To calculate the Scapular Balance Angle (SBA) reference values in a healthy population between 18 and 85 years old, and to define abnormality criteria for this sample.
Materials and methodsA descriptive study was conducted on a total of 300 individuals (mean age: 44.83, range: 18–83; proportion male/female: 1.59), calculating the SBA through manual measurement with a goniometer. An intraobserver Intraclass Correlation Coefficient (ICC) of 0.87 and a interobserver ICC of 0.84 was observed.
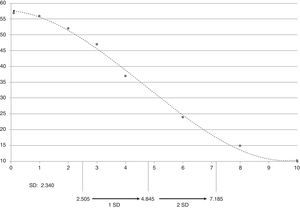
ResultsThe values for the SBA in healthy population were 2.505±2.340°. We define the abnormality criteria for this sample with an angle greater than 7.185°.
DiscussionSBA manual measurement is a simple and reproducible assessment of the position and rotation of the scapula in clinical practice. The main findings of this study are the reference values for the SBA and a statistical cut-off to define abnormality.
Calcular los valores de referencia del ángulo de balance escapular (ABE) en la población sana entre 18 y 85 años de edad, y definir los criterios muestrales de anormalidad para esta muestra.
Materiales y métodosSe realizó un estudio de tipo descriptivo-transversal en un total de 300 individuos (edad promedio: 44,83; rango: 18–83; proporción mujer/varón: 1,59), calculándose el ABE a través de la medición manual con goniómetro. Se obtuvo un valor de coeficiente de correlación intraclase (CCI) intraobservador de 0,87 y un valor de CCI interobservador de 0,84.
ResultadosLos valores para población sana del ABE fueron de 2,505±2,340°. Se define el criterio de anormalidad muestral con un ángulo mayor a 7,185°.
