Carpal tunnel syndrome is treated successfully by surgical release of the transverse carpal ligament (TCL). However, persistent weakness of grip and pain over the thenar and hypothenar ends of this ligament, and “pillar pain”, are reported to be common complications. In order to reduce these complications, different ligament reconstruction or lengthening techniques have been proposed.
ObjectiveThe purpose of this study is compare effectiveness and complications of TCL z-lengthening technique with complete TCL section.
MethodsA prospective, randomised, intervention trial was conducted on 80 patients. The patients were divided into 2 groups: (1) complete release of TCL; (2) z-lengthening of TCL according to a modified Simonetta technique.
Grip strength, pillar pain and clinical and functional assessment were carried out using the Levine et al. questionnaire.
ResultsNo significant differences were observed (P>.05) in the postoperative reviews between the two groups as regards grip strength loss and pillar pain. There were significant differences between preoperative and postoperative mean Levine scores, but there was no difference in the mean scores of the two procedures at any time.
DiscussionIn conclusion, according to the results, TCL z-lengthening is more effective than simple division, but there is no identifiable benefit in z-lengthening for avoiding complications.
La apertura completa del ligamentum carpi transversum (LCT) es el tratamiento de elección para el síndrome del túnel carpiano. Sin embargo, la pérdida de fuerza de prensión y el dolor sobre la eminencia tenar e hipotenar, denominado «pillar pain» son complicaciones comunes asociadas a dicha técnica. Se han descrito técnicas que reconstruyen dicho ligamento o lo elongan para disminuir estas complicaciones.
ObjetivoAnalizar la efectividad de la elongación en Z del LCT y la disminución de dichas complicaciones comparándolo con la apertura completa del LCT.
Material y métodoSe realiza un estudio de intervención prospectivo aleatorizado de 80 pacientes. Los pacientes fueron divididos en 2 grupos: 1) apertura completa de LCT; 2) elongación en Z según técnica modificada de Simonetta.
Se analiza la fuerza de agarre, presencia de pillar pain y valoración clínica y funcional mediante el cuestionario Levine.
ResultadosNo hay diferencias estadísticamente significativas (p>0,05) en la pérdida de fuerza de agarre y presencia de pillar pain entre ambas técnicas en las revisiones realizadas a los 15 días, un mes, 3 meses y un año posquirúrgico. Sí hay diferencias estadísticamente significativas entre los datos preoperatorios y postoperatorios sin embargo, no hay diferencias estadísticamente significativas en el cuestionario de Levine entre ambas técnicas.
DiscusiónLa elongación en Z del LCT es una técnica igual de efectiva que la apertura completa para el tratamiento del síndrome del túnel carpiano pero sin ofrecer ventajas en cuanto a la disminución de fuerza, presencia de pillar pain o mejoría de los resultados funcionales.
Complete resection of the ligamentum carpi transversum (LCT) is the treatment of choice for carpal tunnel syndrome (CTS). Nevertheless, loss of grasping strength and pain on the thenar and hypothenar known as “pillar pain” are common complications associated with this technique, and they may last from 3 months to several years.1,2
The majority of authors attribute this loss of grasping strength to the disappearance of the pulley effect of the LCT on the flexor tendons.3 The exact aetiology of this pain around the incision at the level of the eminences (“pillar pain”) is unclear. One hypothesis is that it may be secondary to an alteration in the structure of the carpal arch4 due to an oedema of the superficial tissues of the LCT, caused by injury to the cutaneous branches of the palm5 or relaxation of the thenar and hypothenar eminence muscles following the resection of the said ligament.6 This complication delays the return to everyday activities and work, and it may cause emotional anxiety, all of which lead to an increase in healthcare costs.7
Several techniques have been suggested to resolve the problem arising from the resection of an important flexor tendon pulley such as the LCT.3,8 These include its reconstruction after complete severance,9–12 as well as other techniques which simply lengthen it without completely cutting it, including the one described by Simonetta.13 Additionally, these techniques aim to prevent “pillar pain”, based on the hypothesis that this is caused by a combination of ligament disruption and exposed nerve endings together with biomechanical alteration of the carpal tunnel due to the loss of the biomechanical and neuroprotector qualities of the retinaculum flexorum.9
The aim of this work is to analyse the efficacy of Z-elongation of the TCL (reduction of pain and paresthesthia within the territory of the median nerve) and to evaluate the possible reduction in complications (loss of strength and “pillar pain”), comparing it with the complete resection of the said ligament to treat CTS.
Material and methodStudy designA randomised prospective study was performed. The study sample is composed of 80 active patients (11 men and 69 women) under the age of 65 years old. The patients were divided at random into 2 groups, each containing 40 patients (group 1 and group 2). Group 1 was treated by complete opening of the TCL, while group 2 were subjected to Z-elongation of the said ligament.
The randomisation process took place in the preoperative visit. The patients were given appointments at random for preoperative visits to the surgeons taking part in the study. Two surgeons (SPP and RHI) performed the complete resection of the TCL (group 1) while the other two (MCM and SPG) performed the Z-elongation (group 2). If patients fulfilled all of the inclusion and exclusion criteria, in this visit they were assigned to one of the two study groups (depending on which surgeon they had seen). The patient was then informed at this time about their participation in the study, and their informed consent was obtained. At no time did the patients know which technique they were to be subjected to.
The inclusion criteria were: (1) paresthesia in median nerve distribution with positive provocation manoeuvres (Phalen and/or Durkan); (2) neurophysiological confirmation of the slowing of sensory nerve conduction through the wrist (an electromyogram described by the Neurophysiology Department as showing moderate, marked or severe CTS).
The exclusion criteria were: (1) inflammatory or autoimmune disease; (2) mental or cognitive disease, and (3) rejection of the treatment.
