To evaluate the clinical results of reinsertion of the distal biceps tendon with anterior bone anchors.
Materials and methodsA retrospective study was conducted on 79 patients who underwent reinsertion of the distal biceps tendon with anterior bone anchors. The mean age was 46 years (range: 32–64). Two anchors were used in 57% of cases, and one anchor in 43%. The same postoperative protocol was performed in all patients. Functional assessment was made using a Motor evoked potentials (MEPS) functional scale. The mean of follow-up time was 20 months (range: 12–28 months).
ResultsThe final mean of MEPS score was 95.2 points (SD: 6.8). Almost all (94%) patients had excellent and good results, and 6% a bad result. No differences were observed when comparing functional outcome among patients in whom one anchor was used (96 points) with those in whom two anchors were used (95 points), P=.5. The mean time off work was 14 weeks (range: 5–56) and 100% of patients were able to return to work. The incidence of complications was 13%. The most frequent was neuropraxia of the lateral antebrachial cutaneous nerve.
ConclusionThe anatomic re-attachment of the distal biceps tendon with bone anchors using a single anterior approach is a safe technique that offers excellent and good functional results in the medium term.
Valorar los resultados clínicos de la reinserción del tendón distal del bíceps con anclajes óseos por vía anterior.
Material y métodosEstudio retrospectivo de 79 pacientes en los que se realizó la reinserción del tendón distal del bíceps con anclajes metálicos óseos por vía anterior. El promedio de edad fue de 46 años (rango, 32-64). En el 57% de los casos se utilizaron dos anclajes y en el 43% un anclaje. Todos los pacientes realizaron el mismo protocolo postoperatorio. Se hizo una valoración funcional con la escala funcional MEPS. El promedio de tiempo de seguimiento fue de 20 meses (rango: 12-28).
ResultadosLa puntuación final media de la escala MEPS fue de 95,2 pts (DE 6,8). El 94% de los pacientes tuvieron resultado excelente y bueno y en el 6% el resultado fue aceptable y pobre. No se observaron diferencias al comparar el resultado funcional entre los pacientes en los que se utilizó un anclaje (96 puntos) con aquellos en los que se utilizaron dos anclajes (95 puntos), p=0,5. El tiempo promedio de baja laboral fue de 14 semanas (rango, 5-56) pudiendo reincorporarse a su trabajo el 100% de los pacientes. La incidencia de complicaciones fue del 13%, siendo la más frecuente la neuroapraxia del nervio cutáneo antebraquial lateral.
ConclusionesLa reinserción anatómica del tendón distal del bíceps con anclajes óseos por vía anterior única es una técnica segura que ofrece resultados funcionales excelentes y buenos a mediano plazo.
Tears of the distal tendon of the biceps are more frequent among males aged between 30 and 50 years; their incidence has been calculated as approximately 1.2 cases for every 100,000 inhabitants per year.1
The bicipital tuberosity, where the distal tendon of the biceps is inserted, is located in the proximal portion of the radius and has particular morphological characteristics. The insertion footprint has an approximate length of 22–24mm and a width between 15 and 19mm.2 It has been proven that the distal tendon of the biceps has independent insertions for each of its portions. The short head, mainly involved in elbow flexion strength, is inserted distally, while the long head, involved in forearm supination, is inserted into the proximal portion of the bicipital tuberosity. Both portions are inserted in a taper shape in the cubital edge of the tuberosity, with the tendinous fibers interlinking with the periosteal.3
Surgical treatment to repair these lesions offers better functional results than conservative treatment, achieving greater flexion and supination strength.4 Different reconstruction techniques have been described. On the one hand there are non-anatomical techniques, which entail a loss of approximately 50% supination strength,5 and on the other hand there are anatomical techniques. The latter usually achieve good or excellent results in 90% of cases, better than with non-anatomical techniques, which usually offer less than 60% of satisfactory results.6
Various methods for anatomical reinsertion have been described, with a similar rate of success: metallic bone anchoring,7,8 Endobutton9 and interferential screws.10,11
Reinsertion with bone anchors has shown good biomechanical and clinical results, with most cases using two anchors.7,10
The working hypothesis of this study was that anatomical reinsertion of the distal tendon of the biceps with bone anchors through an anterior approach offers good functional results and a low incidence of complications, with no relationship between the results obtained and the number of anchors used.
