The purpose of this study is to determine the prognostic factors of a satisfactory functional outcome in patients using upper extremity prosthetics with a proximal third forearm stump, and above, level of amputation.
Materials and methodsAll patients with longitudinal deficiencies and traumatic amputations of upper extremity with a level of amputation of proximal third forearm and above were included. A total of 49 patients with unilateral upper extremity amputations that had used the prosthetic for a minimum of 2 years were included in the protocol. The Disability arm shoulder hand (DASH) scale was used to determine a good result with a cut-off of less than 40%. The independent variables were the level of amputation, the aetiology for its use, initial age of use and number of hours/day using the prosthesis.
ResultsIt was found that patients with a congenital aetiology and those that started using the prosthetic before 6 years of age had better functional results.
DiscussionIt was found that when adapting a patient with an upper extremity prosthetic, which has a high rejection rate of up to 49%, better functional outcomes are found in those who started using it before 6 years of age, and preferably because of a congenital aetiology. It was also found that the number of hours/day strongly correlates with a favourable functional outcome.
El objetivo de este artículo es evaluar los factores pronósticos para una adecuada adaptación protésica de extremidad superior y qué variables condicionan un resultado funcional satisfactorio en pacientes con una amputación por encima del tercio proximal del antebrazo.
Material y métodoSe incluyó en el estudio a 49 pacientes con deficiencias longitudinales o amputaciones traumáticas de extremidad superior de antebrazo proximal hasta desarticulación de hombro, con un tiempo mínimo de utilización de la prótesis de 2 años. Se utilizó la escala de Disability arm shoulder hand (DASH), tomando como un resultado satisfactorio un valor de menos de 40%. Las variables independientes fueron etiología del uso, nivel de la amputación, inicio de uso y h/día de uso.
ResultadosSe consideró de buen pronóstico a aquellos pacientes con una etiología congénita y cuando el inicio del uso de la prótesis era antes de los 6 años, mostrando una diferencia significativa entre los grupos.
DiscusiónSe encontró que la etiología congénita es de buen pronóstico, al igual que el caso de aquellos que utilizan la prótesis más de 6h/día. Por medio de este trabajo se pudieron demostrar mejores resultados funcionales en los pacientes a los que se les adapta una prótesis de extremidad superior antes de los 6 años y preferentemente por una etiología congénita. También se encontró que el número de horas de uso al día correlaciona con un resultado funcional favorable.
At present, there is controversy in the medical field regarding the advantages offered by prosthetic adaptation of an upper limb. These are indicated with the aim of providing patients with a mechanical tool allowing them sustained function of the affected limb, which facilitates a better interaction with the physical medium and psychosocial environment. These prostheses promote social acceptance by altering the physical appearance of the patient, and are useful tools for certain types of activities. However, in certain cases, children with longitudinal deficiencies or amputations have a high functional capacity and quality of life regardless of the use of the prosthesis.1 Little is known about the indications and factors related to an adequate functional prognosis and acceptance by patients of the use of these prostheses, so they are frequently indicated with a poor basis regarding the advantages of this type of devices to improve function and overall patient adaptation.