Patient data were gathered confidentially in the preoperative visit and at 15 days, one month, 3 months and one year after surgery, to determine:
- (1)
The presence of paresthesia in median nerve territory.
The presence of Tinel's sign, the Phallen and Durkan manoeuvres and weakness and/or atrophy of the thenar musculature.
- (2)
Measurement of grasping strength using a Jamar hydraulic manual dynamometer. In all cases measurement was undertaken with the elbow flexed at 90° with the forearm in a neutral position and with 0° dorsal and palm wrist flexion. Grasping force was evaluated using a single Jamar manual calibrated dynamometer that measured kg of force per centimetre2 (kgf/cm2).
- (3)
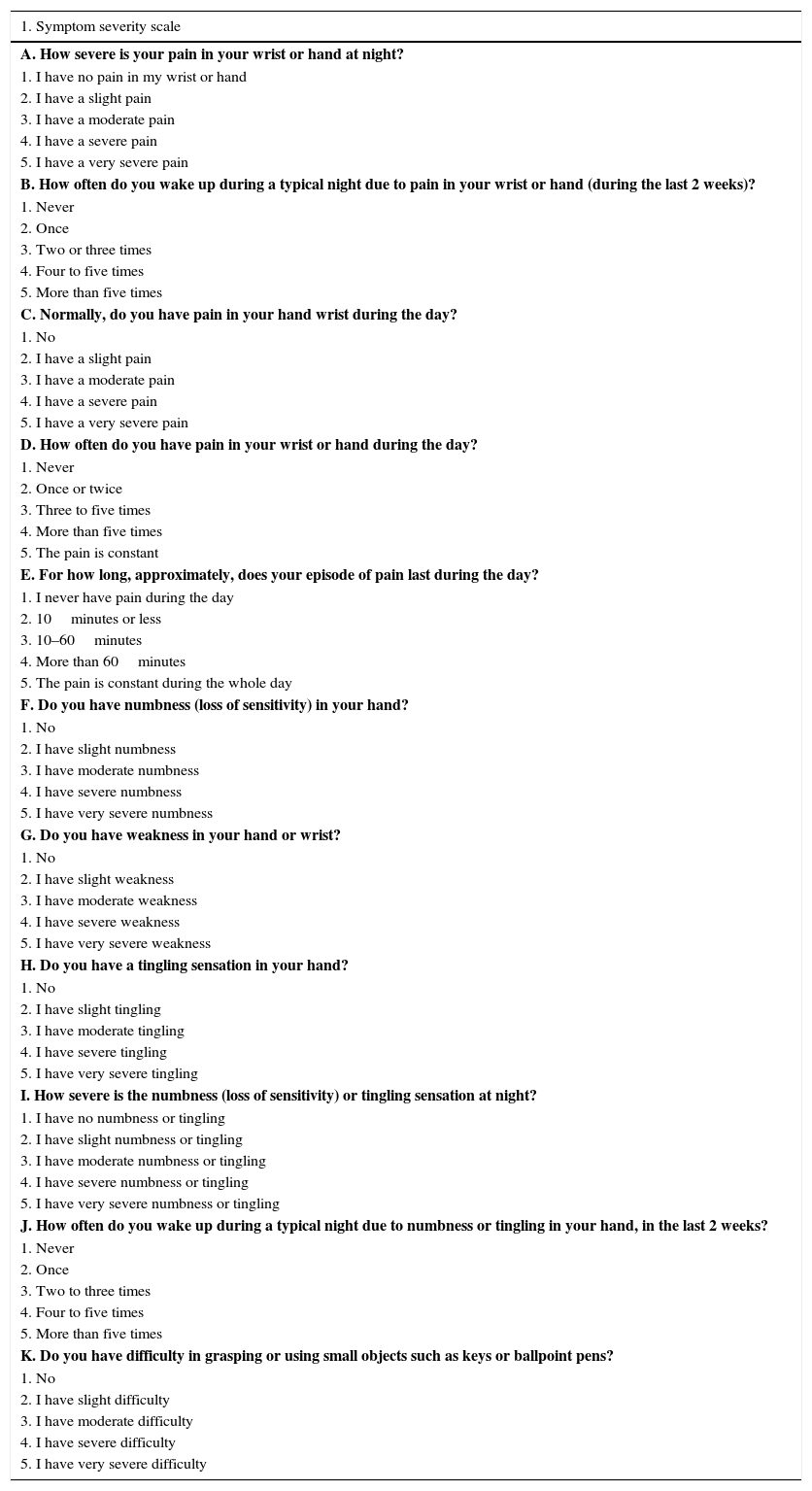
A specific questionnaire for CTS was used for clinical and functional evaluation: the Boston Carpal Tunnel Syndrome Questionnaire (BCTQ), which was first applied in 1993 by Levine et al.14 This questionnaire is composed of two parts. The first part evaluates the severity of the symptoms using 11 questions covering pain, tingling and swelling in the affected hand. Each answer gives a score of from 1 (normal) to 5 (more abnormal or more intense). The results are expressed as average scores for the questions answered. The second part consists of a functional state scale, taking eight daily activities into account. It evaluates the capacity to perform each one of these activities on a scale from 1 (normal) to 5 (more abnormal): this is also expressed as an average for the questions that are answered (Table 1).
- (4)
The presence of pain around the incision or “pillar pain” in postoperative visits. This pain was evaluated in two different ways:15 (a) by applying direct pressure on the thenar and hypothenar regions; (b) asking the patient to support his weight on a table with his elbows straight and the palms of his hands resting on the edge of the table (the “table test”).
These data were recorded by the surgeon who had performed the operation, and they were analysed by an independent observer.
Table 1.CTS clinical and functional evaluation questionnaire: Boston Carpal Tunnel Syndrome Questionnaire (BCTQ).