The objective of this study is to assess the clinical results of reinsertion of the distal tendon of the biceps with bone anchors through an anterior approach.
Materials and methodsWe carried out a retrospective study which included 109 patients admitted with a diagnosis of tear of the distal tendon of the biceps and who were intervened between January 2005 and November 2011. The inclusion criteria were: patients with complete tear of the distal tendon of the biceps who underwent anatomical reinsertion with one or two metallic bone anchors (Corkscrew®, Arthrex) through a single anterior approach and with less than 30 days between diagnosis and surgery. We excluded patients with partial tears or at a muscular level, patients in whom a non-anatomical reconstruction was indicated and patients with a follow-up period under 12 months.
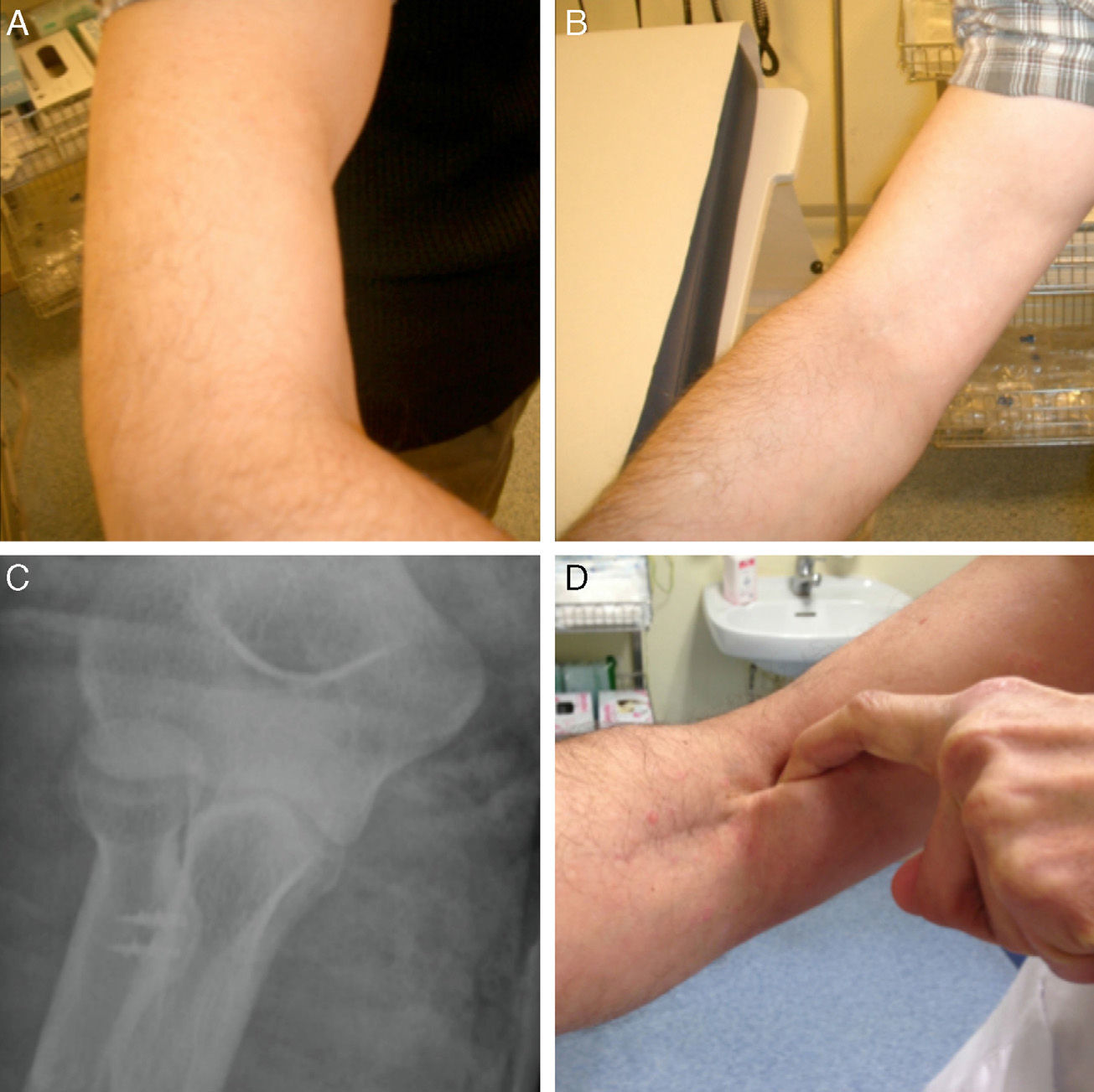
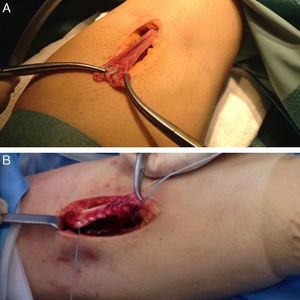
A total of 79 patients, all of them males, fulfilled the inclusion and exclusion criteria. The mean age at the time of diagnosis was 46 years (range: 32–64 years). The affected limb was the right in 52 patients and the left in 27. The dominant limb was affected in 79% of cases. In 70 patients (86.6%) the lesion was caused by a forced flexion, in 5 patients (6.3%) by a forced extension and in 4 patients (5.1%) the mechanism was uncertain. The initial diagnosis was clinical in all cases (Fig. 1). In 62 patients, the diagnosis was confirmed by ultrasound and in 13 by ultrasound and magnetic resonance imaging (MRI).
The mean time elapsed between the diagnosis and the surgical intervention was 3 days (range: 0–28 days).
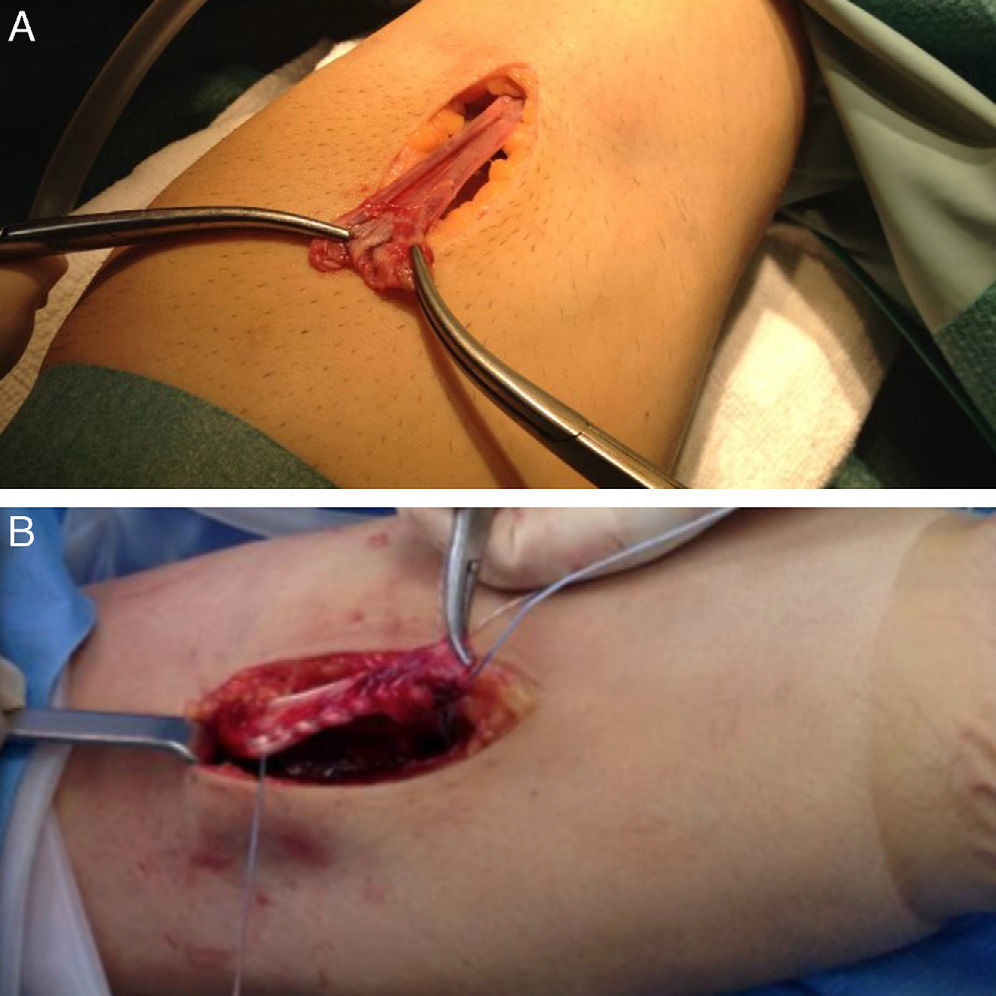