DiscusiónLa medición manual del ABE es una técnica sencilla y reproducible en la práctica clínica diaria para la evaluación general de la posición y la rotación de la escápula. El principal hallazgo de este estudio son los valores de referencia para el ABE y el punto de corte estadístico para definir anormalidad.
Normal scapular kinetics are a prerequisite to ensure proper shoulder function and prevent the onset of pain since they are crucial for a proper alignment of the glenohumeral and acromioclavicular joints.
Physiologically, the scapula is important for coupled and coordinated movement between the scapula and the arm (scapulohumeral rhythm), which provides an optimal spatial arrangement of the arm.2–4
From the biomechanical standpoint, the scapula provides a stable base for muscle activation and a mobile platform to maintain glenohumeral kinematics.2 In addition, it also serves as a permanent link between the core and upper limbs.2–4
Alterations in scapular movement are associated with impingement syndrome, rotator cuff tear, labral lesions, acromioclavicular joint disease and multidirectional instability.1–4
These visual alterations in the position and movement patterns of the scapula are known as scapular dyskinesia.2–4 This pathology has been described very recently and the criteria for its diagnosis are not yet clear.2–7 The word dyskinesia (dys [alteration of] kinesis [movement]) is a general term used to describe the loss of control over normal movement.2
Scapular dyskinesia is not a lesion in itself. It does not always lead to lesions and is not always directly related to a specific lesion.2 Alternatively, it may interact with other shoulder pathologies and exacerbate any associated dysfunction.2