1. Symptom severity scale A. How severe is your pain in your wrist or hand at night? 1. I have no pain in my wrist or hand 2. I have a slight pain 3. I have a moderate pain 4. I have a severe pain 5. I have a very severe pain B. How often do you wake up during a typical night due to pain in your wrist or hand (during the last 2 weeks)? 1. Never 2. Once 3. Two or three times 4. Four to five times 5. More than five times C. Normally, do you have pain in your hand wrist during the day? 1. No 2. I have a slight pain 3. I have a moderate pain 4. I have a severe pain 5. I have a very severe pain D. How often do you have pain in your wrist or hand during the day? 1. Never 2. Once or twice 3. Three to five times 4. More than five times 5. The pain is constant E. For how long, approximately, does your episode of pain last during the day? 1. I never have pain during the day 2. 10minutes or less 3. 10–60minutes 4. More than 60minutes 5. The pain is constant during the whole day F. Do you have numbness (loss of sensitivity) in your hand? 1. No 2. I have slight numbness 3. I have moderate numbness 4. I have severe numbness 5. I have very severe numbness G. Do you have weakness in your hand or wrist? 1. No 2. I have slight weakness 3. I have moderate weakness 4. I have severe weakness 5. I have very severe weakness H. Do you have a tingling sensation in your hand? 1. No 2. I have slight tingling 3. I have moderate tingling 4. I have severe tingling 5. I have very severe tingling I. How severe is the numbness (loss of sensitivity) or tingling sensation at night? 1. I have no numbness or tingling 2. I have slight numbness or tingling 3. I have moderate numbness or tingling 4. I have severe numbness or tingling 5. I have very severe numbness or tingling J. How often do you wake up during a typical night due to numbness or tingling in your hand, in the last 2 weeks? 1. Never 2. Once 3. Two to three times 4. Four to five times 5. More than five times K. Do you have difficulty in grasping or using small objects such as keys or ballpoint pens? 1. No 2. I have slight difficulty 3. I have moderate difficulty 4. I have severe difficulty 5. I have very severe difficulty Activity No difficulty Slight difficulty Moderate difficulty Severe difficulty I cannot do anything due to the symptoms 2. Symptom severity scale A. Writing 1 2 3 4 5 B. Buttoning clothing 1 2 3 4 5 C. Holding a book while reading 1 2 3 4 5 D. Holding a telephone 1 2 3 4 5 E. Opening jars 1 2 3 4 5 F. Doing the housework 1 2 3 4 5 G. Carrying shopping bags 1 2 3 4 5 H. Bathing and dressing 1 2 3 4 5 Source: Levine et al.14
It was calculated that a sample size of 38 patients is sufficient to detect 20% of differences in grasping strength and an improvement in the score of Levine's questionnaire,14 with a precision of 50% and 95% level of confidence.
This study was approved by the Ethics Committee. The researchers undertook the study according to the principles of the Helsinki Declaration. The study was undertaken according to the protocol and fulfilled the regulations governing good clinical practice, as described in ICH norms for the same.
Surgical procedureAll of the surgical procedures were performed from November 2014 to December 2015 by the same surgical team.
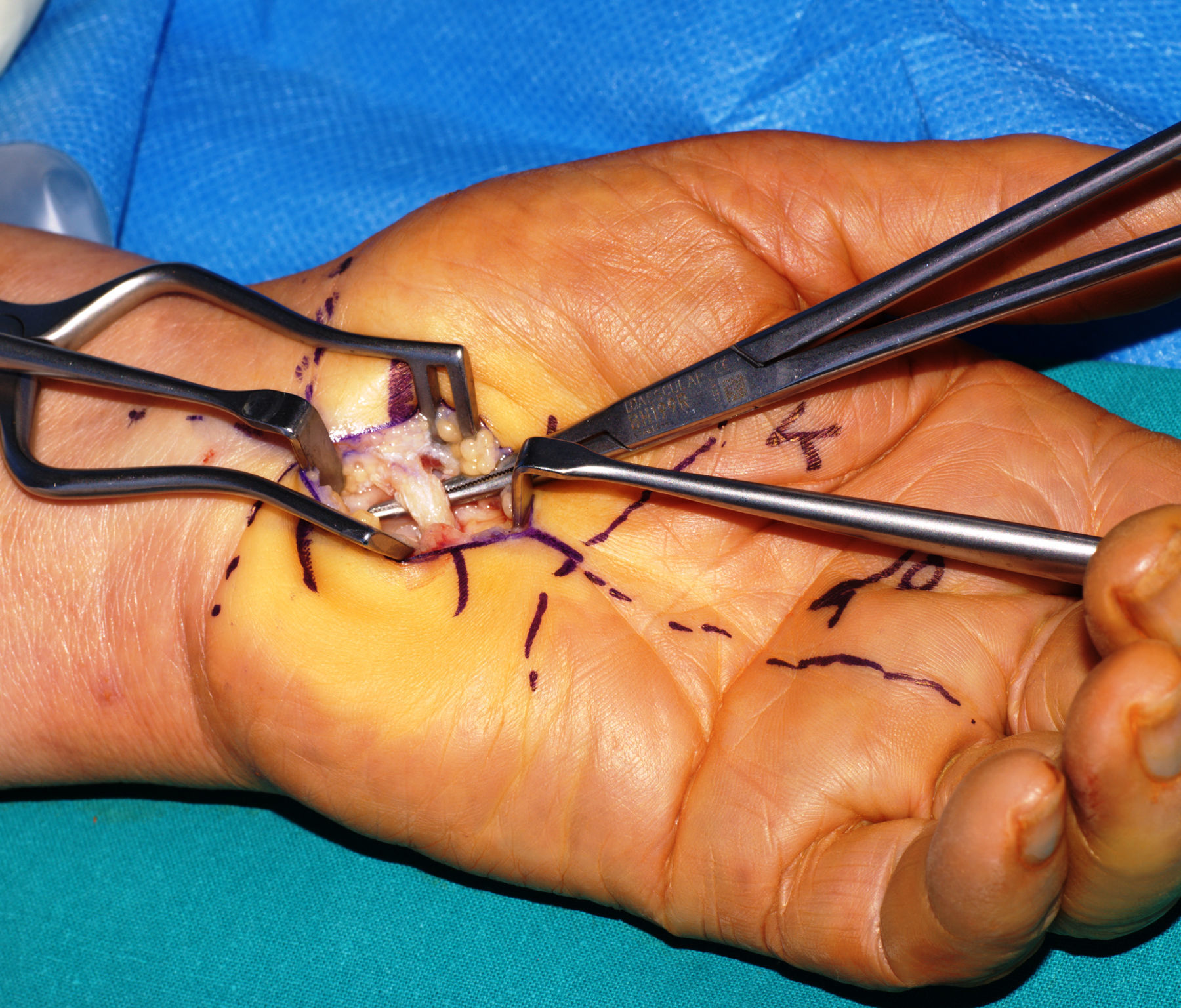
Surgical techniqueSurgery was performed under local anaesthesia, with an ischaemia cuff at 250mmHg and no antibiotic prophylaxis. A short incision was made in the palm at the level of the radial axis of the fourth finger (at a proximal level, from the distal part of the wrist fold up to Kaplan's cardinal line at a distal level). The subcutaneous tissue was separated by shallow dissection until the LCT was visible. The distal edges are identified (by identifying the distal perivascular fat which protects the superficial distal arch) as well as those proximal to the said ligament.