Surgical techniqueAll cases were intervened by a total of six surgeons. Patients were placed on an operating table in the supine position with the limb resting on an auxiliary table. An ischemia cuff was used at the level of the proximal third of the arm in all cases. An anterior Henry approach with an approximate length of 5cm was made, starting from the anterior flexor fold of the elbow toward the distal. When the muscle plane was reached, the lateral antebrachial cutaneous nerve was identified and retracted radially. Subsequently, the bicipital canal was identified and the proximal end of the tendon was located. Next, the dissection was continued until the bicipital tuberosity was located. The radial recurrent artery was identified and cauterized or ligated in order to prevent the formation of a postoperative hematoma. Fully visualizing the insertion footprint is vital, placing the forearm in full supination. After cleaning and curettage of the insertion footprint, the entry point for the anchor was marked with a burin. Subsequently, the bone metal anchor (Corkscrew, Arthrex) was inserted with two FiberWire® sutures or two anchors with a FiberWire® suture on each one. The decision to place one or two anchors, as well as their size, was left to the criteria of the surgeon in charge. The end of one of the sutures was passed in a caudocephalic direction by the distal third of the long portion of the tendon and then in a cephalocaudal direction with a Krakow-type suture and the end of the other in the same manner through the short portion (Fig. 1). The ends of the free sutures were used as a post, so when traction was exerted on them the tendon came closer to the insertion footprint. Lastly, both