Vascular complications are rare after total knee arthroplasty, and popliteal pseudoaneurysms are even more so. There are few cases reported in the literature. We present a case of an 80-year-old woman with osteoarthritis of the left knee, secondary to Genu varum, who was treated with total knee arthroplasty. On the discharge day after surgery, the patient suffered a popliteal pseudoaneurysm that was successfully treated with an intravascular stent introduced by an inguinal approach.
Las complicaciones vasculares después de cirugía protésica de rodilla son poco frecuentes. Dentro de este grupo, el pseudoaneurisma de la arteria poplítea es todavía más raro, habiéndose reportado en la literatura unos pocos casos. Presentamos el caso de una mujer de 80 años con el diagnóstico de gonartrosis izquierda por genu varo que fue intervenida de prótesis total de rodilla y que en el postoperatorio tardío previo al alta, presentó un pseudoaneurisma de la arteria poplítea que fue tratado satisfactoriamente mediante un stent intravascular por abordaje inguinal.
Vascular complications following prosthetic surgery are rare, with an incidence 0.03–0.5% of the cases.1–6 However, they present great morbidity. Among these vascular lesions, popliteal artery pseudoaneurysm constitutes a very uncommon lesion, with reports being few and far between.7–10
We present a new case of popliteal artery pseudoaneurysm, which arose a few days after surgery. After reviewing the existing literature in depth, we indicate the steps to bear in mind when diagnosing it and the various therapeutic alternatives for this serious lesion.
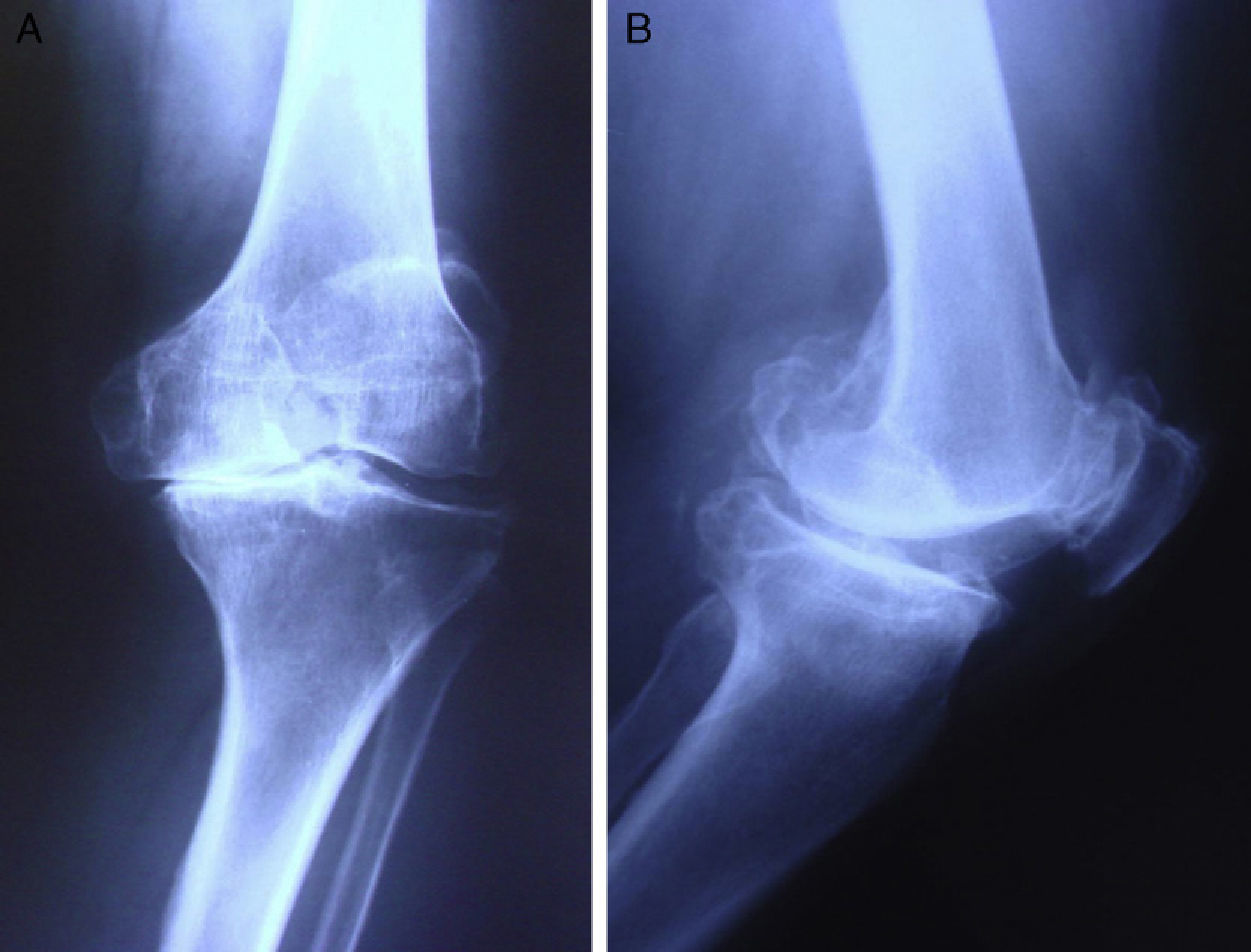
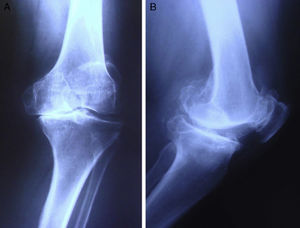
Clinical caseThe patient was an 80-year-old woman, who was admitted to our centre for total knee prosthesis (TKP) for left tricompartmental gonarthrosis secondary to bow legs (genu varum) (Fig. 1).