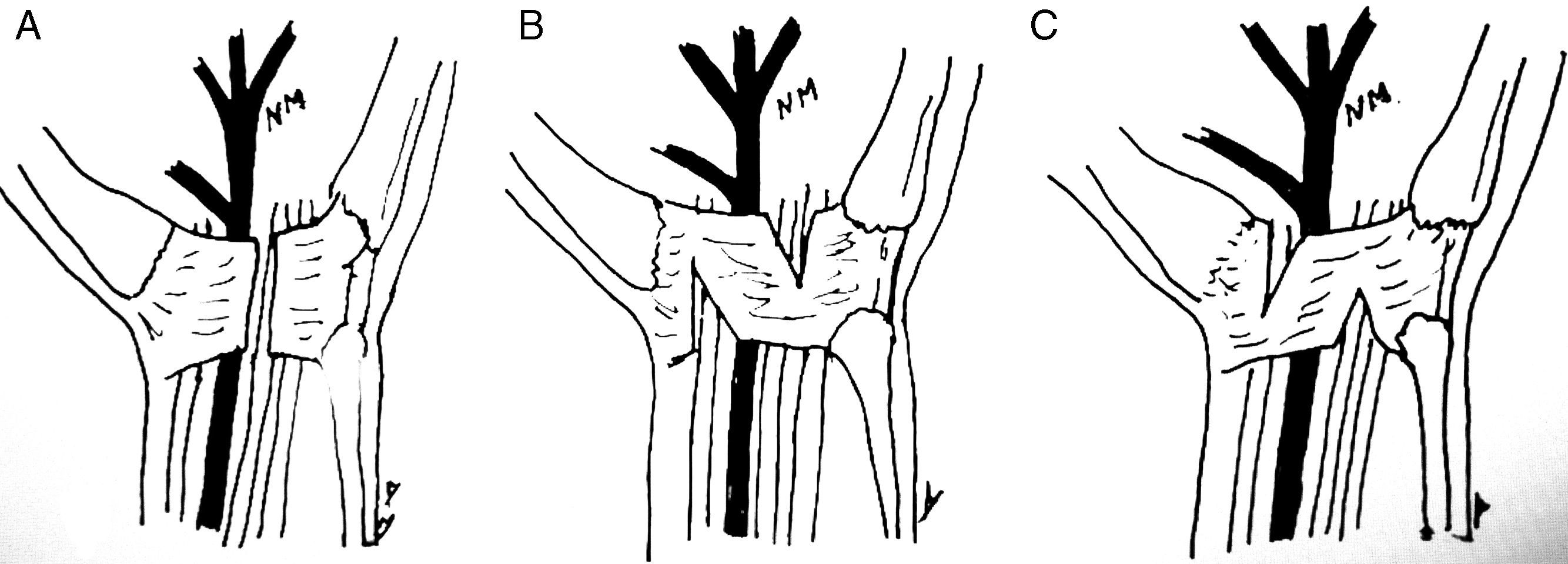
For complete resection of the LCT (group 1) a longitudinal incision was made in line with the cubital edge of the carpi radialis flexor. The median nerve and recurrent motor branch are inspected. The skin is sutured with rapid vicryl 4/0 and a compression bandage is applied before the ischaemia cuff is removed. In the Z-elongation technique (group 2), once the LCT is defined two parallel incisions are made approximately 0.5cm apart. The radial incision extends to the distal edge of the retinaculum flexorum, while the cubital incision runs to the proximal edge (contrary to the initial technique described by Simonetta) (Fig. 1). Both incisions are expanded to achieve the elongation of the ligament sufficiently to decompress the nerve (Fig. 2). Once the elongation is achieved, the median nerve as well as its motor branch are checked to ensure that they are decompressed. The wound is closed in the same way as it is for group 1.
(A) Complete resection of the LCT. (B) Elongation of the TCL according to Simonetta's technique.13 (C) Elongation according to the technique presented in this work.
Patients were instructed to actively make flexo-extension finger movements from the first moment. The first dressing change took place after 48h, and the stitches were removed from the skin after 15 days (in the first postoperative visit). Postoperative physiotherapy was not applied as a protocol in any case, and nor was the wrist immobilised with an orthosis or plaster splint.