In clinical terms, it is characterized by the prominence of the medial or inferomedial edge and scapular elevation. The most common visual findings are scapular protrusion and asymmetry.3
Clinical evaluations of scapular position based on linear differences between both scapulae have proven to be scarcely reproducible.8–10 The most widely used test is the lateral scapular slide test (LSST) designed by Ben Kibler,4 which consists in a semi-dynamic test that evaluates the distance between the inferior angle of the scapula and the spine in 3 positions.4 Some authors have described other methods with better reproducibility to conduct this assessment, but these are not cost-effective in everyday clinical practice and are mainly used for studies in elite athletes.11–13
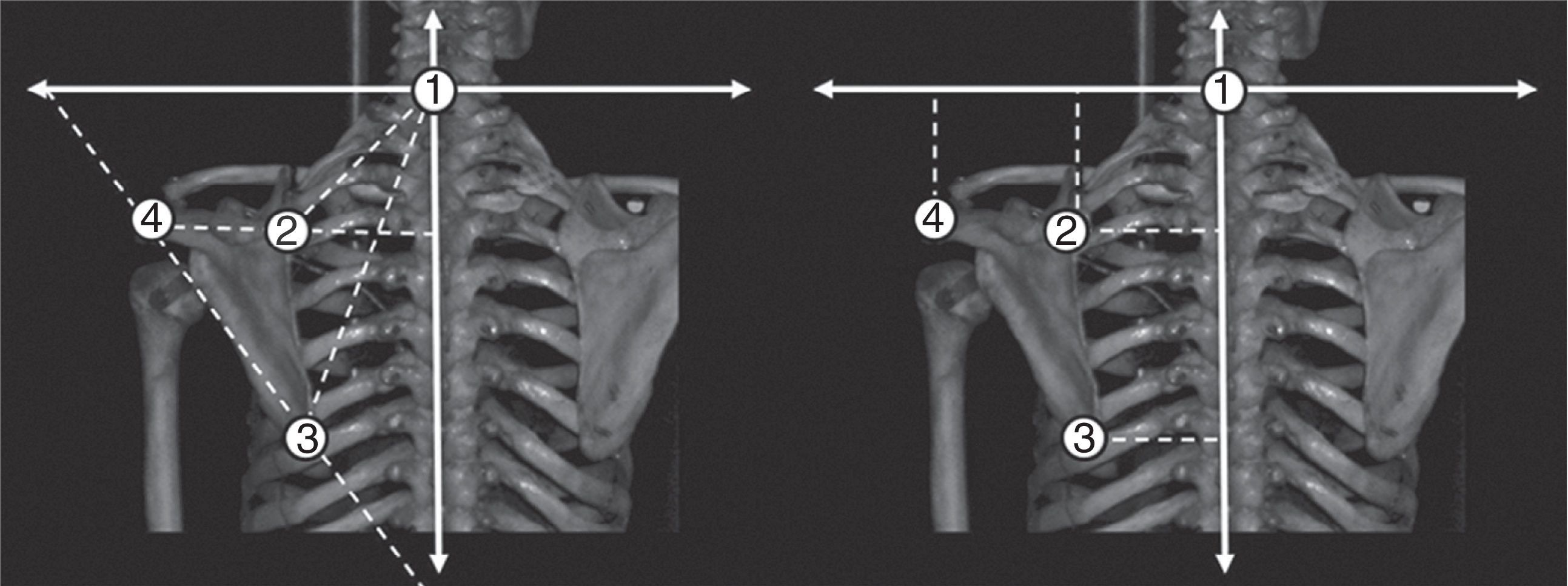
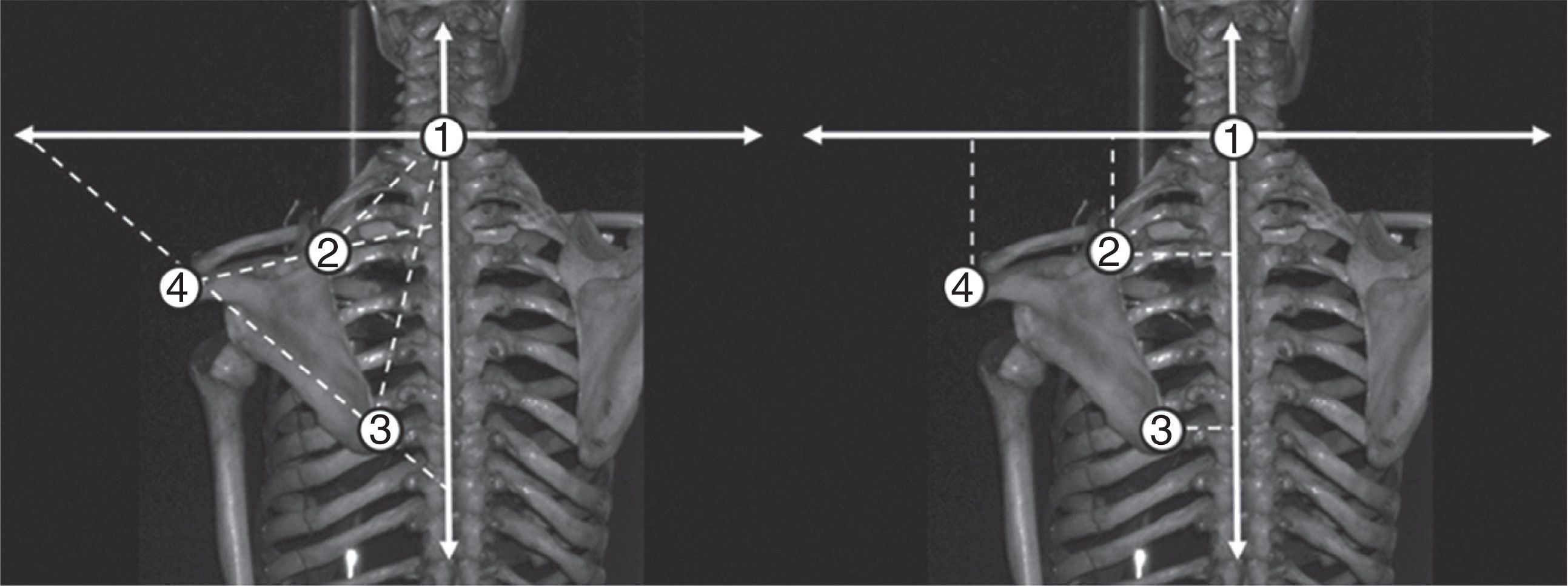
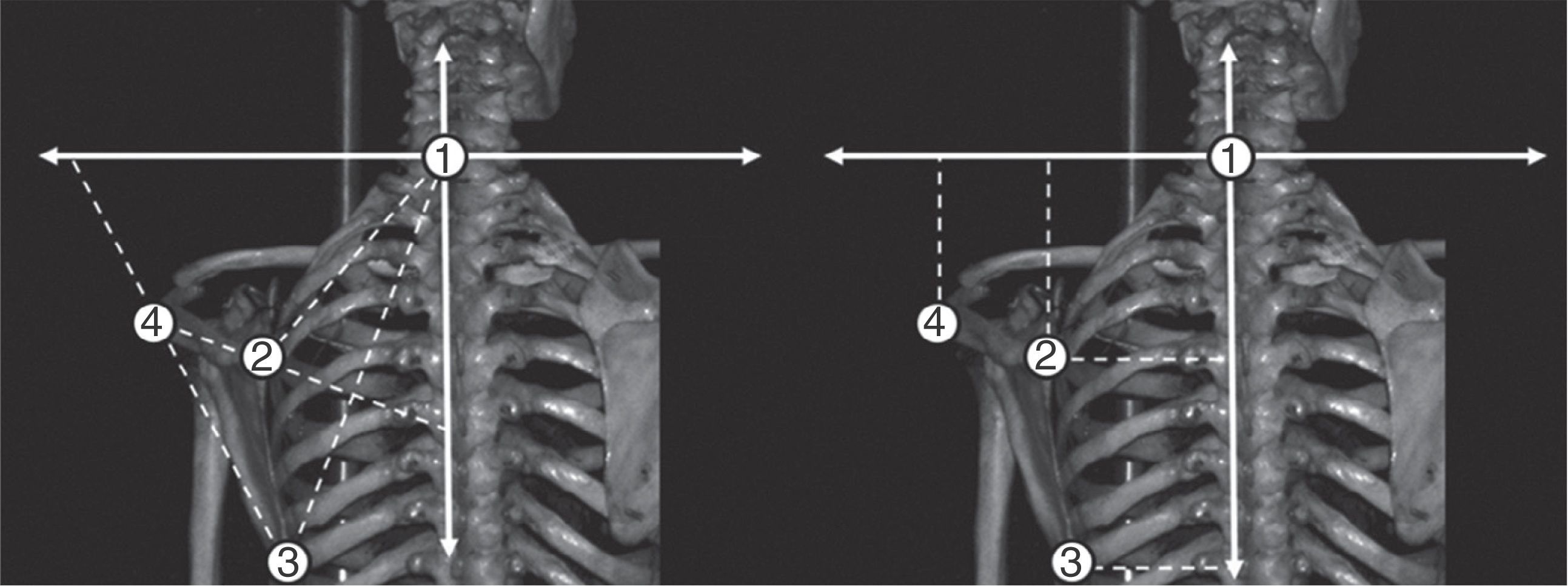
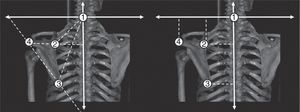
In 2010, our group developed a digital photographic test to evaluate the position and rotation of the scapula in daily clinical practice (scapular photographic analysis test [SPA]).14 The SPA test analyses 3D movements through correlated 2D photographs (Figs. 1–3).
Distances and angles in normal position. It is possible to observe the distances from reference points to the vertical and horizontal axes, along with the angles formed in a model with a normal position of the scapula. Point 1: C7 vertebra; point 2: medial edge of the scapular spine; point 3: inferior angle of the scapula, and point 4: posterior aspect of the acromion.
