The most common cause of osteoarthritis of the ankle is post-traumatic, and although tibiotalar arthrodesis remains the surgical gold standard, a number of techniques have been described to preserve joint mobility, such as joint distraction arthroplasty or arthrodiastasis.
ObjectiveTo evaluate the functional outcome and changes in Visual Analog Scale (VAS) for pain after the application of the distraction arthroplasty for post-traumatic ankle osteoarthritis.
Patients and methodsA prospective comparative study of a group of 10 young patients with post-traumatic ankle osteoarthritis treated by synovectomy and arthrodiastasis, compared to a control group of 10 patients treated by isolated synovectomy. Results were calculated using the AOFAS scale and the VAS for pain before and after treatment.
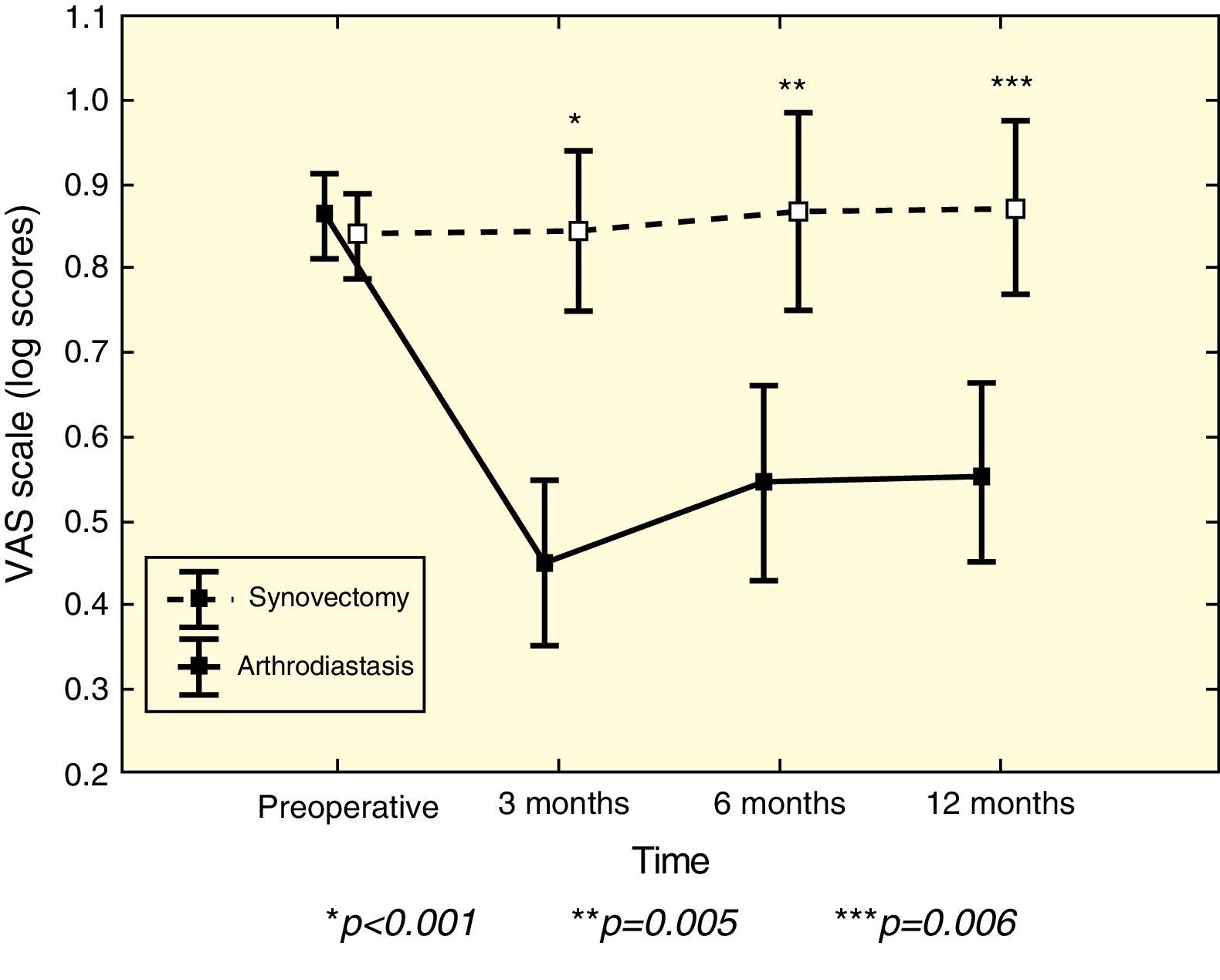
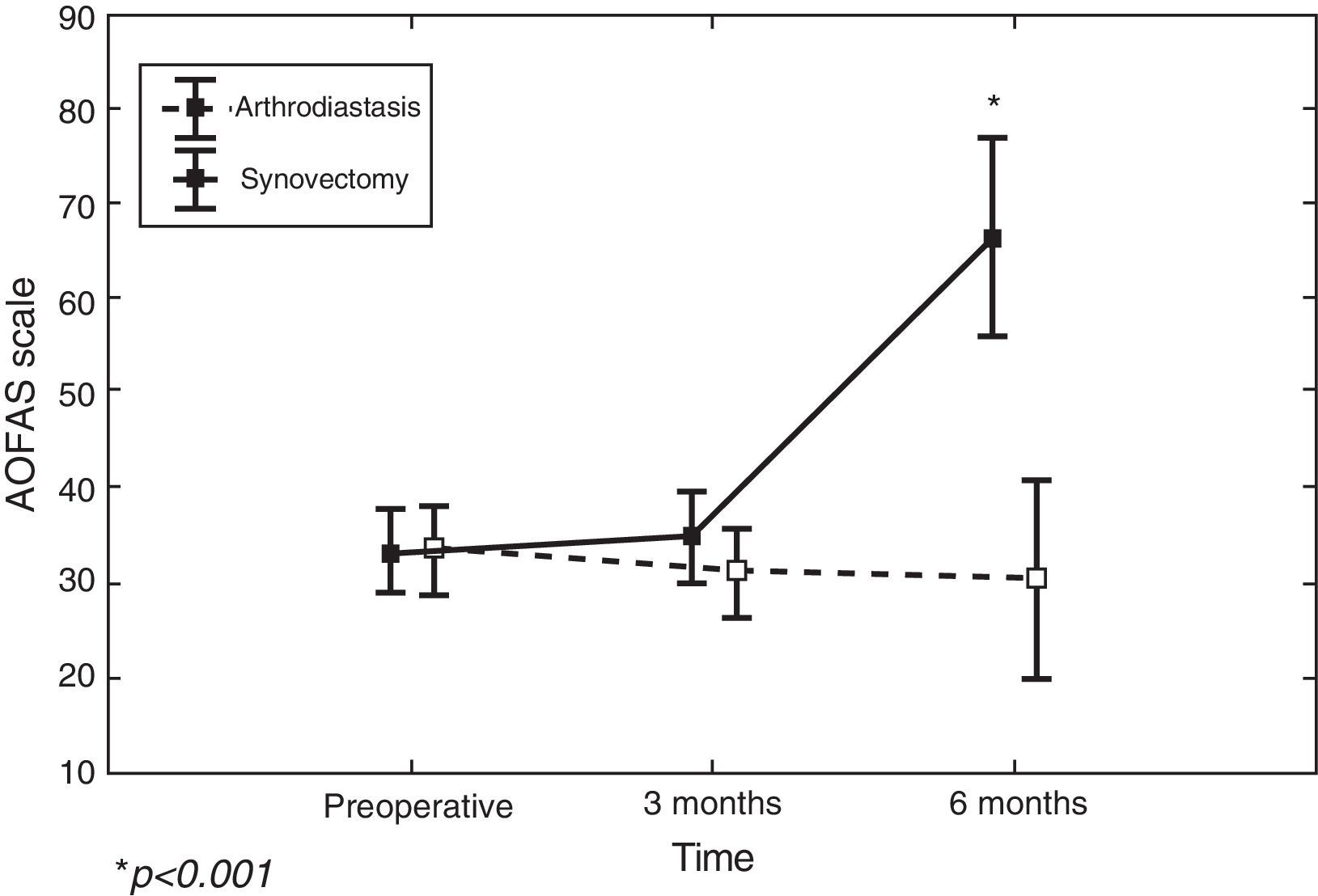
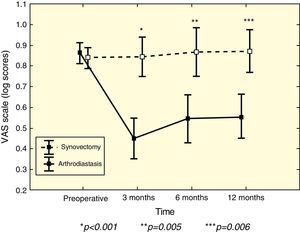
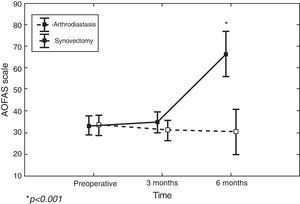
ResultsAs regards the pain measured by VAS, no difference was observed between the two groups before surgery (P=.99), but there was a difference at 3 months (P<.001), 6 months (P=.005), and 12 months (P=.006). No differences were observed in the AOFAS scale between the two groups before surgery (P=.99), or at 3 months (P<.99), but there was a difference at 6 months (P<.001).