Statistical analysisThe IBM SPSS Statistics 22 was used for the statistical analysis of our own specially designed database. Quantitative variables are described by their average and the interval of confidence stands at 95% for those considered normal; qualitative variables are shown by the percentage for each category.
The Student–Fisher t-test was used for the bivariate analysis of differences between dichotomic variable categories and another quantitative one. The Chi-squared test was used to check the association between qualitative variables, and Pearson's or Spearman's test was used for the association between quantitative variables or between a quantitative variable and a qualitative ordinal one.
The bilateral difference between groups was taken as the hypothesis for all comparisons, and the level of significance was set at 0.05.
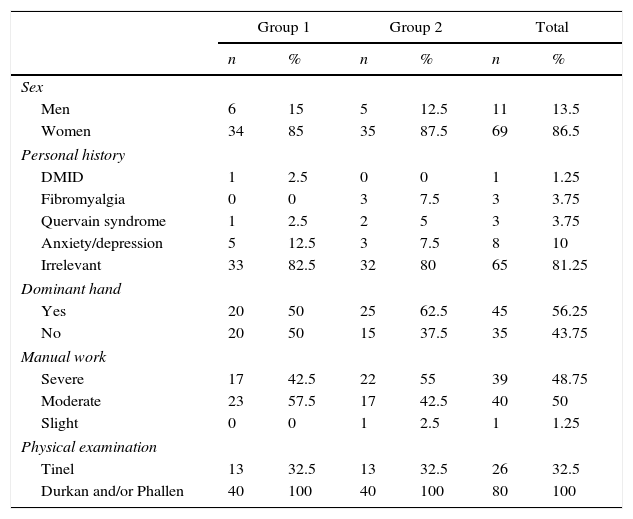
ResultsThe study sample was composed of 11 men (13.8%) and 69 women (86.3%) with an average age of 48.13 (±10.8) years old. Thirty nine of them (48.8%) performed intensive manual labour (agriculture, building work, geriatric assistant, etc.), while 40 patients (50%) performed moderate manual labour (waiters, shop assistants and housewives, etc.) and only one (1.3%) performed light manual labour (a taxi driver). Relevant personal data are that one patient was an insulin-dependent diabetic, 3 patients were diagnosed with fibromyalgia (3.8%), 8 of them (10%) were diagnosed with anxiety or depression disorder and 3 cases presented associated De Quervain syndrome (3.8%) (Table 2).
Description of the population studied.
| Group 1 | Group 2 | Total | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Sex | ||||||
| Men | 6 | 15 | 5 | 12.5 | 11 | 13.5 |
| Women | 34 | 85 | 35 | 87.5 | 69 | 86.5 |
| Personal history | ||||||
| DMID | 1 | 2.5 | 0 | 0 | 1 | 1.25 |
| Fibromyalgia | 0 | 0 | 3 | 7.5 | 3 | 3.75 |
| Quervain syndrome | 1 | 2.5 | 2 | 5 | 3 | 3.75 |
| Anxiety/depression | 5 | 12.5 | 3 | 7.5 | 8 | 10 |
| Irrelevant | 33 | 82.5 | 32 | 80 | 65 | 81.25 |
| Dominant hand | ||||||
| Yes | 20 | 50 | 25 | 62.5 | 45 | 56.25 |
| No | 20 | 50 | 15 | 37.5 | 35 | 43.75 |
| Manual work | ||||||
| Severe | 17 | 42.5 | 22 | 55 | 39 | 48.75 |
| Moderate | 23 | 57.5 | 17 | 42.5 | 40 | 50 |
| Slight | 0 | 0 | 1 | 2.5 | 1 | 1.25 |
| Physical examination | ||||||
| Tinel | 13 | 32.5 | 13 | 32.5 | 26 | 32.5 |
| Durkan and/or Phallen | 40 | 100 | 40 | 100 | 80 | 100 |
The dominant hand was operated in 45 patients (56.3%), of whom 25 were subjected to LCT Z-elongation (55.5% of the dominant hands, 31. 3% of the total sample) while 20 were subjected to a complete resection (45.5% of the dominant hands, 25% of the total).
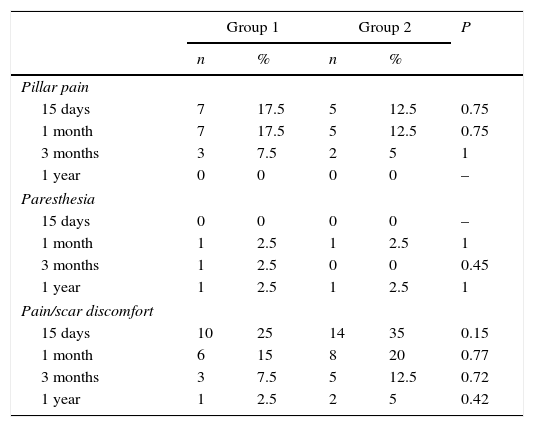
In the check-ups performed at 15 days and one month after surgery, 7 patients of group 1 (17.5%) presented symptoms of pain around the incision (“pillar pain”). This number fell to 3 patients at the check-up at 3 months (7.5%). In group 2, in the check-ups after 15 days and one month 5 patients (12.5%) presented this symptom, falling to 2 patients in the check-up at 3 months (5%). In the check-up after one year no patient in the study had the symptom of eminence pain. No statistically significant differences arose at any of the check-ups respecting this complication (P>.05) (Table 3).
