To identify pre-operative risk factors for surgical delay of more than 2 days after admission in patients older than 65 years with a hip fracture.
Material and methodsA prospective observational study was conducted on 180 hip fractures in patients older than 65 years of age admitted to our hospital from January 2015 to April 2016. The data recorded included, patient demographics, day of admission, pre-fracture comorbidities, mental state, level of mobility and physical function, type of fracture, antiaggregant and anticoagulant medication, pre-operative haemoglobin value, type of treatment, and surgical delay.
ResultsThe mean age of the patients was 83.7 years. The mean Charlson Index was 2.8. The pre-fracture baseline co-morbidities were equal or greater than 2 in 70% of cases. Mean timing of surgery was 3.1 days. At the time of admission, 122 (67.7%) patients were fit for surgery, of which 80 (44.4%) underwent surgery within 2 days. A Charlson index greater than 2, anticoagulant therapy, and admission on Thursday to Saturday, were independently associated with a surgical delay greater than 2 days.
ConclusionsThe rate of hip fracture patients undergoing surgery within 2 days is low. Risk factors associated to surgical delay are non-modifiable. However, their knowledge should allow the development of protocols that can reduce surgical delay in this group of patients.
Identificar los factores al ingreso relacionados con una demora quirúrgica mayor de 2 días en pacientes mayores de 65 años con fractura de cadera.
Material y métodosEstudio de una base de datos prospectiva de pacientes mayores de 65 años con fractura proximal de fémur entre enero de 2015 y abril de 2016. Se incluyeron en el estudio 180 pacientes. Se registraron variables demográficas, día de ingreso, comorbilidades asociadas, estado mental, nivel de deambulación y dependencia, tipo de fractura, toma de medicación anticoagulante o antiagregante, valor de la hemoglobina al ingreso, tipo de tratamiento, y demora quirúrgica.
ResultadosLa edad media de los pacientes fue de 83,7 años. El valor medio del índice de comorbilidad de Charlson era de 2,8; con un 70% de pacientes con al menos 2 comorbilidades. La demora quirúrgica media fue de 3,1 días. En el momento del ingreso, 122 pacientes (67,7%) se consideraron aptos para la intervención quirúrgica. De ellos, 80 pacientes (44,4%) fueron intervenidos en los 2 primeros días tras el ingreso. El análisis multivariante mostraba el índice de comorbilidad de Charlson mayor de 2, la anticoagulación, y el ingreso hospitalario de jueves a sábado, como factores independientes asociados a la demora quirúrgica mayor de 2 días.
ConclusionesEl porcentaje de pacientes con fractura de cadera intervenidos en los 2 primeros días del ingreso hospitalario es bajo. Los factores asociados a la demora quirúrgica no son modificables. Sin embargo, su conocimiento debería permitir el desarrollo de protocolos de actuación que consiguieran reducir la demora quirúrgica en este grupo de pacientes.
Since surgery is the treatment of choice in hip fractures, the influence of the time to surgery on morbimortality following a hip fracture has been extensively studied with a view to identifying the optimal moment for the procedure in order to obtain the best results. Nonetheless, the results published have been contradictory. Various studies and systematic reviews report an association between a time to surgery of less than 48h and morbimortality following hip fracture,1–8 not mentioned by others.9,10 Despite this, some clinical guidelines for the handling of patients with hip fracture recommend that surgery be carried out during the first 2 days following admission to hospital.11–14 The National Health System in Spain establishes surgery for hip fractures in the first 48h following admission to hospital as an indicator of care quality for our hospitals.15
The scenario of a healthy patient with a hip fracture is infrequent. Patients may present significant anaemia and alterations in their hydro-electrolytic balance that must be corrected.12 They generally associate comorbidities requiring stabilization, or else take anticoagulant or anti-platelet medication that must be withdrawn prior to surgery. In consequence, we consider the hypothesis that the percentage of patients with a time to surgery of less than 2 days is low, bearing in mind the characteristics of our patients with hip fracture and the organization of our care services.
The goal of the present study was to investigate the reasons for times to surgery in excess of 48h in patients over 65 years of age with a hip fracture at our department, and to assess the performance of hip fracture surgery procedures in the first 48h following admission to hospital.
