | 140 | 34.53 | 23.21 | 34.53 | |
| Total | 226 | 3 | 436 | 36.1 | 34.905 | 36.1 |
Fracture: C, central metatarsal; CC, complex; I, first metatarsal; V, fifth metatarsal.
Short-term disability in terms of treatment for rehabilitation.
| Metatarsal fractured | Rehabilitation | No. of patients | Minimum | Maximum | Geometric Mean | Standard deviation | Days of STD |
| C | No | 64 | 64 | 4 | 131 | 33.63 | 33.63 |
| Yes | 4 | 4 | 22 | 57 | 37.87 | 37.87 | |
| Total | 68 | 68 | 4 | 131 | 33.87 | 33.87 | |
| CC | No | 45 | 45 | 10 | 140 | 47.21 | 47.21 |
| Yes | 8 | 8 | 39 | 436 | 83.72 | 83.72 | |
| Total | 53 | 53 | 10 | 436 | 51.47 | 51.47 | |
| I | No | 15 | 15 | 6 | 62 | 31.71 | 31.71 |
| Yes | 3 | 3 | 34 | 43 | 38.49 | 38.49 | |
| Total | 18 | 18 | 6 | 62 | 32.75 | 32.75 | |
| V | No | 81 | 81 | 3 | 112 | 29.68 | 29.68 |
| Yes | 6 | 6 | 41 | 95 | 61.25 | 61.25 | |
| Total | 87 | 87 | 3 | 112 | 31.2 | 31.2 | |
| Total | No | 205 | 205 | 3 | 140 | 34.33 | 34.33 |
| Yes | 21 | 21 | 22 | 436 | 58.91 | 58.91 | |
| Total | 226 | 226 | 3 | 436 | 36.1 | 36.1 |
Fracture: C, metatarsal central; CC, complex; I, first metatarsal; V, fifth metatarsal.
The results were as follows:
- 1)
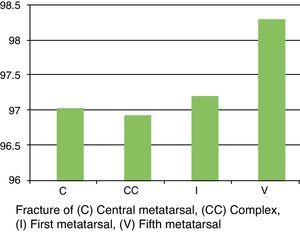
All groups (simple and complex fractures) attained a score of excellent (90-100) on the AOFAS scale (Fig. 2). There were no statistically significant differences in the mean AOFAS scores with respect to the metatarsals fractured.
- 2)
Student's t test value for the effect of corticoid infiltration and anaesthetics in the fracture area in relation to STD duration was P=.218.
Overall, in spite of their not being a statistically significant relationship, we found a lower mean STD duration in days for the 131 patients not treated with infiltration (mean STD days: 38.15) compared with the 95 individuals who did receive infiltration (mean STD days: 34.68).
We found the following in the analysis of each group (Table 2):
- a)
Group C (fracture of the central metatarsal): similar STD duration among the 27 patients receiving infiltration (mean STD days: 33.97) and the 41 who did receive infiltration (mean STD days: 33.80).
- b)
Group CC (complex fractures): lower STD duration (mean STD days: 48.91) for the 25 patients who did not receive area infiltration, compared with the 28 who were infiltrated (mean STD days: 53.88).
- c)
Group I (fracture of the first metatarsal): lower STD duration (mean STD days: 29.27) for the 13 patients not receiving area infiltration than for the 5 patients who were infiltrated (mean STD days: 43.87).
- d)
Group V (fracture of the fifth metatarsal): similar mean STD duration between the 35 infiltrated patients (mean STD days: 31.04) and the 52 non-treated patients (mean STD days: 31.31).
- a)
- 3)
Immediate weight-bearing was considered to be support in the first 3 days after the lesion. To assess the effect of such immediate weight-bearing (147 cases) and that of late weight-bearing (in the period from the third to the twenty-first day from the event of the fracture) (79 cases), we also applied Student's t test for comparison of means. Generally speaking, the value found was P=.157.
In addition, we studied the effect of weight-bearing with respect to the different patient groups. No statistically significant differences were found, although the mean STD days decreased for patients who carried out immediate weight-bearing in comparison with the individuals who carried this out in a delayed fashion. This decrease existed by globally (mean STD days for patients with immediate weight-bearing: 34.53; mean STD days for patients con delayed weight-bearing: 39.21) as well as in the study of each group (Table 3).
- –
Group C: the 28 patients who underwent delayed weight-bearing had 33.72 mean STD days, compared to 40 subjects who underwent immediate weight-bearing with a value of 33.97 for mean STD days.
- –
Group CC: a total of 12 patients had delayed weight-bearing treatment, with 62.45 mean STD days: the 41 patients with immediate weight-bearing treatment had 48.64 mean STD days.
- –
Group I: there were 6 patients who underwent delayed weight-bearing, resulting in a value for mean STD days of 42.39, against the 12 subjects who underwent immediate weight-bearing, with a result of 28.79 mean STD days.
- –
Group V: 33 patients had delayed weight-bearing, with 37.10 mean STD days; 54 patients had immediate weight-bearing, with 28.06 mean STD days.
- –
- 4)
With respect to the treatment for rehabilitation (Table 4), the samples for each group of fractures (C, CC, V y I) varied considerably. Consequently, no statistically significant differences were found.
- 5)
Related to the type of fracture and therapeutic indication (Rockwood criteria) (Table 5).
Table 5.Fracture classification. Indication of treatment and length of work disability.
Rockwood indication Metatarsal fractured No. of patients Days of STD (mean) Conservative C 68 33.87 CC 53 51.47 I 18 32.75 V 87 31.2 Total 226 36.1 Surgical C 7 46.43 CC 24 76.6 I 3 80.9 V 16 59.19 Total 50 65.98 Fracture: C: metatarsal central; CC: complex; I: first metatarsal; V: fifth metatarsal.