Distances and angles after medially rotating the inferior angle of the scapula. It is possible to observe the change in the distances and angles formed in the model, correlating with medial movement of the inferior angle of the scapula. Point 1: C7 vertebra; point 2: medial edge of the scapular spine; point 3: inferior angle of the scapula, and point 4: posterior aspect of the acromion.
Distances and angles in scapular protraction. It is possible to observe the change in the distances and angles formed in the model, correlating with the protraction movement. Point 1: C7 vertebra; point 2: medial edge of the scapular spine; point 3: inferior angle of the scapula, and point 4: posterior aspect of the acromion.
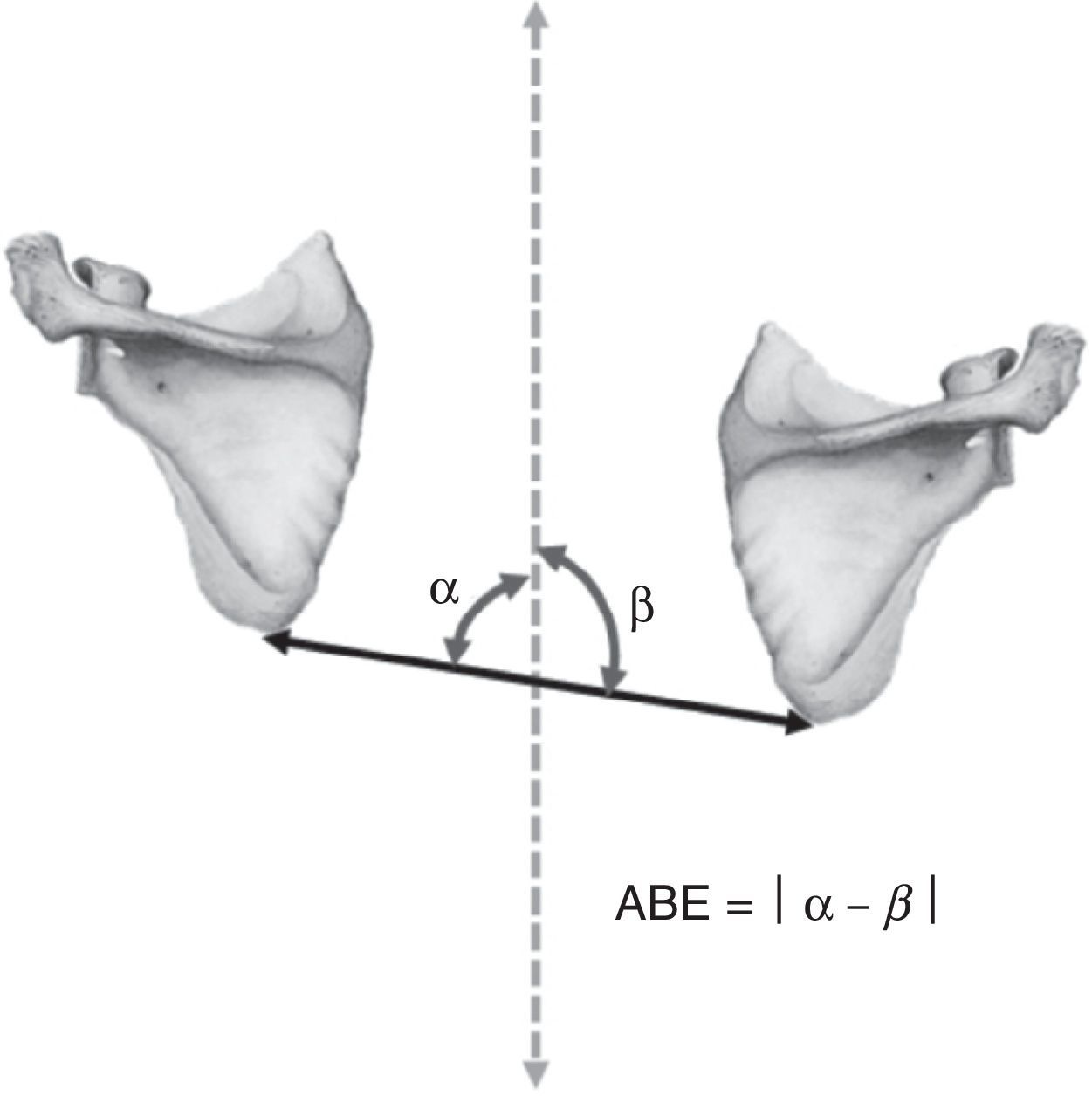
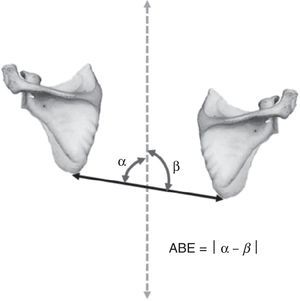
A new indicator of scapular dyskinesia called the scapular balance angle (SBA) was presented among the findings of the study. This represented the difference between the angles formed by the line joining the 2 inferior angles of the scapula with the vertical line passing through the spine.14 The usefulness of an angle in the diagnosis of scapular dyskinesia is extensive, due to its simple calculation and independence from size and weight. No angles have been previously described in the diagnosis of scapular dyskinesia, as this has mostly been based on linear measurements.