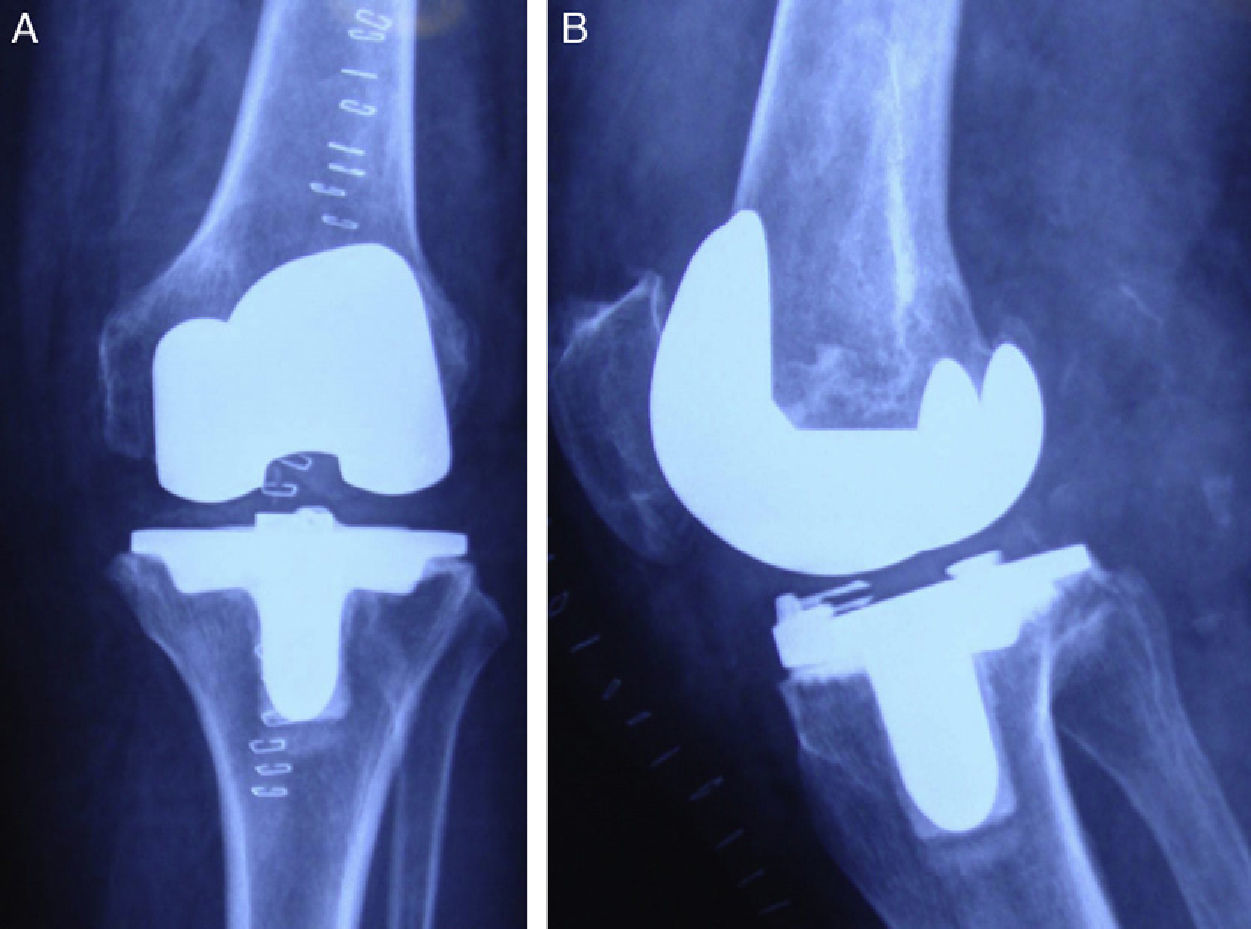
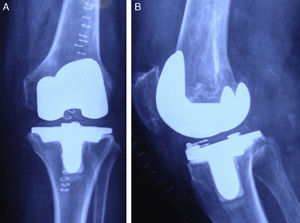
The only significant pathological antecedents were hypothyroidism under thyroid substitute treatment, chronic venous insufficiency of the lower limbs and dyslipidemia. The TKP surgery was uneventful, with appropriate radiographic control afterwards for initiating complete loading (Fig. 2).