Material and methodThe patients over 65 years of age and recorded on our prospective database for proximal femur fractures between January, 2015, and April, 2016, were identified. The exclusion criteria were: aged under 65 years, pathological fracture, polytraumatized patients, simultaneous fractures of both hips, a prior history of hip fracture, and no indication of surgery.
On admission, the age, gender, weight, height, and provenance of the patient and the day of the week were recorded. A body mass index value in excess of 30 was deemed to be obesity. The types of proximal femur fracture were classified as subcapital, intratrochanteric or subtrochanteric.
The presence of associated comorbidities was determined by anamnesis on admission, or through the review of episodes for previous hospital admissions. The comorbidities recorded were: high blood pressure, atrial fibrillation, heart failure, coronary disease, cerebrovascular disease, dementia, epilepsy, Parkinson's disease, chronic obstructive pulmonary disease, asthma, diabetes, rheumatic disease, kidney failure, hypothyroidism, peripheral vascular insufficiency, lung tumour, gastric or duodenal ulcer, liver disease, leukaemia, lymphoma, metastasis, AIDS.4,11–14 The number of comorbidities was determined, as well as the Charlson comorbidity index (CCI),16 and the age-adjusted CCI.17 The taking of anticoagulant and anti-platelet medication was also noted.
The patients’ cognitive status was evaluated using the Mini-Mental State Examination,18 where the maximum score is 10, and a score of 6 or less was indicative of dementia.
The level of deambulation prior to the fracture was assessed using the Parker and Palmer scale,19 with a maximum score of 9. Deambulation was considered to be independent when the score was greater than or equal to 4, indicating that the patient had been able to walk about at home or in the street with the help of a walking stick or unaided. The level of dependence was determined using the Katz index20 based on 6 activities of daily life. A score of 6 determined complete independence for performing all 6 activities, while 5 or 4 points indicated partial dependence, and a score of 3 or less was seen as total dependency.
The haemoglobin (Hb) value on the blood test ordered on admission was noted. A blood transfusion was indicated if Hb was lower than 8g/dl, or if anaemia was symptomatic with values between 8 and 10g/dl.
At the Emergency Department, the patients were assessed by the ER physician and by the orthopaedic surgeon. Once an X-ray examination of the chest, pelvis and hip affected had been requested, along with an electrocardiogram and a blood test, their medication was adjusted and they were admitted to hospital. In the hospital ward, all patients were included in the pre-operative and post-operative acute assistance programme shared between orthopaedic surgeons and a specific team of internal medicine specialists. The surgical technique indicated depended on the fracture type: osteosynthesis with cannulated screws in non-displaced subcapital fractures; cemented partial bipolar prosthesis in displaced subcapital fractures; and endomedullary pins in intratrochanteric and subtrochanteric fractures. All patients undergoing surgery were given spinal anaesthesia. Antibiotic prophylaxis (i.v. cephazolin: 2g prior to the procedure and 1g every 8h for 3 doses post-operatively; in allergic patients, i.v. vancomycin: 1g pre-operatively and a single 1g post-operative dose) and anti-thrombotic prophylaxis (s.c. enoxaparin: 40U every 24h until one month after the procedure) were identical in all cases. A post-surgery analytical check-up was requested 24h after the procedure. Patients were allowed to sit up in armchairs after 24–48h and subsequently deambulation with a walking frame. Once the patients’ general status had returned to normal after treatment, they were discharged from hospital to continue with appropriate care at their own home or in a residential institution.
The time to surgery was considered to be the days that elapsed between admission and the surgical procedure. This variable was categorized into 2 groups: less than or equal to 2 days, and greater than 2 days. The Anaesthesiology and Reanimation Department established this surgical delay on the basis of the need to stabilize the patient prior to surgery, or the taking of anticoagulant or anti-platelet medication. Acetylsalicylic acid at 100mg was not grounds for surgical delay. The reasons for times to surgery in excess of 2 days were classified as: (1) the need to withdraw anticoagulant or anti-platelet medication; (2) stabilization of associated comorbidities, and (3) non-availability of an operating theatre for the surgical procedure.