CTS complications according to type of surgical technique.
| Group 1 | Group 2 | P | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Pillar pain | |||||
| 15 days | 7 | 17.5 | 5 | 12.5 | 0.75 |
| 1 month | 7 | 17.5 | 5 | 12.5 | 0.75 |
| 3 months | 3 | 7.5 | 2 | 5 | 1 |
| 1 year | 0 | 0 | 0 | 0 | – |
| Paresthesia | |||||
| 15 days | 0 | 0 | 0 | 0 | – |
| 1 month | 1 | 2.5 | 1 | 2.5 | 1 |
| 3 months | 1 | 2.5 | 0 | 0 | 0.45 |
| 1 year | 1 | 2.5 | 1 | 2.5 | 1 |
| Pain/scar discomfort | |||||
| 15 days | 10 | 25 | 14 | 35 | 0.15 |
| 1 month | 6 | 15 | 8 | 20 | 0.77 |
| 3 months | 3 | 7.5 | 5 | 12.5 | 0.72 |
| 1 year | 1 | 2.5 | 2 | 5 | 0.42 |
Respecting the presence of paresthesia, in the check-up one month after surgery one patient in group 1 (2.5%) presented paresthesia and continued to do so in the check-up at 3 months, although not in the check-up after one year. However, in the check-up after one year one patient in each group (2.5%) presented paresthesia (and in the case of group 1 this was not the same patient who had done so in the previous check-ups). Here too there were not statistically significant differences between both groups (P>.05).
One patient in group 2 had a superficial infection of the surgical wound that was resolved by oral antibiotic therapy. In the check-up after one year, 3 patients (5%), one in group 1 and two in group 2, presented pain and discomfort at the site of the scar (Table 3).
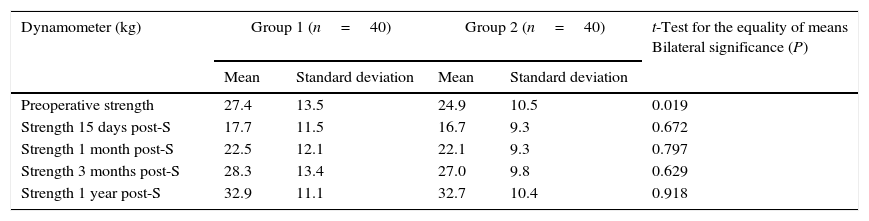
Preoperative strength in group 1 (complete resection of the LCT) stood at 28.4 (±13.5)kgf/cm2, while in group 2 (Z-elongation) it was 24.9 (±10.5)kgf/cm2. In the check-up 15 days after surgery the patients presented 60% of their strength prior to the operation. The corresponding percentage after one month was around 80% of their strength before surgery, and 3 months after surgery the patients in both groups attained similar strength to that prior to the operation (103% of their previous strength in group 1 and 108% in group 2) (Table 4). In the check-up one year after surgery the mean strength in group 1 was 32.9 (±11.1)kgf/cm2, which is 120% of the initial figure, while the mean strength in group 2 was 32.3kg (±10.4)kgf/cm2, which is 134% of the initial figure. Nevertheless, no statistically significant differences (P>.05) were detected between both groups in the difference between strength prior to the operation and strength at the postoperative check-ups (at 15 days, 1 month, 3 months and 1 year) (Table 4).
Description of grasping strength with a Jamar manual dynamometer.
| Dynamometer (kg) | Group 1 (n=40) | Group 2 (n=40) | t-Test for the equality of means Bilateral significance (P) | ||
|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | ||
| Preoperative strength | 27.4 | 13.5 | 24.9 | 10.5 | 0.019 |
| Strength 15 days post-S | 17.7 | 11.5 | 16.7 | 9.3 | 0.672 |
| Strength 1 month post-S | 22.5 | 12.1 | 22.1 | 9.3 | 0.797 |
| Strength 3 months post-S | 28.3 | 13.4 | 27.0 | 9.8 | 0.629 |
| Strength 1 year post-S | 32.9 | 11.1 | 32.7 | 10.4 | 0.918 |
| Mean reduction in strength (kg) | Mean | Standard deviation | Mean | Standard deviation | t-Test for the equality of means Bilateral significance (P) |
|---|---|---|---|---|---|
| Preoperative strength – strength at 15 days | 9.7 | 8.4 | 8.20 | 8.3 | 0.183 |
| Preoperative strength – strength at 1 month | 4.9 | 9.5 | 2.81 | 9.4 | 0.105 |
| Preoperative strength – strength at 3 months | −0.8 | 8.5 | −2.13 | 8.1 | 0.230 |
| Preoperative strength – strength at 1 year | −5.5 | 8.5 | −7.80 | 6.2 | 0.064 |
Post-S: after surgery.
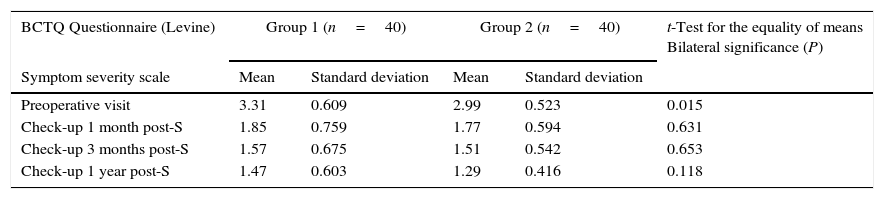
Clinical and functional evaluation: the average score for preoperative symptoms in the BCTQ questionnaire (Levine)14 in group 1 was 3.3 (±0.6), while in group 2 it was 2.9 (±0.5). The average preoperative functional score in the BCTQ questionnaire (Levine)14 in group 1 was 2.8 (±0.6), while in group 2 it was 2.5 (±0.7). There were no statistically significant differences between the two groups for the average fall in the scores of these questionnaires (the score prior to the operation and the score afterwards) at one month, three months and one year after surgery (Table 5).