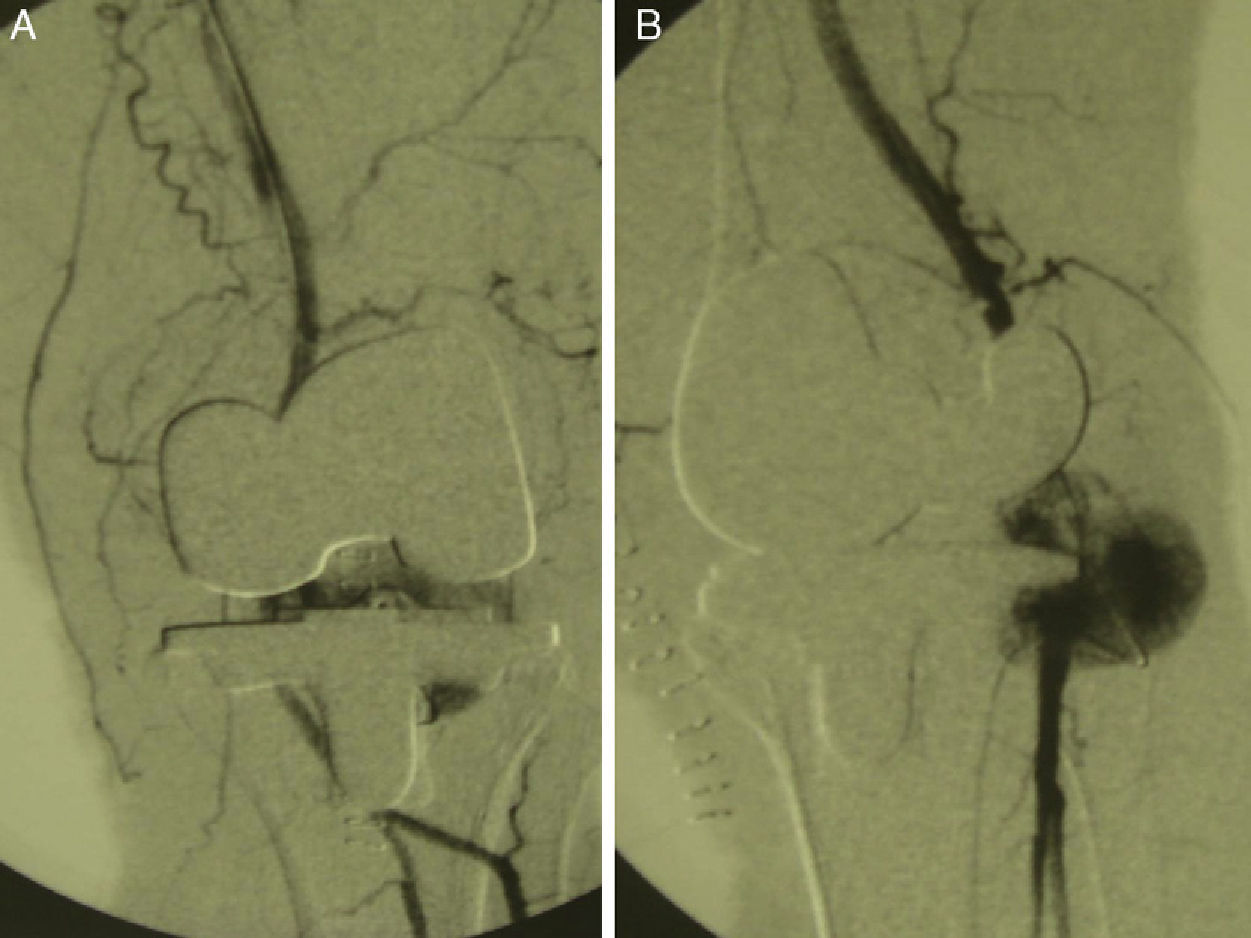
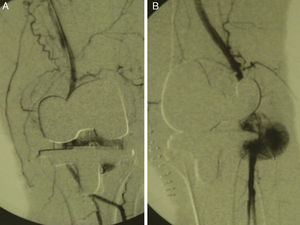
In the immediate postoperative period, the patient presented a wide cutaneous haematoma with oedema and significant knee and leg swelling; however, the distal pulses, mobility and sensitivity were conserved. On the 8th postoperative day, there was a great increase in clinical inflammation extending to calf and leg. Suspecting a deep venous thrombosis, we requested a vascular surgery consult. An echo-Doppler revealed a pulsatile mass with a diameter of 5cm at the level of the popliteal bone, which corresponded to a popliteal artery pseudoaneurysm. A later arteriograph study confirmed the diagnosis (Fig. 3).