Statistical analysisThe statistical analysis was carried out using version 18.0 of the SPSS computer programme (SPSS Inc., Chicago, U.S.A.). The Kolmogorov–Smirnov test was used to determine whether the data conformed to a normal distribution. Quantitative variables were presented as means with their standard deviation, while qualitative variables were displayed as percentages. Comorbidities were adjusted as dichotomic variables, i.e. whether or not they were present. For the statistical analysis, several variables were redefined. Age was classified into 3 groups: less than or equal to 84 years of age, between 85 and 89, and equal to or greater than 90 years of age. The day of admission was classified as either from Thursday to Saturday, or else from Sunday to Wednesday. Fracture types used were intracapsular (subcapital fracture) or extracapsular (intratrochanteric and subtrochanteric fractures). The number of comorbidities was divided into less than or equal to 2, or else greater than 2. The CCI value was less than or equal to 2, or else greater than 2. The age-adjusted CCI was less than or equal to 6, or else greater than 6. Hb on admission was equal to or greater than 10g/dl, or else less than 10g/dl.
A univariate analysis was made on the variables at admission and on the time to surgery in excess of 2 days. For the qualitative variables, the χ2 test was used with Yates's correction depending on whether or not the Mantel-Haenszel parametric test was required. For continuous variables, Student's t test was performed independently or in pairs depending on whether the Mann–Whitney non-parametric tests or Wilcoxon's signs were applied. In the case of univariate tests with a significant relationship, these were used as independent co-variants in a multivariate logistic regression analysis using the “Insert” procedure with respect to time to surgery in excess of 2 days as the dependent variable. Values of p less than or equal to 0.05 were considered significant, and the odds ratio (OR) was calculated with a 95% confidence interval (CI).
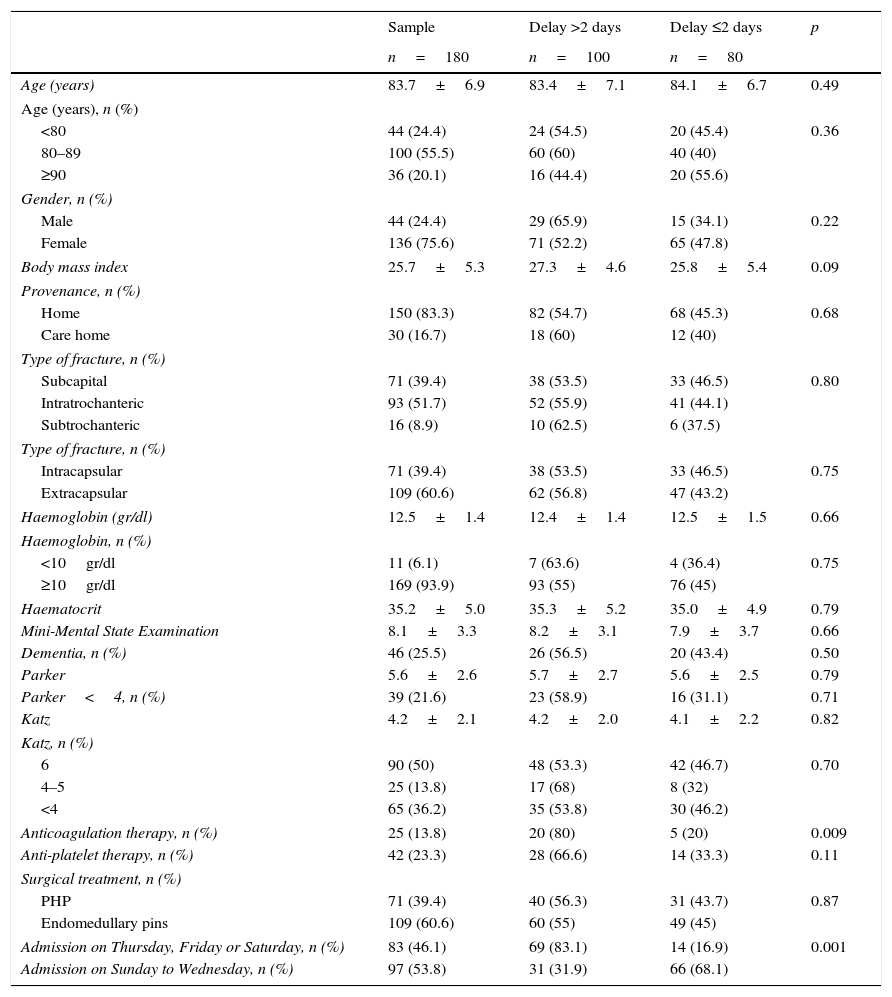
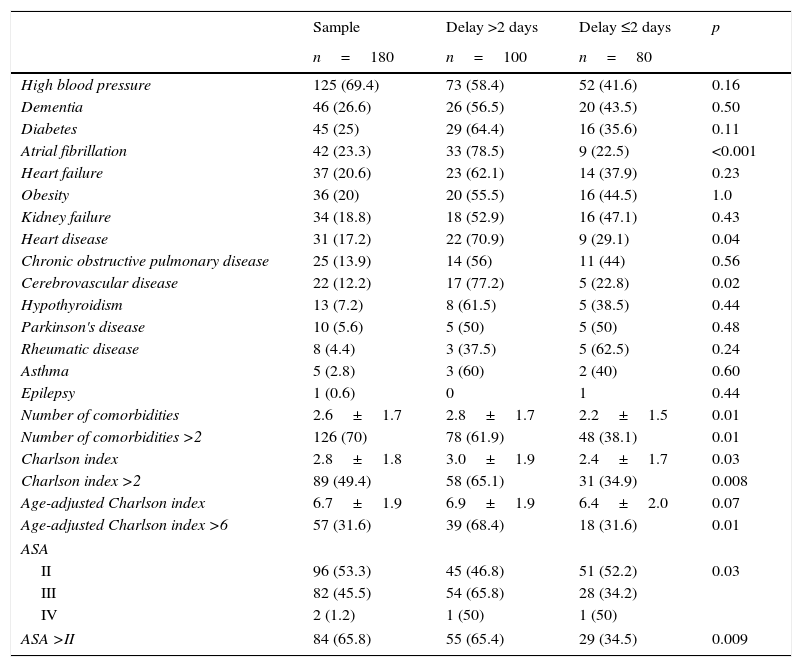