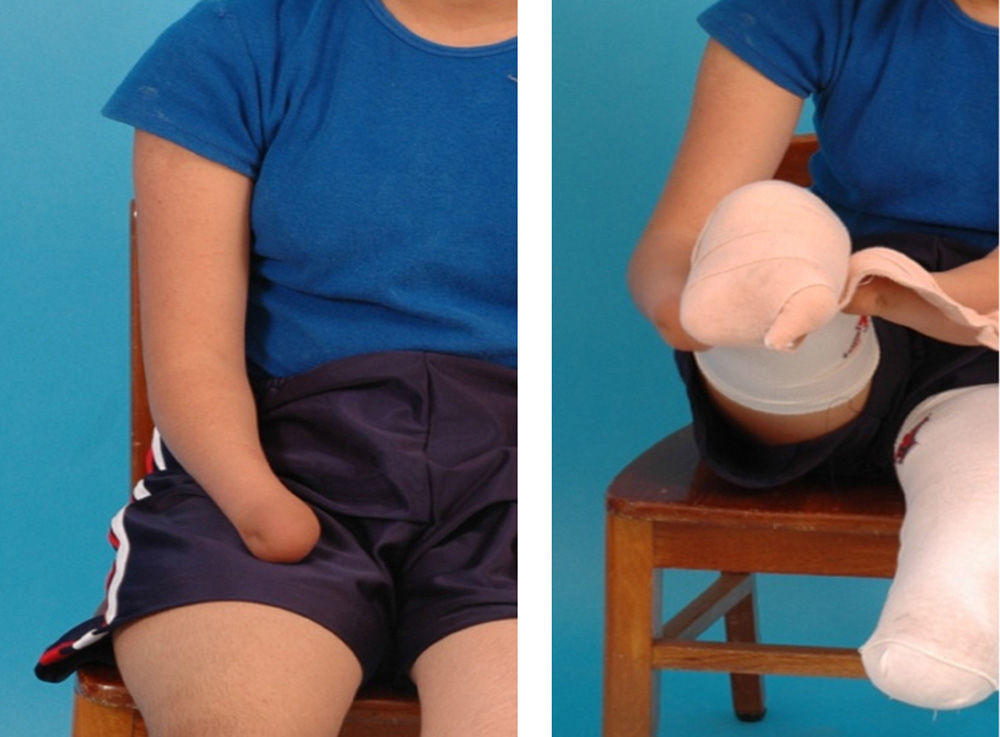
Despite the expectations of both parents and patients about having an instrument that increases functional capacity, frequently both end up not being satisfied with the end result and, despite the motivation given by both physicians and relatives, patients abandon their use at a later age (Fig. 1).2
The results in terms of prosthetic adaptation are variable, with a reported rate of rejection around 10–49%.3 Among the most frequent causes of rejection and abandonment of use are: discomfort caused by the harness, inconvenience for the use of certain types of clothing, skin irritation, increased heat production, weight of the prosthesis and cosmetic concerns.4 Roye et al. pointed out that children with chronic conditions had an adaptation response conditioned by a lack of knowledge of a different health condition.5 The study conducted by Postema et al. confirmed what the literature has historically proposed regarding upper limb prostheses, which are frequently limited to offering the patient a functional gain. It is for this reason that patients eventually reject them.6
This study aims to evaluate the prognostic factors for an adequate prosthetic adaptation in the upper limbs and the variables conditioning a satisfactory functional result. This should provide a better understanding regarding which patients will benefit from using an upper limb prosthesis.
Material and methodThis was a cross-sectional study with patients from Shriners Hospital for Children (Mexico D. F.), who used body activation upper limb prostheses during the period between January 1991 and June 2008. All the patients were amputated at least at the level of proximal forearm.
All patients underwent a psychological evaluation, as well as preprosthetic training for 2 months and prosthetic for a mean period of 4 months at the Department of Occupational Therapy of Shriners Hospital for Children (Mexico D. F.) once the prosthesis had been delivered. Use of the prosthesis was defined as usage for at least 2h/day. The Disability arm shoulder hand (DASH) scale was used to assess the function of the upper limb prosthesis. This scale evaluates the level of disability to carry out certain activities perceived by patients.7 The independent variables analysed to determine the functional prognosis were: level of amputation, age at the start of using the prosthesis, aetiology leading to the use of the prosthesis, number of hours of usage per day.
The clinical history was reviewed and all patients, or a direct relative, were interviewed to determine the independent variables and application of the DASH questionnaire.
A favorable functional result was determined as those patients with a DASH score <40%.
A sample of 67 patients was obtained, of which 8 were excluded due to a poor use of the prosthesis (<2h/day), 2 were excluded due to rejection of usage for over 6 months, and 8 could not be located to apply the DASH questionnaire, so the final study sample was comprised by 49 patients.
An analysis of the DASH scale was conducted with the independent variables through a Fischer exact test for all variables. The level of statistical significance was established at P<.05, with a 95% confidence interval (CI).
ResultsOut the 49 patients, 37 (75.5%) had a proximal forearm stump, 5 (10.2%) a transhumeral stump and 7 (14.2%) were disjointed at the shoulder. A total of 36 (73.4%) had a congenital aetiology and 13 (16.6%) had a traumatic aetiology. The mean age of the sample was 11.5 years, with a minimum age of 3 and a maximum age of 18 years.