ends were tied, placing the forearm in full supination and with the elbow at 30° flexion. At the end of the intervention, a posterior plaster cast was placed, with the elbow at 90° flexion and the forearm in supination. Anteroposterior and elbow profile radiographs were obtained to confirm the correct placement of the bone anchors (Fig. 2).
Postoperative periodImmobilization with a posterior plaster cast and forearm in supination was maintained for 2 weeks. Subsequently, it was changed by a posterior plaster cast with the forearm in a neutral position until the fourth week of immobilization. After the fourth week, rehabilitation with passive assisted and progressive flexion and extension movements of the elbow and pronosupination of the forearm was started. Active mobility was started after the sixth week and progressive muscle strengthening was started after the eighth week. Strength work was left until the tenth week.
All patients attended consultation for a functional assessment. A measurement of the joint balance of the elbow (flexion and extension) was carried out, along with pronation and supination of the forearm with a conventional goniometer and using the Mayo Elbow Performance score (MEPS),12 where the score obtained is measured in a scale from 0 to 100 points, with 100 points indicating the best possible result. This scale assesses pain (45 points), mobility (20 points), stability (10 points) and the use of the elbow for activities of daily life (25 points). The result was considered excellent when it was between 90 and 100 points, good with scores between 75 and 89 points, acceptable with scores between 60 and 74 points and poor with scores below 60 points.