ResultsDuring the period under study, 202 patients were admitted to our department with a proximal fracture of the femur. Of these, 22 patients were excluded: 12 due to being under 65 years of age, 8 due to non-surgical treatments, and 2 due to demise prior to surgery; leaving a total of 180 patients. The mean age of the females was 83.9 years (SD 6.6) and that of the males was 83.3 years (SD 7.8) (p=0.60). The general data and comorbidities in the series are shown in Tables 1 and 2.
General variables and time to surgery.
| Sample | Delay >2 days | Delay ≤2 days | p | |
|---|---|---|---|---|
| n=180 | n=100 | n=80 | ||
| Age (years) | 83.7±6.9 | 83.4±7.1 | 84.1±6.7 | 0.49 |
| Age (years), n (%) | ||||
| <80 | 44 (24.4) | 24 (54.5) | 20 (45.4) | 0.36 |
| 80–89 | 100 (55.5) | 60 (60) | 40 (40) | |
| ≥90 | 36 (20.1) | 16 (44.4) | 20 (55.6) | |
| Gender, n (%) | ||||
| Male | 44 (24.4) | 29 (65.9) | 15 (34.1) | 0.22 |
| Female | 136 (75.6) | 71 (52.2) | 65 (47.8) | |
| Body mass index | 25.7±5.3 | 27.3±4.6 | 25.8±5.4 | 0.09 |
| Provenance, n (%) | ||||
| Home | 150 (83.3) | 82 (54.7) | 68 (45.3) | 0.68 |
| Care home | 30 (16.7) | 18 (60) | 12 (40) | |
| Type of fracture, n (%) | ||||
| Subcapital | 71 (39.4) | 38 (53.5) | 33 (46.5) | 0.80 |
| Intratrochanteric | 93 (51.7) | 52 (55.9) | 41 (44.1) | |
| Subtrochanteric | 16 (8.9) | 10 (62.5) | 6 (37.5) | |
| Type of fracture, n (%) | ||||
| Intracapsular | 71 (39.4) | 38 (53.5) | 33 (46.5) | 0.75 |
| Extracapsular | 109 (60.6) | 62 (56.8) | 47 (43.2) | |
| Haemoglobin (gr/dl) | 12.5±1.4 | 12.4±1.4 | 12.5±1.5 | 0.66 |
| Haemoglobin, n (%) | ||||
| <10gr/dl | 11 (6.1) | 7 (63.6) | 4 (36.4) | 0.75 |
| ≥10gr/dl | 169 (93.9) | 93 (55) | 76 (45) | |
| Haematocrit | 35.2±5.0 | 35.3±5.2 | 35.0±4.9 | 0.79 |
| Mini-Mental State Examination | 8.1±3.3 | 8.2±3.1 | 7.9±3.7 | 0.66 |
| Dementia, n (%) | 46 (25.5) | 26 (56.5) | 20 (43.4) | 0.50 |
| Parker | 5.6±2.6 | 5.7±2.7 | 5.6±2.5 | 0.79 |
| Parker<4, n (%) | 39 (21.6) | 23 (58.9) | 16 (31.1) | 0.71 |
| Katz | 4.2±2.1 | 4.2±2.0 | 4.1±2.2 | 0.82 |
| Katz, n (%) | ||||
| 6 | 90 (50) | 48 (53.3) | 42 (46.7) | 0.70 |
| 4–5 | 25 (13.8) | 17 (68) | 8 (32) | |
| <4 | 65 (36.2) | 35 (53.8) | 30 (46.2) | |
| Anticoagulation therapy, n (%) | 25 (13.8) | 20 (80) | 5 (20) | 0.009 |
| Anti-platelet therapy, n (%) | 42 (23.3) | 28 (66.6) | 14 (33.3) | 0.11 |
| Surgical treatment, n (%) | ||||
| PHP | 71 (39.4) | 40 (56.3) | 31 (43.7) | 0.87 |
| Endomedullary pins | 109 (60.6) | 60 (55) | 49 (45) | |