ConclusionsAnkle arthrodiastasis is effective in reducing pain in post-traumatic ankle arthropathy, and is superior to isolated synovectomy.
La causa más frecuente de la artrosis de tobillo en nuestro medio es postraumática y, aunque la artrodesis tibioastragalina sigue siendo el tratamiento quirúrgico de elección, se han descrito numerosas técnicas que preservan la movilidad articular, como la distracción articular.
ObjetivoEvaluar el resultado funcional y los cambios en la escala visual analógica (EVA) para el dolor tras la aplicación de la artrodiastasis en la artropatía postraumática de tobillo.
Pacientes y métodosEstudio prospectivo comparativo de un grupo de 10 pacientes jóvenes con artrosis postraumática de tobillo tratados con sinovectomía+artrodiastasis, frente a un grupo control tratado con sinovectomía aislada. Se calcularon los resultados de las escalas AOFAS y EVA para el dolor, antes y después del tratamiento.
ResultadosRespecto al dolor medido por la EVA, no se observó diferencia precirugía entre ambos grupos (p=0,99), pero sí a los 3 meses (p<0,001), a los 6 meses (p=0,005) y a los 12 meses (p=0,006). Respecto a la escala AOFAS, no se observó diferencia precirugía entre ambos grupos (p=0,99), ni a los 3 meses (p<0,99), pero sí a los 6 meses (p<0,001).
ConclusionesLa artrodiastasis de tobillo resulta eficaz en la disminución del dolor en la artropatía postraumática de tobillo y es superior a la sinovectomía aislada.
The ankle joint supports the greatest load per unit area in the whole organism, and is the most often injured. However, symptomatic osteoarthritis of this joint is not as clinically prevalent compared to other joints supporting load.1,2 The true prevalence of ankle osteoarthritis is difficult to determine given its considerable clinical-radiographic variability1,3: radiographic, clinical and cadaver studies suggest that it is less common than in the knee and hip, and, in clinical practice, symptomatic gonarthrosis is 8–9 times more common than symptomatic ankle osteoarthritis. Total knee arthroplasties are approximately 24 times more common than ankle arthrodesis and arthroplasty procedures combined.1 Nevertheless, the late developmental stages of ankle osteoarthritis are very disabling and can cause the same effects on quality of life as severe coxarthrosis.4 The most common cause of ankle osteoarthritis is trauma, responsible for 70% of cases,3 caused by intra-articular fractures or secondary to unresolved chronic instability. Tibiotalar arthrodesis is currently the surgical technique of choice.5 However, altered gait pattern, overload of neighboring joints,6–9 and the rate of pseudoarthrosis (or nonunion) (5–35%) make this a less appropriate option for young and active patients.9–14 Moreover, total ankle arthroplasty offers, at least theoretically, certain advantages over arthrodesis.15,16 Unfortunately, some concerns about the wear and long-term survival of the implant have led this procedure to be carried out in very selected cases.17,18
In the absence of encouraging long-term results of total ankle arthroplasty procedures in young and active patients, multiple techniques following the philosophy of joint preservation19 have been described for these patients with high functional requirements who do not wish to undergo arthrodesis on their ankle. Joint distraction or arthrodiastasis is one of these techniques.
Joint distraction arthroplasty or arthrodiastasis is not a new method in the treatment of ankle osteoarthritis.20 Judet developed it for this joint in the 70s, following the positive initial results obtained in the hip.20 The technique was revived later, based on the studies by van Valburg et al.,21,22 who obtained satisfactory, medium-term results.
There are many theories that explain the beneficial effect of joint distraction on the tibiotalar cartilage; intraarticular pressure variations produced by cyclic partial load appear to promote reparative phenomena in the cartilage,23 which are also favored by the tibiotalar movement allowed by articulated external fixation. Furthermore, it has been reported that subchondral sclerosis decreases during distraction, as mechanical stress on the cartilage during load is reduced.24–26 Our working hypothesis was to assess whether arthrodiastasis is a valid treatment alternative for posttraumatic ankle arthropathy, evaluating the functional outcome and the degree of pain in 10 young patients undergoing synovectomy, debridement and arthrodiastasis, compared to another group of 10 patients treated only by synovectomy and debridement.