Simple radiographs of the elbow obtained between the third and fourth month were studied in all cases to assess the presence of heterotopic calcifications. Furthermore, the incidence of complications during follow-up was also assessed.
Data analysisThe statistical analysis was carried out using the software package SPSS version 14 for Windows (SPSS Inc., Chicago, IL, USA). The descriptive analysis included means and ranges for continuous variables and frequencies and percentages for discrete variables. The comparison of means between qualitative and quantitative variables was carried out with the Student t test for independent data if the sample fulfilled the criteria for normality and with the Wilcoxon test if it did not. We established the limit for statistical significance at a value under 0.05.
ResultsThe mean follow-up period was 20 months (range: 12–28 months).
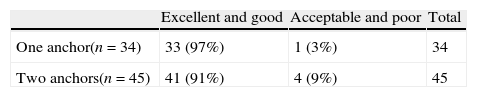
In 45 patients (57%), the anatomical insertion was carried out with two bone anchors and in 34 patients (43%) with only one anchor. The 3.5mm bone anchors were used in 62 patients (78%), whereas the 5mm anchors were used in 17 patients (22%).
The mean period of immobilization was 5 weeks (range: 3–6 weeks). The mean period until the start of rehabilitation was 5 weeks (range: 2–6 weeks). The mean duration of rehabilitation was 7.6 weeks (range: 3–29 weeks).
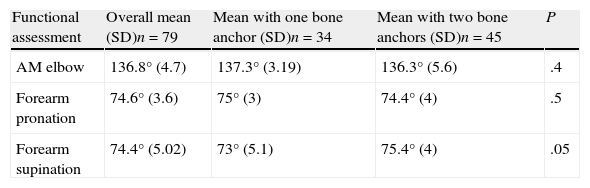
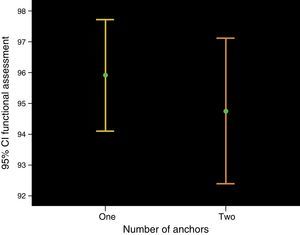
The mean arch of elbow movement was 136.8° (SD: 4.7). Mean supination was 74.4° (SD: 5.02) and mean pronation was 74.6° (SD: 3.6). The arch of movement was similar between patients in whom one anchor was used, 137.3° (SD: 3.19) and those in whom two bone anchors were used, 136.3° (SD: 5.6) (P=.4). Mean supination was 75° (SD: 3) among those in whom one anchor was used, and 74.4° (SD: 4) among patients with two bone anchors (P=.5). Patients with two bone anchors had a range of supination of 75.4° (SD: 5.1), while among those with a single anchor, the mean supination was 73° (SD: 4) (P=.05) (Table 1).
Final elbow and forearm mobility results.
| Functional assessment | Overall mean (SD)n=79 | Mean with one bone anchor (SD)n=34 | Mean with two bone anchors (SD)n=45 | P |
| AM elbow | 136.8° (4.7) | 137.3° (3.19) | 136.3° (5.6) | .4 |
| Forearm pronation | 74.6° (3.6) | 75° (3) | 74.4° (4) | .5 |
| Forearm supination | 74.4° (5.02) | 73° (5.1) | 75.4° (4) | .05 |
AM: arch of movement.