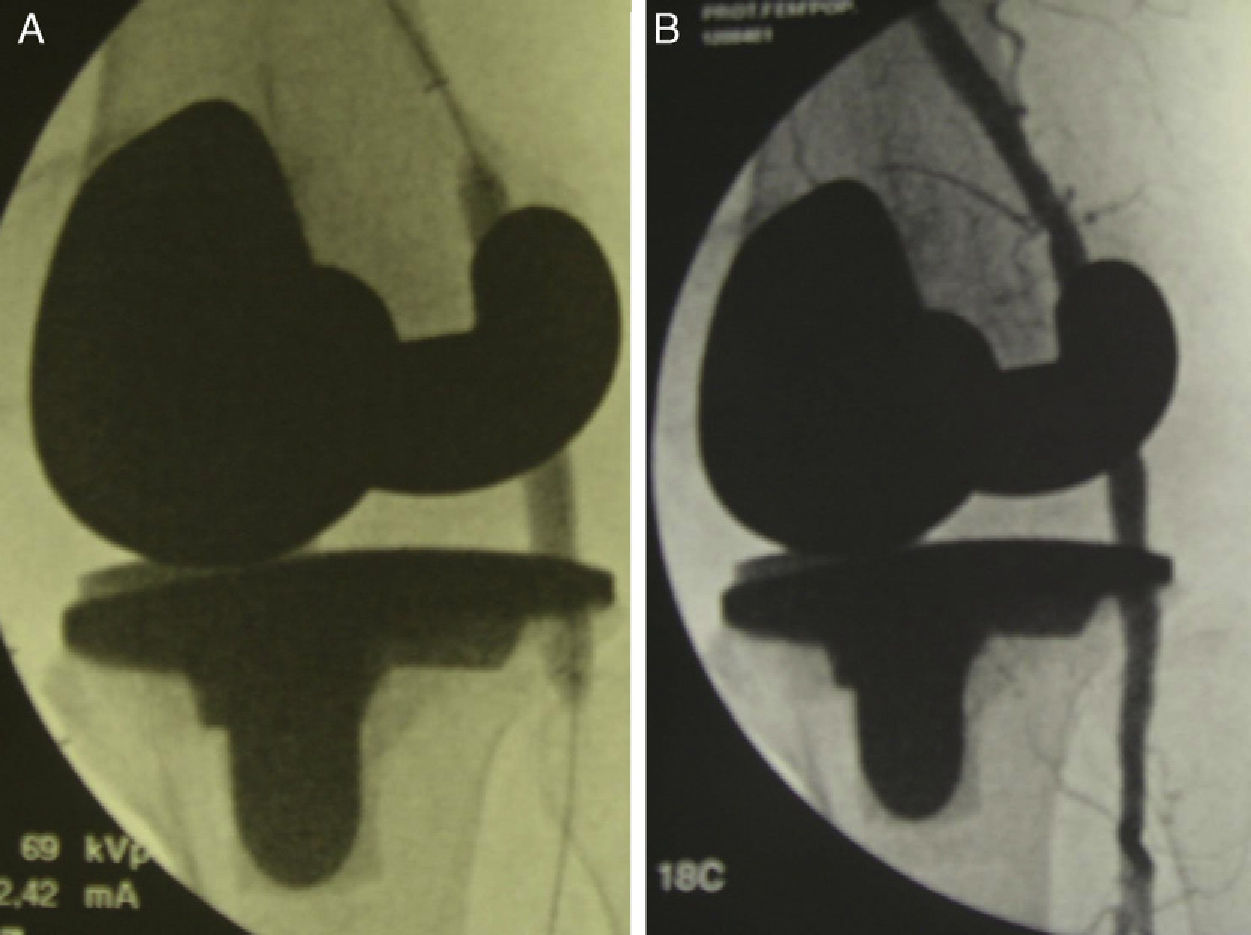
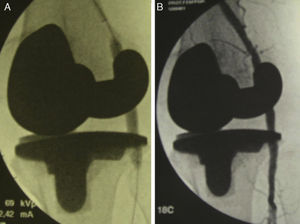
The treatment consisted of placing an intravascular stent using the femoral ilioinguinal approach (Fig. 4). Following 48h of rest, the patient initiated the standard TKP rehabilitation programme and was discharged 1 week after the vascular operation; that is, 2 weeks after admission. At 1 year after the surgery, the patient was free from pain, with distal pulses and joint movement of 0/100°. She did not need any type of help for walking.