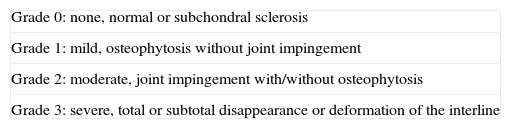
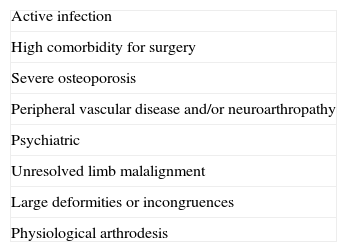
Patients and methodsThis was a prospective comparative study of 2 groups of young patients suffering posttraumatic ankle osteoarthritis who underwent surgery in the period between July 2010 and October 2012. The inclusion criteria were: symptomatic posttraumatic osteoarthritis in stage 2 or less according to the van Dijk classification27 (Table 1), pain level greater than 5 on a visual analog scale (VAS), failure to control pain with powerful pain medication (third analgesic step of the WHO), signing of the corresponding informed consent form for surgery and absence of contraindications for arthrodiastasis (Table 2).
Van Dijk radiographic classification of ankle osteoarthritis.
| Grade 0: none, normal or subchondral sclerosis |
| Grade 1: mild, osteophytosis without joint impingement |
| Grade 2: moderate, joint impingement with/without osteophytosis |
| Grade 3: severe, total or subtotal disappearance or deformation of the interline |
The distribution of patients into each group was carried out after rejection of tibiotalar arthrodesis (which was the first choice for young patients in our center) and after informing patients of the therapeutic options available: joint debridement+synovectomy plus application of an external fixator or else only debridement+synovectomy.
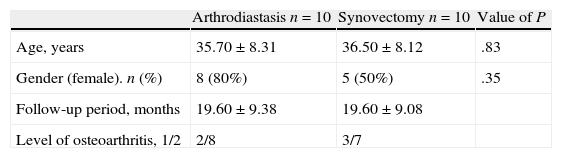
The first group, or “arthrodiastasis group”, included 10 patients (8 females and 2 males). The mean age was 35.7 years (range: 22–47 years) and the mean follow-up period was 19.6 months (range: 6–33 months).
The second group, or “synovectomy group”, included 10 patients (5 females and 5 males). The mean age at the time of inclusion in the study was 36.5 years (range: 23–47 years) and the mean follow-up period was also 19.6 months (range: 6–33 months).
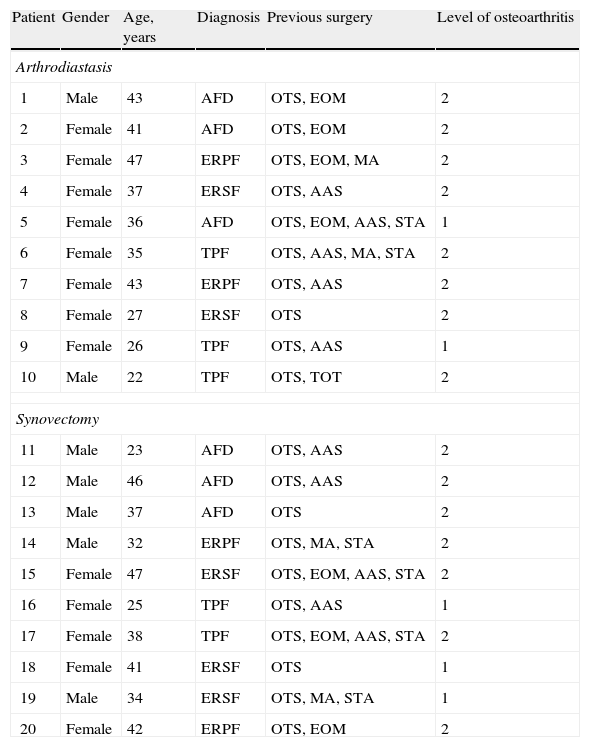
Tables 3 and 4 reflect the diagnoses, previous surgeries, degree of osteoarthritis and other characteristics of both groups.
Characteristics of patients.