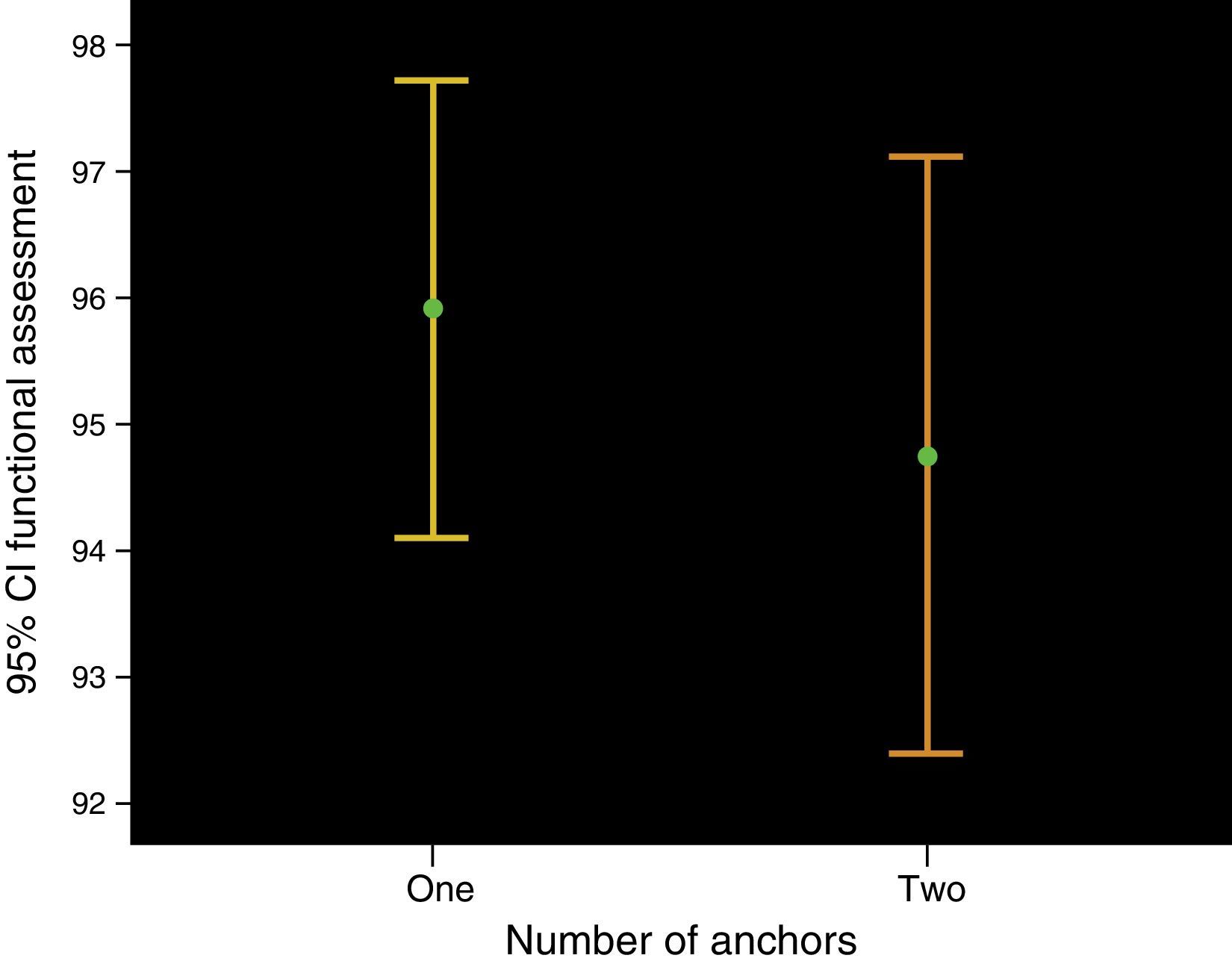
The final mean score in the MEPS scale was of 95.2 points (SD: 6.8). Among patients in whom a single bone anchor was used, the final mean score in the MEPS scale was 96 points (SD: 5.2), whereas among patients with two anchors it was 94.8 points (SD: 7.9) (P=.5) (Fig. 3).
According to the classification based on the MEPS scale, 74/79 (94%) patients had an excellent or good result, and only 5/79 (6%) had acceptable or poor results (Table 2). These five patients reported moderate pain in the anterior side of the forearm with forced pronosupination, mainly during personal hygiene and dressing.