| Admission on Thursday, Friday or Saturday, n (%) | 83 (46.1) | 69 (83.1) | 14 (16.9) | 0.001 |
| Admission on Sunday to Wednesday, n (%) | 97 (53.8) | 31 (31.9) | 66 (68.1) | |
Quantitative variables are given as mean±standard deviation.
PHP: partial hip prosthesis.
Comorbidities and time to surgery.
| Sample | Delay >2 days | Delay ≤2 days | p | |
|---|---|---|---|---|
| n=180 | n=100 | n=80 | ||
| High blood pressure | 125 (69.4) | 73 (58.4) | 52 (41.6) | 0.16 |
| Dementia | 46 (26.6) | 26 (56.5) | 20 (43.5) | 0.50 |
| Diabetes | 45 (25) | 29 (64.4) | 16 (35.6) | 0.11 |
| Atrial fibrillation | 42 (23.3) | 33 (78.5) | 9 (22.5) | <0.001 |
| Heart failure | 37 (20.6) | 23 (62.1) | 14 (37.9) | 0.23 |
| Obesity | 36 (20) | 20 (55.5) | 16 (44.5) | 1.0 |
| Kidney failure | 34 (18.8) | 18 (52.9) | 16 (47.1) | 0.43 |
| Heart disease | 31 (17.2) | 22 (70.9) | 9 (29.1) | 0.04 |
| Chronic obstructive pulmonary disease | 25 (13.9) | 14 (56) | 11 (44) | 0.56 |
| Cerebrovascular disease | 22 (12.2) | 17 (77.2) | 5 (22.8) | 0.02 |
| Hypothyroidism | 13 (7.2) | 8 (61.5) | 5 (38.5) | 0.44 |
| Parkinson's disease | 10 (5.6) | 5 (50) | 5 (50) | 0.48 |
| Rheumatic disease | 8 (4.4) | 3 (37.5) | 5 (62.5) | 0.24 |
| Asthma | 5 (2.8) | 3 (60) | 2 (40) | 0.60 |
| Epilepsy | 1 (0.6) | 0 | 1 | 0.44 |
| Number of comorbidities | 2.6±1.7 | 2.8±1.7 | 2.2±1.5 | 0.01 |
| Number of comorbidities >2 | 126 (70) | 78 (61.9) | 48 (38.1) | 0.01 |
| Charlson index | 2.8±1.8 | 3.0±1.9 | 2.4±1.7 | 0.03 |
| Charlson index >2 | 89 (49.4) | 58 (65.1) | 31 (34.9) | 0.008 |
| Age-adjusted Charlson index | 6.7±1.9 | 6.9±1.9 | 6.4±2.0 | 0.07 |
| Age-adjusted Charlson index >6 | 57 (31.6) | 39 (68.4) | 18 (31.6) | 0.01 |
| ASA | ||||
| II | 96 (53.3) | 45 (46.8) | 51 (52.2) | 0.03 |
| III | 82 (45.5) | 54 (65.8) | 28 (34.2) | |
| IV | 2 (1.2) | 1 (50) | 1 (50) | |
| ASA >II | 84 (65.8) | 55 (65.4) | 29 (34.5) | 0.009 |
The values for variables are expressed as n (%) or as the mean±standard deviation.
ASA: American Society of Anaesthesiologists.
The indications for anti-platelet treatment were cardiac pathology in 21 patients, cerebrovascular disease in 12, and other indications in 9. The anti-platelet medication prescribed were 100mg acetylsalicylic acid in 31 patients, clopidogrel in 6, triflusal in 3, prasugrel in 1, ticlopidine in 1.