The main objective of this study is to calculate the reference values of the SBA in a healthy population aged between 18 and 85 years and to define the sampling criteria for abnormality in this sample.
Materials and methodsGeneral descriptionWe conducted a descriptive, cross-sectional study during the period between January 2011 and December 2012, in order to calculate the reference values of the SBA among a healthy population aged between 18 and 85 years, and to define the sampling criteria for abnormality in this sample. We obtained written informed consent after explaining the characteristics of the test. This study was conducted according to the principles of the Declaration of Helsinki.
SampleThe inclusion criteria defined a healthy population of both genders aged between 18 and 85 years. We excluded patients with shoulder pain (acute or chronic), acute or old fractures related to the shoulder, rotator cuff disease, adhesive capsulitis, current physical therapy treatment, morbid obesity, previous shoulder surgery (open or arthroscopic), brachial plexus injury (especially of the long thoracic nerve), neuromuscular disease, muscular dystrophies, cervical disease, scoliosis, kyphosis and prior spinal surgery.
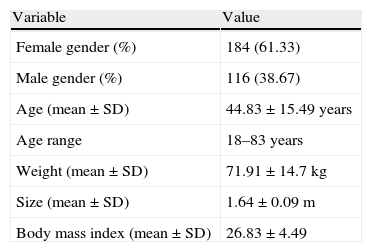
In total, we selected 300 patients by simple random sampling following the criteria presented previously (Table 1).
Summary of the characteristics of the sample selected.
| Variable | Value |
| Female gender (%) | 184 (61.33) |
| Male gender (%) | 116 (38.67) |
| Age (mean±SD) | 44.83±15.49 years |
| Age range | 18–83 years |
| Weight (mean±SD) | 71.91±14.7kg |
| Size (mean±SD) | 1.64±0.09m |
| Body mass index (mean±SD) | 26.83±4.49 |
SD=standard deviation.
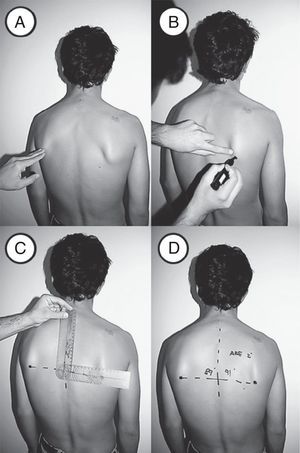
We used a booklet with photographs to standardize the measurement technique, along with 2 training sessions. A total of 7 participants were trained in the measurement of the SBA.