Levine questionnaire data classified according to symptom severity and functional results, and a fall of ½ between preoperative and postoperative visits.
| BCTQ Questionnaire (Levine) | Group 1 (n=40) | Group 2 (n=40) | t-Test for the equality of means Bilateral significance (P) | ||
|---|---|---|---|---|---|
| Symptom severity scale | Mean | Standard deviation | Mean | Standard deviation | |
| Preoperative visit | 3.31 | 0.609 | 2.99 | 0.523 | 0.015 |
| Check-up 1 month post-S | 1.85 | 0.759 | 1.77 | 0.594 | 0.631 |
| Check-up 3 months post-S | 1.57 | 0.675 | 1.51 | 0.542 | 0.653 |
| Check-up 1 year post-S | 1.47 | 0.603 | 1.29 | 0.416 | 0.118 |
| Functional scale | Mean | Standard deviation | Mean | Standard deviation | t-Test for the equality of means Bilateral significance (P) |
|---|---|---|---|---|---|
| Preoperative visit | 2.88 | 0.668 | 2.585 | 0.705 | 0.057 |
| Check-up 1 month post-S | 2.05 | 0.729 | 1.845 | 0.690 | 0.189 |
| Check-up 3 months post-S | 1.58 | 0.690 | 1.556 | 0.575 | 0.813 |
| Check-up 1 year post-S | 1.49 | 0.641 | 1.293 | 0.449 | 0.108 |
| A fall of ½ in the severity of symptoms in pre- and post-operative check-ups | Mean | Standard deviation | Mean | Standard deviation | t-Test for the equality of means Bilateral significance (P) |
|---|---|---|---|---|---|
| Visit pre-S–1 month post-S | 1.45 | 0.925 | 1.21 | 0.688 | 0.190 |
| Visit pre-S–3 months post-S | 1.73 | 0.900 | 1.47 | 0.628 | 0.150 |
| Visit pre-S–1 year post-S | 1.83 | 0.860 | 1.70 | 0.616 | 0.434 |
| A fall of ½ in the severity of symptoms in pre- and post-operative check-ups | Mean | Standard deviation | Mean | Standard deviation | t-Test for the equality of means Bilateral significance (P) |
|---|---|---|---|---|---|
| Visit Pre-S–1 month post-S | 0.82 | 0.941 | 0.74 | 0.980 | 0.689 |
| Visit Pre-S–3 months post-S | 1.29 | 1.007 | 1.02 | 0.658 | 0.172 |
| Visit Pre-S–1 year post-S | 1.38 | 0.943 | 1.29 | 0.623 | 0.597 |
Pre-S: preoperative; post-S: postoperative.
This study analyses the results of Z-elongation of the LCT in comparison with the complete resection of the said ligament. This Z-elongation technique is a modification of the technique initially described by Simonetta,13 the efficacy of which has been studied by very few published works. In fact we only found three works on this subject in the literature.16–18 Dias et al.16 studied 52 patients over more than 25 weeks of follow-up, and they found no advantage with this technique over complete resection of the LCT in terms of neurological symptoms recovery, functional results and postoperative pain. Faour-Marti¿n et al.17 detected no differences in terms of “pillar pain” between this technique and complete resection of the LCT over the long term. Nevertheless, they did find favourable rates with this technique in comparison with complete resection at four weeks after surgery. In the study by Martin et al.18 of 130 patients there were 7 painful scars, of which 3 or 4 were suspected cases of “pillar pain”. Complete pain relief was achieved in 94.4% of these patients, although this work does not compare the technique with complete resection of the LCT.
The initial technique involves making two parallel cuts in the middle third of the LCT, running to the proximal and distal edges of the radial and cubital sides, respectively, thereby avoiding the risk of damaging the motor brand of the median nerve, which is highly variable.13 However, we made the incisions in the opposite direction so as not to cut the insertion of the hamulus in the hamate bone, thereby preventing possible pain in the hypothenar eminence (cubital pillar pain). As the incisions are made in the opposite way to that described initially by Simonetta, there is a greater risk of lesion to the recurring motor branch, although in our study this branch was not injured. It is possible to perform this technique safely if it is done carefully and with this possible complication in mind.
It must be remembered that the carpal bones form a transversal arch which together with the LCT give rise to a tunnel through which the flexor tendons and median nerve pass. The hamulus of the hamate bone and the pisiform bone on the cubital side, and the crest of the triangular bone together with the scaphoid bone on the radial side form the walls or pillars of this tunnel. The distal pillars (the triangular and hamate bones) are fixed, although the proximal bones (the scaphoid and pisiform bones) are mobile. The LCT is joined to these four bones and acts as an intrinsic carpal ligament that restricts the movement of these bones, as well as forming a pulley for the protection of the flexor tendons and median nerve.16
Studies have shown that after complete resection of the LCT intercarpal mobility increases,19 together with the projecting displacement of this ligament, the median nerve and the flexor tendons.3 According to the majority of authors, this leads to a loss of grasping strength due to the loss of the pulley effect of the LCT.20 Lluch8 reported a 16% average reduction in grasping strength with the wrist extended and 29% when it is flexed, in a study of 200 hands in which the CTS had been surgically operated, with an average follow-up of 4 years. Netscher et al.9 (23) performed a study to compare complete resection with two LCT repair techniques (reconstruction using the two flap technique described by Jakab11 vs. suture of the radial edge with the cubital edge of the LCT cut) with a follow-up of 6 and 12 weeks. Better results were obtained in terms of grasping strength in the two-flap reconstruction group11 than was the case in the other two groups. Karlson et al.12 also compared grasping strength in a group in which the LCT had been repaired vs. another one in which it had not been repaired. With the wrist extended at 45°, the patients with LCT reconstruction achieved a stronger average grasping strength, while when strength was measured with the wrist at 45° flexion, the patients with simple resection of the LCT achieved greater strength. According to Lluch3, it is probable that these paradoxical results are due to measurements being taken too early, and that exposure was greater in the reconstruction group, leading to a longer period of local inflammation. Using Simonetta's technique Faour-Marti¿n et al.17 found greater grasping strength than was the case in the group that had received complete resection of the LCT after 4 weeks of follow-up, although they found no significant differences after long-term follow-up. Seitz et al.10 carried out Z-reconstruction of the LCT and achieved similar grasping strength values to preoperative figures earlier than was the case for patients who had been subjected to complete resection, although there were no differences at 6 and 12 months of follow-up. Gellman et al.21 measured grasping strength in 24 patients following resection of the LCT. After 3 weeks these authors found 28% of preoperative strength, 73% at 6 weeks and values similar to preoperative ones at 3 months. At the check-up after 3 months in our study the patients in both groups achieved a similar level of strength to that before the operation (103% of preoperative strength in group 1 and 108% of previous strength in group 2). Although strength values were higher than preoperative ones in the check-up at 1 year (Table 4), no statistically significant differences were detected (P>.05) between the two group in any of the postoperative check-ups.