| Patient | Gender | Age, years | Diagnosis | Previous surgery | Level of osteoarthritis |
| Arthrodiastasis | |||||
| 1 | Male | 43 | AFD | OTS, EOM | 2 |
| 2 | Female | 41 | AFD | OTS, EOM | 2 |
| 3 | Female | 47 | ERPF | OTS, EOM, MA | 2 |
| 4 | Female | 37 | ERSF | OTS, AAS | 2 |
| 5 | Female | 36 | AFD | OTS, EOM, AAS, STA | 1 |
| 6 | Female | 35 | TPF | OTS, AAS, MA, STA | 2 |
| 7 | Female | 43 | ERPF | OTS, AAS | 2 |
| 8 | Female | 27 | ERSF | OTS | 2 |
| 9 | Female | 26 | TPF | OTS, AAS | 1 |
| 10 | Male | 22 | TPF | OTS, TOT | 2 |
| Synovectomy | |||||
| 11 | Male | 23 | AFD | OTS, AAS | 2 |
| 12 | Male | 46 | AFD | OTS, AAS | 2 |
| 13 | Male | 37 | AFD | OTS | 2 |
| 14 | Male | 32 | ERPF | OTS, MA, STA | 2 |
| 15 | Female | 47 | ERSF | OTS, EOM, AAS, STA | 2 |
| 16 | Female | 25 | TPF | OTS, AAS | 1 |
| 17 | Female | 38 | TPF | OTS, EOM, AAS, STA | 2 |
| 18 | Female | 41 | ERSF | OTS | 1 |
| 19 | Male | 34 | ERSF | OTS, MA, STA | 1 |
| 20 | Female | 42 | ERPF | OTS, EOM | 2 |
AAS: arthroscopic ankle surgery; AFD: ankle fracture-dislocation; EOM: extraction of osteosynthesis material; ERPF: external rotation-pronation fracture; ERSF: external rotation-supination fracture; MA: mobilization under anesthesia; OTS: osteosynthesis; STA: Strayer; TOT: tibial osteotomy; TPF: tibial pilon fracture.
All surgeries were performed by the same surgeon (MHP) in 2 different centers. All operations were performed under spinal anesthesia, antibiotic prophylaxis (intravenous cefazolin 2g) and preventive lower limb ischemia.
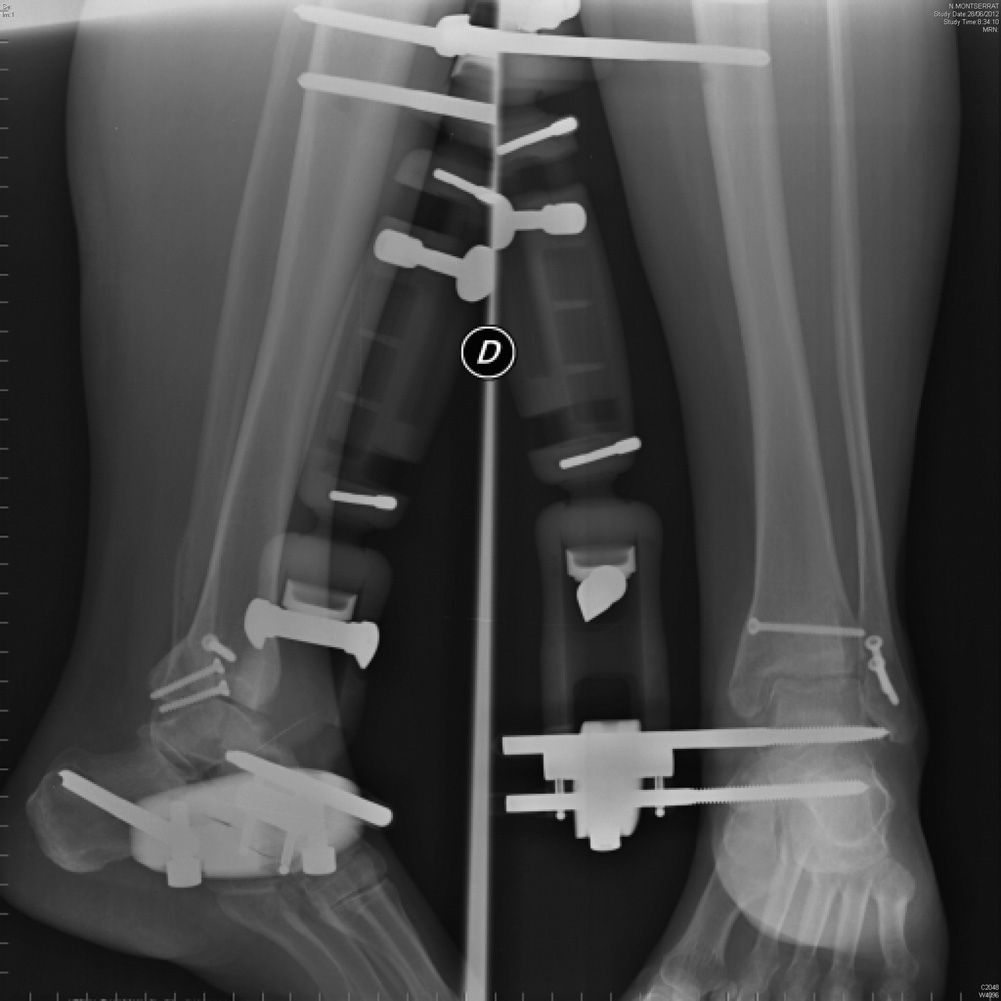
With the patient in the supine position, in the “arthrodiastasis group” we conducted the first stage on the joint through anteromedial miniarthromy (7 cases) or standard arthroscopic approach (3 cases), performing microfracture techniques on exposed cartilage areas (grade IV chondropathy), synovectomy, anterior cheilectomy (7 cases) and extraction of loose bodies plus profuse joint lavage with saline solution. Subsequently, we applied the external fixator (XCaliber, Orthofix®) using 3 proximal and 2 distal tibial nails (1 in the talus and 1 in the calcaneus) (Fig. 1).