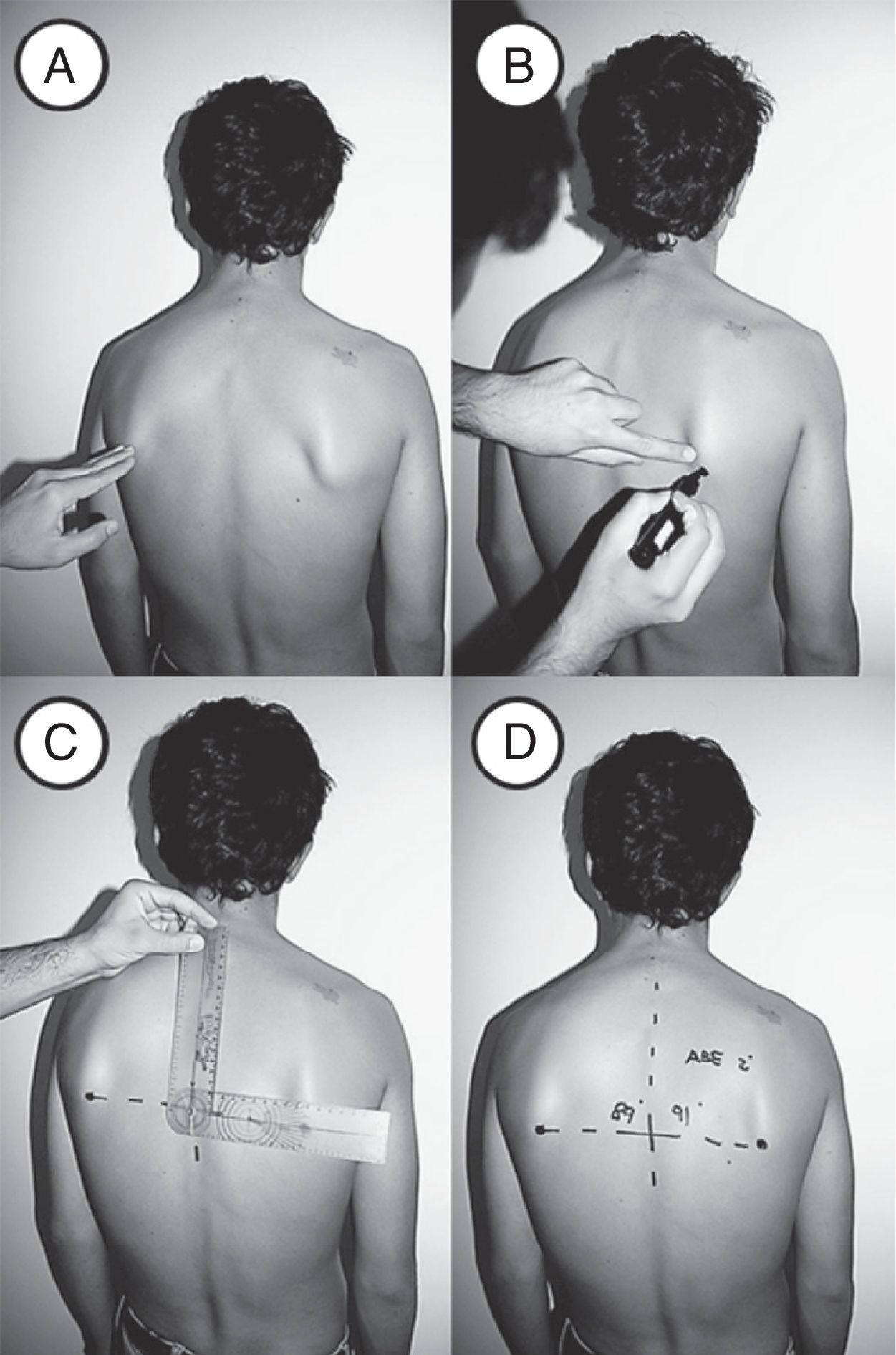
The SBA was defined as “the difference between the angles formed by the line joining the 2 inferior angles of the scapula with the vertical line passing through the spine”14 (Fig. 4).
The measurement was obtained with the patient standing on both bare feet, with arms hanging on both sides of the pelvis and heels together (Fig. 5a). Next, the inferior angle of the scapula was marked bilaterally and the line connecting these marks and another vertical line between the C7 and T9–T10 spinous processes were drawn (Fig. 5b). Lastly, the angles formed by the line joining both inferior angles of the scapula with the vertical line running through the spine (Figs. 5c and d) were measured. The absolute value of the difference between these angles corresponded to the SBA.
All the evaluators used a set of standard goniometers of the same model. The training period consisted of 2 talks explaining the theory behind SBA calculation, along with a demonstration. Next, the evaluators conducted measurement exercises among themselves, which were compared with assessments of the second session through the intraclass correlation coefficient (ICC). The ICC values obtained were 0.87 intraobserver and 0.84 interobserver.
The size measurement was performed using a 2m stadiometer with 2 levels to ensure a perpendicular measurement, and the weight was measured with a standard electronic scale.
Statistical analysisData were analyzed with the software package Stata 12 and presented as percentages and mean±standard deviation (SD). A normal distribution was found for age with the Shapiro–Wilk test, so we used the Student t test to analyze significant differences. Regarding gender, we used the χ2 test.