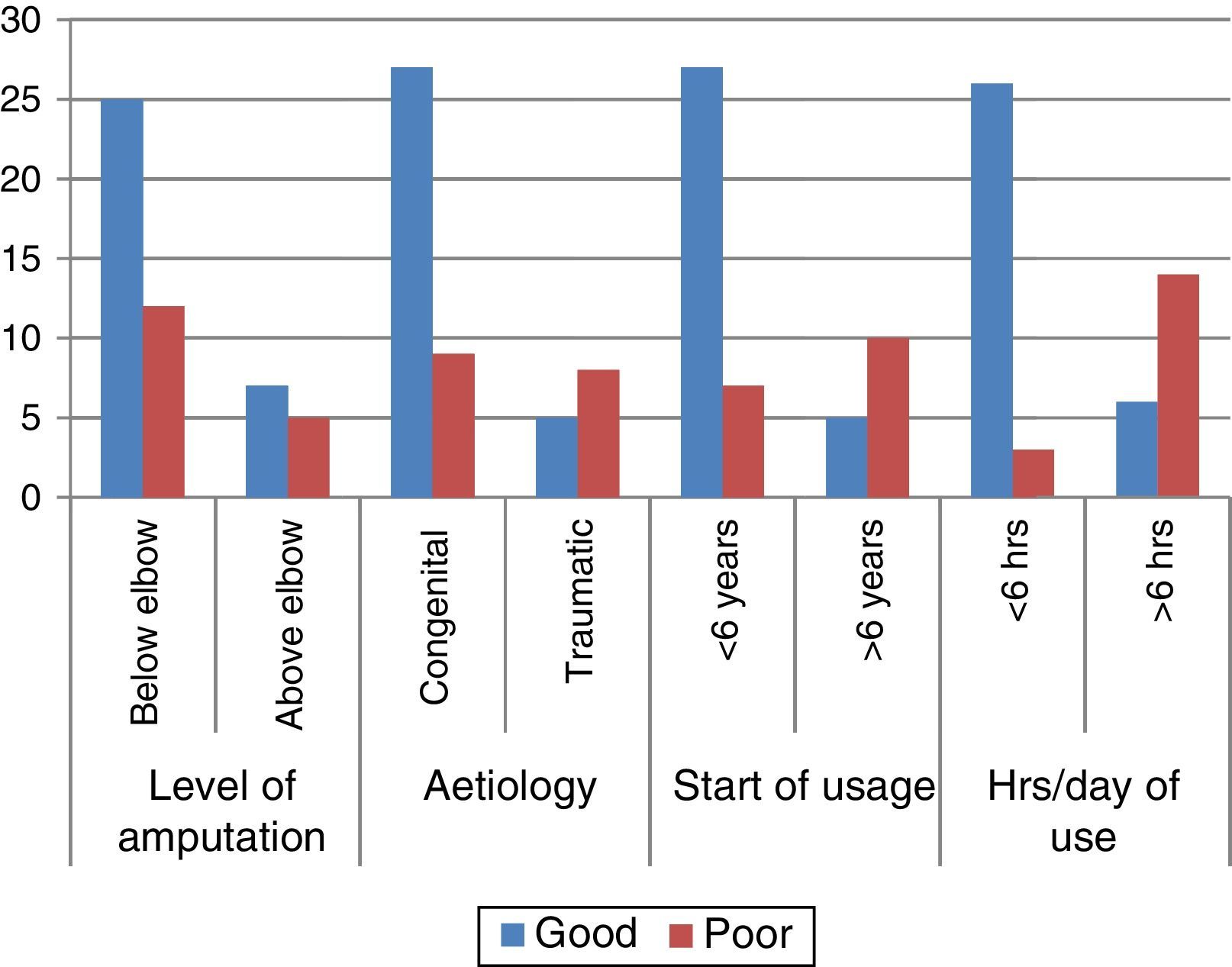
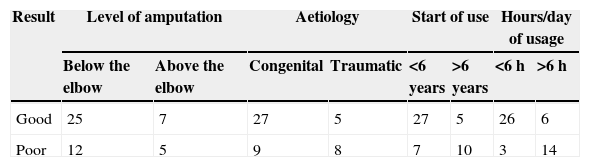
Level of amputationA total of 37 patients had a level of amputation under the elbow (UE) and 12 above the elbow (AE). There were 25 good results among the UE group and 7 among the AE group, with a value of P=.7287. The level of amputation was found not to be significant in predicting a functional result.