Indications for anticoagulation therapy were cardiac pathology in 22 patients, and cerebrovascular illness in 3. The anticoagulants prescribed were acenocoumarol in 20 patients, rivaroxaban in 3, and dabigatran in 2.
The distribution of admissions over the days of the week was as follows: 18 patients (10%) on Monday, 22 (12.2%) on Tuesday, 30 (16.7%) on Wednesday, 26 (14.4%) on Thursday, 28 (15.6%) on Friday, 29 (16.1%) on Saturday, and 27 (15%) on Sunday.
The mean time to surgery was 3.16 days (SD 2.0; range 1–10). At the moment of admission, 122 patients (67.7%) were considered suitable candidates for the surgical procedure. Eighty patients (44.4%) were operated on in the first 2 days after admission, and the other 100 (55.6%) on the third or later day after admission. The reasons for the times to surgery over 2 days were the need to withdraw anticoagulant or anti-platelet medication in 25 patients (13.8%), the need to stabilize medical comorbidities in 33 patients (18.3%), and the non-availability of an operating theatre in 42 (23.3%). With respect to those patients whose surgery was delayed due to the non-availability of an operating theatre, 11 (26.1%) were admitted on a Thursday, 17 (40.4%) on a Friday, and 14 (33.5%) on a Saturday. The mean time to surgery in patients undergoing anticoagulation therapy was 4.0 days (SD 1.1; range 3–6); in patients with anti-platelet medication, it was 4.7 days (SD 1.2; range 4–10); in patients requiring stabilization of comorbidities, it was 4.1 days (SD 0.6; range 3–10); and in patients where an operating theatre was not available, it was 3.2 days (SD 0.44; range 3–4).
In the univariate analysis, hospital admission from Thursday to Saturday (OR: 3.94; 95% CI: 2.40–6.45) and anticoagulation (OR: 3.20; 95% CI: 1.25–8.15) were significantly associated with a time to surgery in excess of 2 days (Table 1). With respect to the comorbidities on admission, patients with the presence of atrial fibrillation (OR: 2.93; 95% CI: 1.49–5.77), coronary disease (OR: 1.95; 95% CI: 0.95–4.0), cerebrovascular disease (OR: 2.70; 95% CI: 1.04–7.05), more than 2 comorbidities (OR: 1.26; 95% CI: 1.03–1.55), CCI >2 (OR: 1.49; 95% CI: 1.08–2.06), age adjusted CCI >6 (OR: 1.72; 95% CI: 1.07–2.77), and an ASA degree >2 (OR: 1.51; 95% CI: 1.07–2.11) presented a time to surgery significantly in excess of 2 days (Table 2).