DiscussionVascular complications in knee surgery are infrequent, but they have a high morbidity rate and consequences that are potentially fatal for the limb.11–13 The main artery affected in these cases is the popliteal, due to how close it is anatomically to the knee joint.14
If the traumatism is acute and serious, the consequences produced are more evident from the distal ischaemia in the limb. The foot is pale, lacking in capillary filling or it is excluded, with paresthesia, muscular debility, high drain flow or intractable pain. These symptoms can go unnoticed at times due to the anaesthetic block; a vascular surgeon should always be consulted in case of doubt, given that any delay in diagnosis and treatment can lead to irreversible ischaemia with compartmental syndrome and limb loss.1–10 In contrast, when the traumatisms are not so evident, a true pseudoaneurysm can arise, with clinical signs and symptoms of late thrombosis or recurrent embolic episodes.3,6,9 If the artery intima is injured and a pseudoaneurysm is produced, as in our case, the clinical signs and symptoms are normally localised, such as regional oedema and a pulsatile mass in the posterior side of the knee.6,9 It can also manifest as diffuse oedema in the entire leg, simulating a deep venous thrombosis, as happened in our patient. These symptoms usually become evident in the immediate postoperative period,3 although there are cases in which the diagnosis was not made until 5 months after surgery.1 In fact, the appearance of a geniculate artery pseudoaneurysm has even been described at 36 months after the operation.1
With respect to the injury mechanism, Butt et al.11 describe 4 different types of production:
- -
Patients having prior vasculopathy who present atheromatous plaques that, due to the tourniquet, present fragmentation with embolic episodes and/or postoperative thrombotic episodes.
- -
Injuries to the artery intima during the surgery, also due to the suction on the blood vessels that the tourniquet produces.
- -
Injury to the intima and/or compression against bony or muscle-tendon structures, in those cases of freeing contractures, especially flexion contractures.
- -
Puncture and/or direct laceration of the blood vessels by orthopaedic instruments (scalpel, retractor, oscillating saw, etc.).
The anatomical situation of the blood vessels is another important factor to take into consideration in vascular injuries. Calligaro et al.5 found an increase in vascular injuries in knee prosthetic revision due to the distortion suffered by the anatomy following the primary surgery. In addition, the proximity of the artery with the tibial posterior cortex, which lies 1–3mm from it, has to be considered. In 6% of the cases, even the birth of the anterior tibial artery, proximal to the popliteal muscle, has been described.15
In our patient, we do not know the exact cause of the popliteal artery injury. However, we speculate that the bone saw might have injured the arterial intima at the moment of the tibial cut. In Fig. 3B, it can be seen that the level of the pseudoaneurysm coincides with the tibial cut in the radiographic profile.
However the pseudoaneurysm happened, the treatment in this case was satisfactory.16–23 Although they go beyond our environment, the treatments proposed range from aneurysm excision and direct arterial repair, remote placement of an intravascular stent (as was the case for our patient) and balloon catheter embolisation, up to patch angioplasty. However, in spite of our good results, survival follow-up over a longer term would be helpful; this is especially true in the case of the intravascular stents, due to the great mobility of the knee joint, which can produce implant failures and migrations, obstructions and so on.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of humans and animals. The authors declare that the procedures followed were performed in compliance with the ethical regulations of the appropriate human experimentation committee and agreed with the World Medical Association and the Helsinki Declaration.
Data protection. The authors declare that they followed their centre's protocols on patient data publication and that all of the patients included in the study received sufficient information and gave written informed consent to participate in this study.
Right to privacy and informed consent. The authors obtained informed consent from the patients and/or subjects mentioned in the article. This document is filed with the corresponding author.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: González Rodríguez JC, et al. Pseudoaneurisma poplíteo como complicación de la artroplas-tia total de rodilla. Revisión y actualización bibliográfica a propósito de un caso. Rev Esp Cir Ortop Traumatol. 2012;56:205-9.