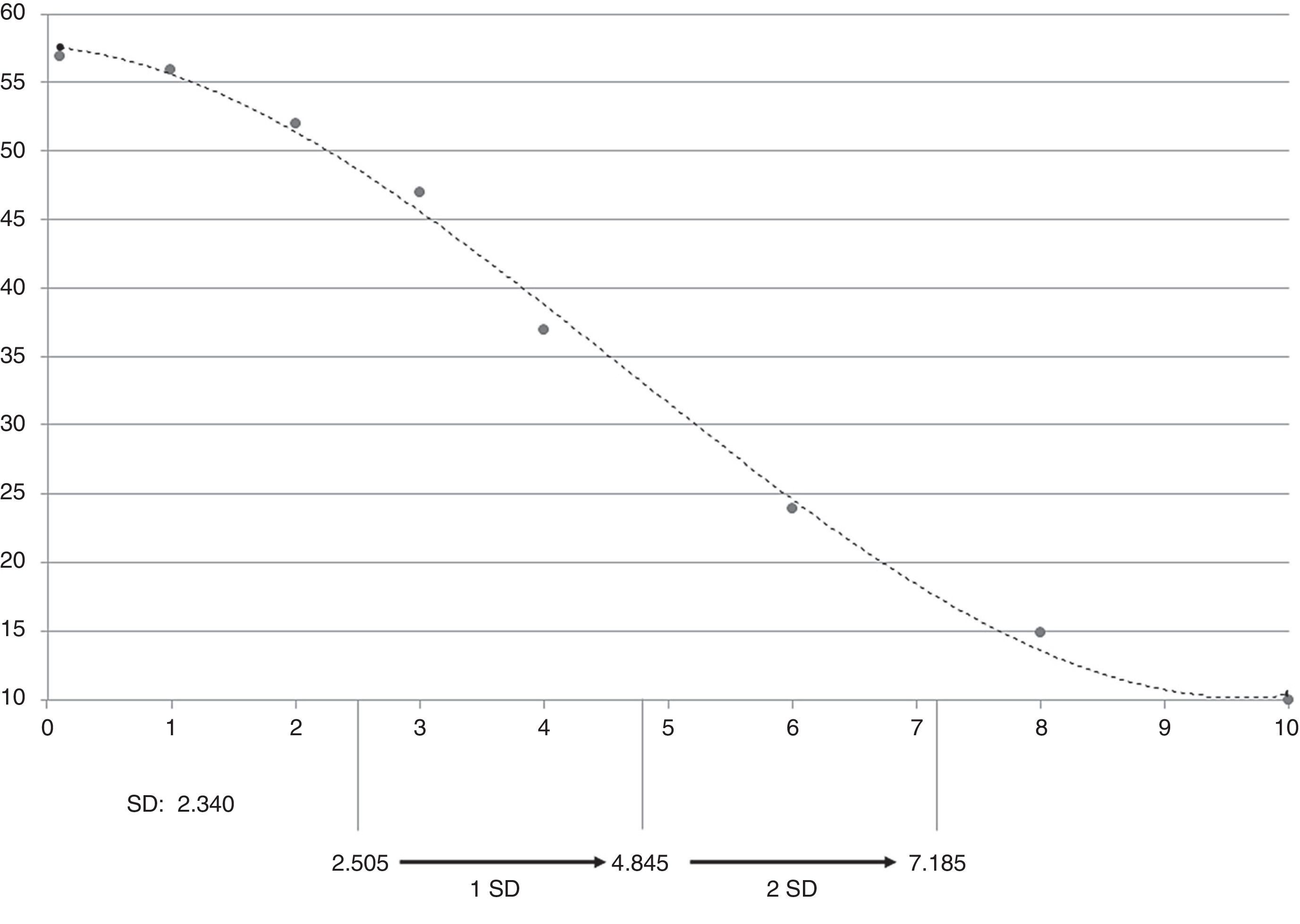
Statistical significance was set at a value of P<.05 and the sampling abnormality criterion was considered to be a mean+2 SD (95% of the sample).
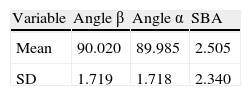
ResultsThe mean SBA of the sample was 2.505±2.340. No significant differences by age and gender (Tables 2 and 3) were found. We established a sample abnormality criterion of 7.185 (Fig. 6).