After successful placement of the nails we proceeded to progressive and calibrated distraction of 5mm under fluoroscopic control, as reported by van Valburg et al.,21,22 who described the surgical standard of this technique and advocated maintaining the fixator for at least 3 months (according to these authors, chondrocytes require 12–20 weeks discharge to be able to regenerate the cartilage matrix). The articulated piece was left totally free from the beginning, in order to allow tibiotalar mobility. In the second group we only applied the articular procedure (6 open and 4 arthroscopic synovectomies).
All patients were administered low molecular weight heparin and were discharged after 24–48h. In the “arthrodiastasis group”, prior to discharge we ensured that the articulated piece allowed free tibiotalar mobility. The procedures associated in the “arthrodiastasis group” were: Strayer procedure (isolated lengthening of the gastrocnemius at the level of the myotendinous junction) in 2 cases and lengthening of the Achilles tendon in 2 cases; in the “synovectomy group” we performed 2 Strayer procedures and 1 lengthening of the Achilles tendon.
Assessment of patientsBefore surgery we recorded the result in the AOFAS scale for the ankle and pain intensity on the VAS for all patients. After surgery we recorded the result in the AOFAS questionnaire at 3 and 6 months and the VAS score at 3, 6 and 12 months. In both groups, the first cure took place after 5 days and subsequently in the corresponding health center, removing the stitches at 2 weeks. In the “arthrodiastasis group”, we insisted on an exquisite care of the nails with diluted hydrogen peroxide as advocated by other authors.20 All arthrodiastasis patients initiated partial load with crutches (20kg) at 10 days after surgery and rehabilitation at 2 weeks. Full load was allowed at 4 weeks, although the use of at least 1 crutch in the contralateral side was recommended. In the “synovectomy group”, partial load was also started at 10 days and total load at 4 weeks after the procedure. Radiographs were obtained at 6 weeks and at 3, 6 and 12 months of evolution in all cases, except for the last 2 (intervened in October 2012).
Statistical analysisWe used the software package SPSS® for Windows® version 14.0 (SPSS Inc., Chicago, IL, USA) for the descriptive statistical study.
The results of the categorical variables were expressed as frequencies and percentages, while quantitative variables were expressed as means and standard deviations. Comparisons of proportions were performed using the Chi-square or Fisher's exact tests, as appropriate. Comparisons of means between treatments for age and follow-up time were performed with Student's t test. Verifications of normality for age, follow-up time, VAS scores and AOFAS scores within each group were performed using the Kolmogorov–Smirnov test. Due to its lack of normality, the VAS variable was transformed with logarithms. Comparisons between treatments (arthrodiastasis/synovectomy) between the study periods (pretreatment, 3, 6 and 12 months) and AOFAS scale scores (pretreatment, 3 and 6 months) were performed using repeated measures ANOVA. Comparisons of means a posteriori were performed with the Scheffé test.
ResultsRegarding the demographic and clinical characteristics of patients, there were no significant differences in age, gender, follow-up or degree of osteoarthritis (the majority of cases were van Dijk level 2) (Table 3). Regarding the intensity of pain as measured by VAS, there was a significant interaction between the type of treatment and measuring periods (F3.54=19.6; P<.001). We found no difference between both types of treatment preoperatively (P=0.99), but we did find it at 3 months (P<.001), 6 months (P=.005) and 12 months (P=.006) (Fig. 2). Thus, the VAS result at 1 year decreased by a mean total of 2.3 points in over 70% of patients in the “arthrodiastasis group” compared to a mean increase of 3.8 points in the “synovectomy group”.
Regarding the clinical outcomes recorded through the AOFAS scale, the interaction between type of treatment and measurement periods was significant (F2.36=29.0; P<.001). There was no difference between both types of treatment preoperatively (P=.99) or at 3 months (P<.99), but it was observed at 6 months (P<.001) (Fig. 3).