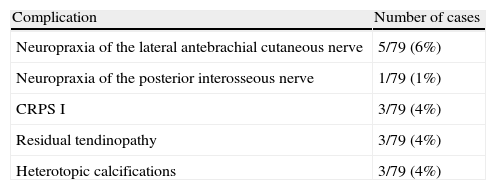
In total, 10/79 (13%) patients suffered complications. The most frequent were neurological lesions, which were observed in 6/79 patients (8%). A total of five patients suffered neuropraxia of the lateral antebrachial cutaneous nerve, while one patient suffered neuropraxia of the posterior interosseous nerve. All six cases were resolved spontaneously within a mean period of 7 weeks (range: 5–8 weeks). Three patients (4%) developed type I complex regional pain syndrome (CRPS I) which required a rehabilitation program and specific drug treatment. In three (4%) cases, persistence of pain in the anterior side of the forearm led to an indication for a control MRI scan, which revealed signs of tendinopathy but absence of signs of rerupture, whereas in three patients (4%) the control radiographs showed the presence of heterotopic ossifications, albeit without functional repercussions (Table 3).
Incidence of complications.
| Complication | Number of cases |
| Neuropraxia of the lateral antebrachial cutaneous nerve | 5/79 (6%) |
| Neuropraxia of the posterior interosseous nerve | 1/79 (1%) |
| CRPS I | 3/79 (4%) |
| Residual tendinopathy | 3/79 (4%) |
| Heterotopic calcifications | 3/79 (4%) |
CRPS I: type I complex regional pain syndrome.
Only one case required surgical reintervention due to a retraction of the cutaneous scar which caused an elbow extension deficit of 15°. This case required a Z-plasty and scar release, which achieved an extension improvement of 10°.
The mean period of absence from the workplace was 14 weeks (range: 5–56 weeks). All patients were able to return to their usual jobs.
DiscussionThis study presents the functional results of 79 patients who underwent repair of a tear in the distal tendon of the brachial biceps through a single anterior approach (Henry-type) using metal bone anchors, with which we obtained excellent and good results according to the MEPS functional assessment scale in 94% of cases.
Avulsion of the insertion of the distal biceps at the level of the insertion is a rare pathology, but accounts for 3% of all lesions in the brachial biceps. Isolated avulsion of the short head only takes place in 1% of cases, while the long head is affected in 96% of cases.13
Conservative treatment offers satisfactory results in patients with scarce functional demands.14
There are currently different surgical techniques for the repair of the distal tendon of the biceps, including anatomical reinsertion to the distal tuberosity and non-anatomical reinsertion through a tenodesis toward the brachial biceps muscle. Nevertheless, the biceps muscle strongly contributes to forearm supination and various studies have demonstrated a 40–56% reduction in supination strength with non-anatomical repairs.7
There is some controversy regarding the type of approach to use. Boyd and Anderson14 described an approach through two incisions to reduce the risk of damaging the radial nerve associated to the classical extensive anterior approach. However, the technique with two incisions has been associated to radio-cubital synostosis and heterotopic calcifications15 which could cause a limitation of elbow mobility, as well as a similar incidence of lesions of the posterior interosseous nerve.16,17
In our series, we have used a single anterior approach in all cases. Most cases did not require extending the approach beyond the fold of the elbow. Various studies have reported a low incidence of complications with the use of this approach.7,8,18–21 Out of 53 patients who underwent distal biceps reinsertion through a single anterior approach, McKee et al.20 found that 8% (4/53) presented some kind of complication related to the approach. One patient presented infection of the surgical wound, two patients presented paresthesias in the territory of the lateral antebrachial cutaneous nerve and one patient suffered neuropraxia of the posterior interosseous nerve.