Congenital vs traumaticGood results were obtained in 27 congenital cases and 5 traumatic cases, whilst poor results were obtained in 9 congenital cases and 8 traumatic cases, with a value of P=.0383. The level of function presented by patients according to their aetiology was statistically significant (Table 1 and Fig. 2).
Regarding the 49 patients analysed, it was observed that, out of those who started using the prosthesis before the age of 6 years, 27 had a good result and only 7 had a poor result. In addition, out of those who used the prosthesis after the age of 6 years, only 5 had a good result, whilst 10 had a poor result. These results were statistically significant, with a value of P=.0031.
Hours of use per dayIt was observed that, out of the patients who used the prosthesis for more than 6h/day, 26 had a good result and only 3 had a poor result. It was also observed that, out of those who used their prosthesis for less than 6h/day, only 6 had a good functional result and 14 had a poor result, with a value of P<.0001.
DiscussionAlthough it is true that prostheses contribute to social acceptance and certain special activities, there is still considerable controversy regarding the benefits of adapting an upper limb prosthesis in children, particularly in unilateral amputations below the elbow, since the levels of function and quality of life observed are very close to normal. This questions the practice of routinely adapting such prostheses.8
This study managed to establish the prognostic variables to help determine a satisfactory functional result with greater precision in proximal forearm and transhumeral amputations and shoulder disjoints, as well as to predict which patients could be associated to a higher rate of rejection.
The study by Lerman et al. found an inverse relationship to the level of amputation among groups with high functional demands. However, the general group (activities of daily life) did not show any difference in terms of the level of amputation,9 which is correlated with the findings in our study, where no statistically significant differences were found either between the functional results of the 2 groups, despite our hypothesis that the elbow joint provided patients with a functional advantage to place the terminal device in a better position, as well as increase in activation speed, which would facilitate adaptation and prosthetic usage.
Regarding the age and aetiology leading to the use of a prosthesis, a significant difference was found in the functional result between the 2 groups, with a better function among patients who used the prosthesis because of a congenital aetiology and those who had a prosthesis adapted before the age of 6 years. These findings were correlated with how each patient perceived the environment prior to the use of the prosthesis. We believe that adapting a prosthesis before the age of 6 years allows patients to discover that the use of the prosthesis is beneficial for special activities at the same time as they develop1,10 and allows them to adapt the prosthesis in a better way, making its use indispensable for both common and special activities. These findings are correlated with those reported by Scotland and Galway,3 as well as Brooks and Shaperman,11 who found a higher rate of rejection among patients who started to use the prosthesis after 2 years.
Regarding the aetiology, we believe that it is related to the fact that children with congenital deficiencies do not have a sense of loss,12 thus making it easier to adapt a mechanism which allows them to increase their functional level. That is not the case in patients with traumatic amputations, who had a prior functional level, and are now introduced to a mechanism affecting the performance of previously known daily activities with associated activation mechanisms, thus hindering adaptation and the attainment of a level of function close to normality.
A significant level of association was identified regarding the number of hours which the patient used the prosthesis for with a satisfactory functional result: those patients who used the prosthesis for over 6h presented a functional level close to normality. We believe that this is related to an adequate functional adaptation which leads to individuals using the prosthesis for a longer time, since it increases the functional level and promotes social integration and acceptance by peers.13
ConclusionsThe use of upper limb prostheses and their acceptance by patients has been and continues to be a controversial topic, particularly in children, in whom the rate of rejection is high. There have been numerous studies and speculations regarding which patients will benefit from their use, since a large proportion of patients do not obtain functional gains through the use of a prosthesis. Although it is true that upper limb prostheses do not only generate a functional gain, but also promote social adaptation and feeling of normality, nevertheless, a large proportion of children and parents report discouraging functional results.
The present study was able to establish factors that may guide physicians and relatives when making a decision according to their needs and predict a prognosis regarding the functional result of using an upper limb prosthesis. In this study we have been able to observe greater functional gains among patients with congenital deficiencies, in whom introduction and psychological management took place before the age of 6. We also observed better function among those patients who used the prosthesis for a longer period per day, leading to a lower rate of rejection.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Dabaghi-Richerand A, Haces-García F, Capdevila-Leonori R. Factores pronósticos de un resultado funcional satisfactorio en pacientes con amputaciones unilaterales de extremidad superior por arriba de la muñeca que utilizan próstesis de extremidad superior. Rev Esp Cir Ortop Traumatol. 2015;59:343–347.