We only registered 5 complications in our series: 2 intolerances to nails, 1 type I reflex sympathetic dystrophy syndrome in the “arthrodiastasis group” (of these, 1 case of intolerance led to removal of the nails before 3 months while the rest of patients evolved favorably) and 2 partial wound dehiscences in the “synovectomy group”, with no impact on the final results.
In the “arthrodiastasis group”, 8 patients were clinically stabilized, while the remaining 2 presented poor outcomes (worse results on the AOFAS and VAS scales) and required arthrodesis (tibiotalar in one case and tibiotalocalcaneal in the other).
In the “synovectomy group”, 3 cases were stabilized and 7 patients evolved unfavorably: 5 required tibiotalar arthrodesis, 1 patient underwent implantation of an ankle prosthesis and 1 case was treated at the Pain Unit because he rejected a new surgical intervention.
DiscussionAnkle degenerative arthropathy in the young and active population represents a therapeutic challenge for orthopedic surgeons. The main cause in our environment is trauma, in 70% of cases, and from the practical point of view we wish to call attention to seemingly trivial bimalleolar fractures, present in our series in 15 of the 20 cases. Multiple studies have shown how minor defects in the reduction of these fractures inevitably lead to posttraumatic osteoarthritic changes.28–30 Therefore, we must be scrupulous in our treatment in order to prevent intractable, degenerative sequelae. But not only incorrect reduction predisposes toward osteoarthritis: up to 14% of ankle fractures and 25% of ankle fracture-dislocations (found in 6 cases in our series) present posttraumatic degenerative changes in the first 2 years of follow-up despite anatomical reduction.31 This is likely related to cartilage damage sustained at the time of injury. As demonstrated by Hintermann et al., as many as 79% of patients with ankle fractures who underwent arthroscopy at the time of treatment suffered some kind of chondral lesion, especially patients with Lauge-Hansen32 pronation/external rotation (PER) fracture patterns, which were present in 4 cases in our series (2 in each group), all of them with poor results.
There is currently controversy regarding the ideal treatment for posttraumatic ankle osteoarthritis in the young and active population, due to the high functional requirements and life expectancy of this population group.19 Surgical procedures which preserve the joint may be effective in patients with moderate osteoarthritis,19,20 but only arthrodesis and total ankle arthroplasty have shown acceptable results in the medium and long term. Nevertheless, the rates of nonunion and overload of neighboring joints in the first procedure have been widely reported,8,9,15 as have loosening and other complications associated with the implantation of an arthroplasty in the second procedure.15–18,33
Understood as a last option before considering treatments which sacrifice the original ankle joint, arthrodiastasis can represent a valid alternative in this group of patients who wish to preserve mobility. The first retrospective study on ankle arthrodiastasis was published in 199521: 11 patients with a mean age of 35 years who were candidates for arthrodesis and who received treatment with an Ilizarov circular external fixator with distraction of 5mm for 3 months. Partial load was allowed after a few days and the fixator was articulated to allow flexion and extension from week 6. At 20 months follow-up, all patients presented decreased pain, 5 were without pain, mobility improved over 50% and 3 patients even presented an increase in joint space. In 2002, Marijnissen et al. published a prospective multicenter study of 57 patients aged under 40 years who were followed for 2.8 years, reporting significant improvement in the functional parameters of 38 patients, although 10 were lost during follow-up, 8 suffered arthrodesis and 1 required total ankle arthroplasty due to an unfavorable evolution.26 Ploegmakers et al. published their results in 27 patients with posttraumatic arthritis, a mean age of 37 years and a monitoring period of 7 years: 73% reported significant improvement in all parameters, while 6 patients suffered arthrodesis.34 However, the functional improvement of this technique has not only been demonstrated in the short term. Paley and Lamm reported that 16 of 22 patients (73%) presented a persistent improvement after 7 years of follow-up after undergoing arthrodiastasis.35
Regarding the type of external fixation, it has been demonstrated that circular external fixation, although technically more complex, is biomechanically superior to monolateral fixation such as was used in our series, as the latter applies unequal distraction on the joint and is difficult to implement correctly in the ankle axis. However, there are some reports with large series of patients using this type of fixation and also showing satisfactory results.20,22,36
In 2003, Marijnissen et al. published a similar study to the present one, although our follow-up period was longer, which showed better results for arthrodiastasis plus debridement versus debridement alone, with higher rates of functional improvement after 1 year.37
Our results regarding pain relief in 70% of cases are consistent with the literature,21,22,24,34–36 and we consider them the main clinical benefit of this surgical procedure.
Moreover, our study clearly shows how patients who evolve favorably begin to experience functional improvement after 5–6 months of joint distraction20 (the differences in the AOFAS scale are significant after 6 months). Based on this fact, we encourage our patients to wait approximately 1 year before deciding to undergo treatments which sacrifice their original joint (arthrodesis or arthroplasty).