In a study comparing the single anterior approach and a double approach, El-Hawary et al.22 reported 44% of complications with the single approach technique and 10% complications with the double approach, with transient paresthesias being the most common complication in both cases. Other authors, like Chavan et al.,23 carried out a systematic review to compare the results between both approaches and reported that the double approach technique presented more complications, with this difference being statistically significant. However, Grewal et al.24 recently carried out a comparative and randomized prospective study in which they assessed the results with the techniques using one and two incisions. They observed that the single incision technique was associated with a higher incidence of transient neuropraxias of the lateral antebrachial cutaneous nerve (19/47 in the single incision group versus 3/43 in the double incision group, P<.001).
In our series, the rate of complications was of 13% (10/79). As in other series, the most common complication was neuropraxia, which was observed in 6/79 patients (8%). We believe that the lesion of the lateral antebrachial cutaneous nerve is secondary to the pressure exerted by the separators at the time of exposing the bicipital tuberosity, so it is very important to pay special attention to the site where these are placed.
There are various methods of anatomical fixation for the distal biceps, like reinsertion through transosseous sutures,25,17 interferential screws,8,10,11 techniques based on Endobutton systems9,26–28 and metal bone anchors. In biomechanical studies conducted in cadavers, Endobutton systems have shown their superiority compared to the rest of techniques in terms of resistance to failure.26,27 However, no technique has been proven to offer superior clinical results to the rest.
Anatomical repair with metal bone anchors through a single anterior approach has become increasingly popular in recent years.7–9,20,21,29
Most authors recommend the use of two anchors. Soteranos et al.29 assessed the results obtained in 16 patients in whom the distal tendon of the biceps was reinserted through an anterior approach with two bone anchors. The mean age was 43 years and the mean follow-up period was 39 months. These authors found that, 6 months after the intervention, all the patients had returned to their previous work with a normal range of elbow movement in 14 patients and full pronation–supination in all cases. McKee et al.20 reported good results using two bone anchors in 53 patients with a mean follow-up period of 29 months. The final result of the DASH questionnaire was 8.2 points, final mean elbow flexion was 137°, a mean loss of extension of 2°, mean pronation of 86° and mean supination of 83°, with no significant differences found when comparing the results with the healthy side. These authors reported a complication rate of 7.5% in 4/53 patients, of which 2 were neuropraxias of the lateral antebrachial cutaneous nerve and 1 of the posterior interosseous nerve. John et al.7 reported excellent results in 46/53 patients and good in 7/53 according to the Andrews–Carson functional scale using a single transversal anterior approach and two suture anchors. In their series they found 2% of neuropraxia of the radial nerve and 4% of heterotopic calcifications.
Khan et al.8 reported the results in 17 patients using a Henry-type anterior approach and bone anchors for the reinsertion of the tendon. When comparing the range of elbow and forearm movement against the healthy side, they found a loss of extension of 5.3°, a loss of flexion of 6.2°, of pronation of 11° and of supination of 6.4°. The incidence of complications was 12%; neuropraxia of the radial nerve in 6% of cases and heterotopic calcifications in 6% of cases. The final score in the DASH questionnaire was 14.4 (range: 0–55).
These results are comparable to those obtained in our series, in which the mean final arch of elbow movement was 136.8° (SD: 4.7), with a mean final score in the MEPS functional scale of 95.2 points (SD: 6.8), with no differences between cases in which one anchor was used when compared to those with two anchors. All patients in our series returned to their normal work within a mean period of 14 weeks (range: 5–56 weeks) and there were no cases of rerupture in a mean follow-up period of 20 months (range: 12–28 months).
The limitations of this study pertain to its retrospective nature and the follow-up period, which, on average, did not exceed 24 months. Moreover, the functional results have not been compared with the contralateral limb and there was no control group.
ConclusionsAnatomical reinsertion of the distal tendon of the biceps using bone anchors through a single anterior approach entails low morbidity and rate of complications, and achieves excellent and good functional results in the medium-term.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Ramazzini-Castro R, Montiel-Gimenez A, Gallardo-Villares S, Abellán-Miralles C. Tratamiento quirúrgico de las roturas del tendón distal del bíceps con anclajes óseos por abordaje anterior único. Rev Esp Cir Ortop Traumatol. 2014;58:370–376.