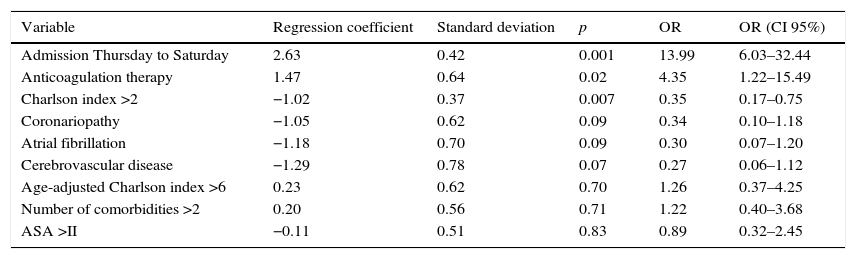
The multivariate logistic regression analysis established hospital admission on Thursdays to Saturdays, anticoagulation therapy, and a CCI >2 as predictor variables for a time to surgery in excess of 2 days (Table 3).
Multivariate analysis of variables predicting a time to surgery of more than 2 days.
| Variable | Regression coefficient | Standard deviation | p | OR | OR (CI 95%) |
|---|---|---|---|---|---|
| Admission Thursday to Saturday | 2.63 | 0.42 | 0.001 | 13.99 | 6.03–32.44 |
| Anticoagulation therapy | 1.47 | 0.64 | 0.02 | 4.35 | 1.22–15.49 |
| Charlson index >2 | −1.02 | 0.37 | 0.007 | 0.35 | 0.17–0.75 |
| Coronariopathy | −1.05 | 0.62 | 0.09 | 0.34 | 0.10–1.18 |
| Atrial fibrillation | −1.18 | 0.70 | 0.09 | 0.30 | 0.07–1.20 |
| Cerebrovascular disease | −1.29 | 0.78 | 0.07 | 0.27 | 0.06–1.12 |
| Age-adjusted Charlson index >6 | 0.23 | 0.62 | 0.70 | 1.26 | 0.37–4.25 |
| Number of comorbidities >2 | 0.20 | 0.56 | 0.71 | 1.22 | 0.40–3.68 |
| ASA >II | −0.11 | 0.51 | 0.83 | 0.89 | 0.32–2.45 |
ASA: American Society of Anaesthesiologists; CI: confidence interval; OR: odds ratio.
The most important findings of our study were: (1) in 55.6% of patients, it was not possible to operate on the hip fracture in the first 48h; (2) admission from Thursday to Saturday, the withdrawal of anticoagulant medication, and a CCI >2 were the variables associated with a time to surgery in excess of 2 days in the multivariate analysis.
The recommendation to perform surgery in the first 2 days following admission to hospital, as indicated in the clinical guidelines for handling patients with hip fracture,11–14 is not complied with in a high percentage of cases, according to the studies published in our setting. Librero et al.15 reported 25% of patients operated on in the first 48h after admission to hospital out of a cohort of 56,500 patients over 60 years of age admitted for a hip fracture to 8 public hospitals in Spain's National Health System between 2002 and 2005. Sánchez-Crespo et al.4 published 24.2% out of 634 hip fractures operated on between 2000 and 2004. Lizaur-Utilla et al.,10 28.6% out of 628 hip fractures included in a shared pre-operative acute assistance programme and operated on between 2012 and 2014. And Vidan et al.,21 35.1% in 2258 hip fractures operated on between 2003 and 2008. In our series of patients seen as part of a shared pre-operative acute assistance programme, 44.1% of patients were operated on in the first 2 days after admission. Our results confirm the hypothesis that the percentage of patients with hip fracture operated on in the first 2 days after hospital admission is low.