The 226 patients who fulfilled criteria for conservative treatment showed a statistically significant drop in the duration of STD, in the following order: complex fractures (No. of patients: 53; mean STD days: 51.47); fractures of metatarsal central (No. of patients: 68; mean STD days: 33.87); fracture of first metatarsal (No. of patients: 18; mean STD days: 32.75); and fracture of the fifth metatarsal (No. of patients: 87; mean STD days: 31.20). There were no significant differences in the length of STD among Groups C, I and V.
The 50 patients who fulfilled criteria for surgical treatment showed a decrease in the length of STD, in the following order: fractures of first metatarsal (No. of patients: 3; mean STD days: 80.90); complex fractures (No. of patients: 24; mean STD days: 76.60); fractures of the fifth metatarsal (No. of patients: 16; mean STD days: 59.10); and fractures of the central metatarsal (No. of patients: 7; mean STD days: 46.43). However, there was very little difference between Groups I and CC, and between Groups V and C.
- 6)
With respect to the type of work performed by each patient and its effect on duration of STD, no statistically significant differences appeared for the 3 groups. However, the mean STD days tended to be greater according to greater work intensity: mean STD days for the 29 patients in Group A: 35; mean STD days for the 116 patients in Group B: 39.50; mean STD days for the 131 patients in Group C: 33.98 (Table 6).
Table 6.Duration of the short-term disability by type of work.
Treatment Work No. of patients Short-term disability (STD) Median Standard deviation Functional A 29 35 26.677 B 116 39.5 46.094 C 131 43 33.981 Total 276 41 39.083 A: sedentary work; B: jobs requiring prolonged standing and walking on flat surfaces; C: jobs requiring walking on irregular surfaces.
Treatment complications have been few:
- –
Residual metatarsalgia: 1 case.
- –
Delay in consolidation: 2 cases (fractures of the fifth metatarsal base with significant divergence of fragments).
- –
Deep vein thrombosis: 1 case.
- –
Metatarsophalangeal osteoarthritis, tarso-metatarsal osteoarthritis or hallux rígidus: 3 cases.
- –
Complex regional pain: 1 case.
- –
Functional treatment for metatarsal fractures was initiated in 1999 by the authors of this study, directed then by Dr J.I. Martínez de Renobales. The basis was the idea that a metatarsal fracture should not behave very differently from an osteotomy when putting early weight-bearing into practise, as advocated in the beginnings of percutaneous surgical techniques on the foot.
Initially, the protocol consisted of administering corticoids in the fracture area before instituting immediate weight-bearing, based on the patient's pain tolerance.7 The corticoid was combined with local anaesthesia to achieve better diffusion in the area and immediate analgesia, which would allow the patient to perform immediate weight-bearing.
After that, through this prospective study, we wanted to ascertain whether steroid infiltration in the fracture area provided real benefits; we also wanted to study the effects of immediate vs. delayed weight-bearing after the lesion (Tables 2 and 3).
An attempt was made to establish the influence of the rehabilitation treatment following fracture consolidation. However, the reality was that the study samples differed greatly for each group, which led to our eliminating this variable when analysing the results (Table 4). Rehabilitation can constitute a support for functional treatment: however, we do not consider it absolutely necessary, given that functional treatment for metatarsal fractures does not need immobilisation. Consequently, functional treatment does not produce secondary joint rigidity and promotes venous return and disappearance of oedema and residual inflammation (Fig. 2).
We studied the results in 50 patients who, in spite of fulfilling Rockwood surgical treatment criteria, were treated with the functional method (Figs. 3 and 4) and STD duration fell within the range expected for this type of fractures (displaced and/or with joint involvement) when treated with surgery (Table 5). It should be pointed out that 2 cases of consolidation delay appeared in 2 patients who suffered a fracture of the base of the fifth metatarsal with significant fragment divergence.
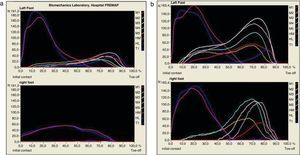
Dynamic study on a Footscan® pressure plate. (a) Dynamic study 2 months after the lesion. Observe the normal walking pattern on the left foot (early stance phase with increased heel pressures (HM, medial heel, and HL, lateral heel). Plantigrade weight-bearing phase with distribution of the pressures over the 5 metatarsals (M1, M2, M3, M4, M5), and kick off phase with increasing pressure over the first toe (T1) in contraposition with that of the affected foot, where there is barely any weight-bearing on the metatarsal, with the almost all of the weight being distributed on the heel; (b) dynamic study 13 months after the accident: observe how the pressures between both feet have become more equalised, with the patient performing a normal walking pattern.
Lastly, the duration of short-term disability was considered according to the type f work carried out by the patients. The obvious result obtained was that the workers with the most sedentary functions went back to their normal jobs first (Table 6).
ConclusionsFunctional treatment of metatarsal fractures provides good results, as deduced from the excellent mean score obtained in the AOFAS score and the few complications derived from such treatment.
We propose that this method should be generalised as the treatment for metatarsal fractures, advocating weight-bearing with a stiff-soled shoe, preferably during the first 3 days from the time the lesion occurred, with no need to infiltrate the fracture area with corticoid; the orthopaedic shoe should be removed when there is radiological evidence of consolidation.
A separate remark should be made on the fractures of the base of the fifth metatarsal, which involve significant displacement. In these cases, initial surgical treatment should be considered.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Úbeda Pérez de Heredia I, et al. Medición de resultados del tratamiento funcional de las fracturas metatarsianas mediante la escala AOFAS y la duración de la incapacidad laboral. Rev esp cir ortop traumatol. 2012;56(2):132–9.