Summary of the SBA reference values of the sample selected according to age range.
| Age range (years) | Variable | Angle β | Angle α | SBA |
| 19–24 | Mean | 89.67 | 90.33 | 3.11 |
| SD | 1.88 | 1.88 | 2.08 | |
| 25–34 | Mean | 89.41 | 90.59 | 2.82 |
| SD | 1.79 | 1.79 | 2.44 | |
| 35–44 | Mean | 89.98 | 90.02 | 2.32 |
| SD | 1.67 | 1.67 | 2.36 | |
| 45–54 | Mean | 90.34 | 89.68 | 2.20 |
| SD | 1.60 | 1.59 | 2.37 | |
| 55–64 | Mean | 89.85 | 90.15 | 2.23 |
| SD | 1.59 | 1.59 | 2.25 | |
| 65–74 | Mean | 90.00 | 90.00 | 1.85 |
| SD | 1.63 | 1.63 | 2.64 | |
| 75–85 | Mean | 91.50 | 88.50 | 5.00 |
| SD | 2.38 | 2.38 | 1.15 | |
No significant differences according to age were found. SBA: scapular balance angle; SD: standard deviation.
Manual measurement of the SBA is a simple and reproducible technique in daily clinical practice enabling the overall assessment of the spatial arrangement of the scapula. The main findings of this study were the reference values for SBA and the statistical cutoff point to define abnormality.
The LSST, designed by Kibler1 to assess scapular asymmetry, recorded intraobserver ICC values between 0.52 and 0.66 and interobserver ICC between 0.45 and 0.79 for subjects with shoulder dysfunction.8 For the same test, Nijs et al.,15 in different positions, recorded ICC values ranging from 0.70 to 0.82. Methods based on an objective technique presented an ICC close to 1. Roy et al.13 reported an ICC close to 0.95 with a method for evaluating the 3D position of the scapula (Optotrak Probing System). Using a digital inclinometer adapted to rest on the scapula, Borsa et al.16 recorded an intraobserver ICC of 0.94. The disadvantage of these techniques is their high cost, taking into account that musculoskeletal disorders are among the most prevalent pathologies in everyday clinical practice.17–21 Manual measurement of the SBA is reproducible at an intraobserver (ICC: 0.87) and interobserver (ICC: 0.84) level. Being a manual technique, it is operator-dependent, but even taking this fact into consideration it presents adequate ICC values.
The anatomical landmarks determine the accuracy of this method. Working with embalmed cadavers, Lewis et al.22 showed that the skin surface can be used as a reliable and valid point of reference to determine the location of bony areas in the scapula and thoracic spine by palpation.
In 2010, our group developed a digital photographic test to evaluate the position and rotation of the scapula in everyday clinical practice.14 The SPA test requires specific bone demarcation points in order to link these coordinates to a Cartesian plane generated by the vertical and horizontal axes formed in the C7 vertebra. This enables the analysis of 3D movements by 2D photographs, since the angles and distances are modified in a correlated manner. We showed that this test is a reliable, accurate and objective method to assess the position and rotation of the scapula. Moreover, it presents diagnostic criteria with high sensitivity and specificity for the diagnosis of scapular dyskinesia.14
The SBA was presented among the findings of the study. Regarding the diagnostic capability of this angle, we observed a high sensitivity and specificity for the diagnosis of scapular dyskinesia (through ROC curve analysis, the optimal diagnosis of scapular dyskinesia was calculated with a difference greater than 5°. This criterion presented a sensitivity of 72.73%, specificity of 90.91% and odds ratio of 8). The usefulness of an angle in the diagnosis of scapular dyskinesia is significant because of its ease of calculation and independence of size and weight.
With the sampling criteria of abnormality, we established that a SBA greater than 7° would entail the diagnosis of scapular dyskinesia for this sample (from a statistical point of view). On the other hand, a SBA greater than 5° (mean+1 SD) would establish a reasonable level of suspicion for the diagnosis of scapular dyskinesia for this sample. These findings were consistent with the study conducted in the year 2010.14 However, we must take into account that this is only a statistical criterion and that no patients with scapular dyskinesia were evaluated in this study. In addition, the study conducted in 2010 employed a digital photographic method which provided accuracy, reliability and reproducibility. Despite these considerations, the values found were very similar, so they can probably be extrapolated. Nevertheless, it is necessary to conduct further studies to evaluate the diagnostic ability of the SBA in an environment employing manual measurement techniques.
The characteristics of this type of analysis are beneficial for clinical research, as they would allow the unification of criteria and generate clinical studies, making it possible to compare the results of different treatments in an objective manner. In addition, in the future, it could be used for patient assessment in daily clinical practice, in order to guide the evolution and treatment.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Contreras J, Gil D, de Dios Errázuriz J, Ruiz P, Díaz C, Águila P, et al. Valores de referencia del ángulo de balance escapular en población sana. Rev Esp Cir Ortop Traumatol. 2014;58:24–30.