Some authors15,22–24 have reported a time to surgery in excess of 2 days in elderly patients, although others have not found the same association.10,21,25 With respect to gender, Vidan et al.21 and Ryan et al.23 indicate a greater time to surgery among women compared to men, whereas other studies do not publish this association.4,10,15,22,24,25 In our results, we have not any association between age or gender compared to the time to surgery.
The need to stabilize comorbidities on admission is another variable associated with time to surgery in excess of 2 days.4,10,15,21–25 The comorbidities assessed in our series include the presence of atrial fibrillation, coronary and cerebrovascular diseases, which have presented a significant association with time to surgery in excess of 2 days. Some authors relate a CCI >2 and an ASA degree >2 with a higher risk for a time to surgery in excess of 2 days.4,10,15 According to our results both variables showed statistical significance in the univariate analysis, but only CCI >2 maintained this significance in the multivariate analysis.
In clinically stable patients, the need to withdraw anticoagulant or anti-platelet medication due to the risk of intraoperative bleeding and spinal bruising constitutes grounds for a time to surgery in excess of 2 days.10,22,25,26 The clinical practice guidelines advise a careful individualized evaluation of each patient with respect to the thrombotic/haemorrhagic risk in order to determine the minimum withdrawal time prior to performing the surgical procedure.27,28 In our series, anticoagulation was a variable predicting for a time to surgery in excess of 2 days in both the univariate and multivariate analyses. Anti-platelet therapy, however, did not reach significant values in the univariate analysis, possibly due to a larger number of patients using 100mg of acetylsalicylic acid for anti-platelet purposes, as this does not require withdrawal prior to surgery.
The day for admission to hospital is a cause of a time to surgery in excess of 2 days reported in both surveys of hospitals in our country10 and also other European health systems.22–25 Lizaur-Utilla et al.10 report weekend admission as a variable associated with a time to surgery in excess of 2 days in the univariate analysis, although it did not achieve statistical significance in the multivariate analysis. Belotti et al.25 indicate that the lowest percentage of patients operated on in the first 48h by admission day corresponded to patients admitted on Thursdays or Fridays. And Ryan et al.23 show admission on Saturdays or Sundays as a variable associated with time to surgery. In our study, hospital admissions between Thursday and Saturday were a variable predicting a time to surgery in excess of 2 days in both the univariate and the multivariate analyses.
The implementation of a multidisciplinary programme for the handing of patients with hip fracture reduces the time to surgery according to recent publications.22,29–31 On admission, our patients were included in a pre- and post-operative acute assistance programme shared between orthopaedic surgeons and a specific team of specialists in internal medicine. We have not conducted any comparison with another series of patients with conventional hospital management, but our results with patients operated on in the first 2 days following admission are superior to those published by other hospital centres in our same setting, which leads us to think that this must be the correct way to act.
The kind of treatment is also reported in the literature as a variable associated with a time to surgery in excess of 2 days in patients requiring prosthetic surgery for a hip fracture,4,23,25 but this does not coincide with our results.
Our study presents limitations that must be taken into account. First of all, our series is short compared to other series published. Secondly, the time to surgery was not established for all patients by the same anaesthetist, with the consequential variability and subjectivity that this entails.
ConclusionThe results of the study confirm our hypothesis that the percentage of patients with a time to surgery of less than 2 days following admission to hospital for a hip fracture is low. Patients undergoing anticoagulant therapy, with a CCI >2, or who were admitted from Thursday to Saturday present a greater risk of not being operated on in the first 48h following hospital admission. Since these factors cannot be modified, we recommend the development of action protocols enabling the time to surgery to be shortened in this group of patients.
Level of evidenceLevel IV evidence.
Ethical responsibilitiesProtection of people and animals subjectsThe authors state that no experimentation on human beings or animals have been conducted for the purposes of this research.
Confidentiality of dataThe authors state that they have followed the protocols of their workplace regarding the publication of patient data.
Right to privacy and informed consentThe authors state that this article contains no patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sanz-Reig J, Salvador Marín J, Ferrández Martínez J, Orozco Beltrán D, Martínez López JF. Factores de riesgo para la demora quirúrgica en la fractura de cadera. Rev Esp Cir Ortop Traumatol. 2017;61:162–169.