Regarding the use of open versus arthroscopic synovectomy, various authors have reported better results with the latter,19,27,38 although in our study we could not find a statistically significant association in this regard.
All patients in both groups with a previous diagnosis of PER-type ankle fracture eventually presented poor results and required either arthrodesis or arthroplasty. Various authors have reported a link between this fracture pattern and a higher incidence of chondral lesions, which could explain the poor results obtained in these patients.31,32
The worst results in the “arthrodiastasis group” were obtained among older patients (47 and 43 years) who had undergone 2 or more previous procedures. Neither result was statistically significant. In the “synovectomy group”, 2 of the 3 patients aged over 40 years presented the worst results, both with more than 2 previous operations, but without statistical significance. Despite not having statistical significance, it seems logical that the age and number of previous surgeries could negatively influence the final result.
Regarding the degree of prior osteoarthritis according to the classification described by van Dijk,27 all our negative results in both groups except for 1 were grade 2, although this fact was not statistically significant.
While not part of our initial objectives, in 4 patients in our series we observed an objective decrease of radiographic subchondral sclerosis after the application of arthrodiastasis. Furthermore, in 1 case with asymmetric impingement and varus axis, this disappeared in the radiographic control after removal of the fixator and remained thus throughout the entire follow-up period (Figs. 4–7). Based on the results of this study, we cannot confirm that arthrodiastasis recovers the joint interline, as we have only evaluated clinical and functional criteria, but it seems clear that this treatment was effective in slowing the progressive radiographic deterioration of the 8 patients in our series, who evolved favorably. This could explain the functional results in these patients, although some studies based on magnetic resonance imaging analysis have shown a recovery of the articular cartilage after the application of this technique.34,35
In 2012, Rodriguez et al.37 published the largest series of patients treated with ankle arthrodiastasis to date. It included 82 patients intervened during the period 1998–2010, with a mean age of 5.6 years (range: 1–12 years), who were evaluated before and after surgery using the Maryland Foot Score functional outcome scale, which is similar to that used in our study (AOFAS), but takes into account other aspects, such as difficulty using ordinary shoes and esthetic aspects. This showed 24% excellent results and 55% good results, that is, over 70% good or excellent results, with 15% moderate results and 6% poor results. Out of the entire series, only 5 patients with a poor outcome required surgery during follow-up: 4 required tibiotalar arthrodesis and 1 required joint replacement. The most common complication was intolerance or infection in the pathway of the nails, in 15% of cases. These results are similar to those in our series. More recently, Smith et al.38 analyzed the levels of evidence existing regarding ankle arthrodiastasis and found that there is not yet sufficient and adequate evidence-based literature to support or refute its use as a valid alternative to arthrodesis or arthroplasty. Further and higher-quality scientific studies, both prospective and comparative, are required to support this technique. One example would be the study we have carried out in order to validate this surgical technique which preserves the joint in young patients.
The main limitations of this study include lack of randomization, although both groups were perfectly comparable in all parameters. We also consider that it would be useful to apply a longer follow-up period (at least in the medium term), in order to validate the results obtained. Furthermore, it would be interesting to incorporate other adjuvant therapies described for ankle arthropathy, such as platelet-rich plasma and viscosupplementation, so as to evaluate whether there are significant differences in treatment groups.
ConclusionsBased on the results obtained in this study, ankle arthrodiastasis represents a valid and promising alternative to be considered for the treatment of posttraumatic ankle arthropathy in young patients. It mainly helped to reduce pain and delay, and even eliminate, the need for fusion or arthroplasty in most of our patients in the short term, and was clinically superior to synovectomy alone.
Moreover, since this technique entails minimal morbidity and does not eliminate the possibility of conducting other surgical treatments in the future, we support it as a therapeutic option for young and active patients who refuse tibiotalar arthrodesis, provided they meet the requirements described in this article for the use of this surgical technique.
Level of evidenceLevel of evidence ii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
This study was initiated in the year 2010, encouraged by the initial positive results obtained by Dr. Fernando Sellers, orthopedic surgeon at Móstoles Hospital, who recently passed away.
Please cite this article as: Herrera-Pérez M, Pais-Brito JL, de Bergua-Domingo J, Aciego de Mendoza M, Guerra-Ferraz A, Cortés-García P, et al. Resultados de la artrodiastasis en la artropatía postraumática de tobillo en población joven: estudio prospectivo comparativo. Rev Esp Cir Ortop Traumatol. 2013;57:409–416.