Another transitory complication which has been known to occur in CTS surgery since the end of 1930 is pain around the incision at the level of the thenar and hypothenar eminence, known as “pillar pain”.10 Incidence of this varies from 6% to 36%.22 In our study this occurred in 17.5% of group 1 patients in the first month, while the corresponding figure for group 2 was 12.5%. There were no statistically significant differences between both groups in this respect. Although the exact aetiology of this pain is unknown, four possible causes or mechanisms have been suggested in the literature. One is that this pain is due to a lesion of the ligament or muscle, where freeing the LCT allows the muscles of the thenar and hypothenar eminence which can pull on scar tissue to relax.4 Authors such as Brown et al.23 and Gartsman et al.24 believe that this pain is caused by expansion of the carpal arch and the realignment of the carpal bones. Seradge and Seradge25 described pain in the hypothenar zone after the freeing of the CTS, terming it “Piso-pyramidal pain syndrome”, attributing it to changes in carpal alignment. It has also been linked to the lesion of small cutaneous branches of the median and cubital nerves that cross the line of the incision, in a highly variable pattern.26 Wilson5 attributed this pain to the cutting of the nerve fibres in the “critical pillar rectangle”. This rectangle is delimited at a proximal level by the palm fold, at a distal level at 1cm distally from the hook of the hamate bone, at a medial level by the cubital edge of the hamate bone and at a lateral level by the scaphoid tubercle. This author hypotheses that this pain may be minimised if this “critical rectangle” is left unharmed, and he proposes making the incisions outside this area.5 Lastly, some authors believe that pillar pain is the result of a postoperative oedema which usually lasts for 12–16 weeks.10,27
Citron and Bendall28 and Wilson5 found a higher incidence of pillar pain at 4 and 6 weeks after surgery, respectively. Diet et al.16 reported an incidence of 44% of pillar pain at 2 weeks, rising to 55% at 6 weeks and improving to 39% at 12 weeks and 4% at 25 weeks. Kluge et al.29 reported 4% of cases of pillar pain after the complete resection of the TCL, with a 10 month follow-up. We found a similar maximum incidence at 2 and 4 weeks after surgery, falling in subsequent check-ups and without any case being observed in the check-up after one year (Table 4).
The possibility that the complete resection of the LCT causes a biomechanical alteration of the carpal tunnel that leads to exposed nerve endings9 has led many surgeons to reconstruct this ligament after its complete resection or simply to elongate it, as was done in this work. Nevertheless, and in agreement with the works carried out using this technique,16–18 in our study we found no statistically significant differences between both techniques respecting the presence of pillar pain in any of the check-ups (Table 3).
Respecting clinical and functional improvement (measured by Levine's questionnaire), Cagle et al.30 reported a significant functional improvement 6 weeks after surgery. These authors remark that, independently of the time difference, symptoms and functional scores improved significantly by more than 0.5 points, suggesting a significant clinical difference. Faour-Marti¿n et al.17 found a greater clinical improvement (numbness, tingling) in patients who had been subjected to complete resection of the LCT, while those patients who had received Simonetta's elongation technique attained a greater functional improvement (grasping strength and the performance of everyday activities). In our study an improvement was obtained in the clinical and functional scales (of more than 0.7 points) with both techniques. Statistically significant differences arose between the preoperative and postoperative data at check-ups after one month, 3 months and 1 year after surgery (P<.05). However, unlike findings in the previous study, better results were obtained on both of these scales (a reduction in average preoperative figures in comparison with postoperative ones) with the complete resection of the LCT, although the difference respecting the Z-elongation was not statistically significant in any of the check-ups (Table 5).
One restriction of this study is that the patients in both groups were operated by different surgeons. Although they are all members of the same surgical team and perform the standard procedure in the same way, only two surgeons (MCM and SPG) performed the LCT Z-elongation procedure, while RHI and SPP performed the complete resection. It also has to be said that the patients were included in the study by the surgeon who performed their operation, and that the results were recorded by the said surgeons even though they were analysed by an independent observer. Although the inclusion of the patients and data recording were undertaken as rigorously as possible, there may be distortion in selection and one due to the agent as these actions were not carried out by an independent observer.
To conclude, we are able to state that, in our experience, Z-elongation of the LCT is a technique that is as effective as complete resection for the treatment of CTS, although it has no advantages in terms of strength reduction, the presence of pillar pain or an improvement in clinical and/or functional results.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conform to the ethical regulations of the committee for responsible human experimentation and are according to the Helsinki Declaration and the World Medical Association.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or subjects mentioned in the paper. This document is held by the corresponding author.
FinancingThis work received no financing or specific subsidy from any financing body in the public, private or not-for-profit sector.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Castro-Menéndez M, Pagazaurtundúa-Gómez S, Pena-Paz S, Huici-Izco R, Rodríguez-Casas N, Montero-Viéites A. Elongación en Z del ligamentum carpi transversum vs. apertura completa para el tratamiento del síndrome del túnel del carpo. Rev Esp Cir Ortop Traumatol. 2016;60:355–365.