Due to the homeostatic changes that take place secondary to aging and multimorbidity, older patients are more prone to atypical disease presentation.1 Said atypical presentations are, thus, associated with worse health-outcomes (longer mean stays, comorbidity, etc.).2
Tako-tsubo Syndrome was first documented and described in Japan in 1990 as acute coronary syndrome in the absence of coronary stenosis and with a characteristic apical ballooning image in the context of an emotionally o physically stressful event. It is an infrequent entity which constitutes no more than 1% of all acute coronary syndrome presentations. It generally affects postmenopausal women with few cardiovascular risk factors.3,4 Incidence of heart failure secondary to this entity seems to be higher in older patients and it seems to cause this demographic a higher prevalence of recurrence and in-hospital adverse events.5
We present an 89-year-old woman with an excellent functional state prior to admission (Barthel Index 85/100, Lawton & Brody Index 6/8) and without cognitive impairment signs. She had a history of mitroaortic sclerosis, and a complete atrioventricular block (a pacemaker was implanted). She was admitted to the Geriatric Ward due to dyspnea that progressed for 7 days until it affected her even at rest and orthopnea. While obtaining a history, the patient mentioned the next day would be the anniversary of the death of a child she had had that had died at age 3. Jugular engorgement ++/++++, lower limb swelling, bibasilar rales and aortic and mitral systolic murmurs were observed on examination. Leukocytosis with neutrophilia, slight anemia, a low platelet count (in relation to already diagnosed thalassemia minor and autoimmune trombopenia), a C-reactive protein value of 111.5mg/L, a natriuretic B-peptide of 650pg/mL and a troponin I of 72.4pg/mL were determined in the bloodwork on admission. On the chest X-ray, we observed a right basilar condensation, signs of a cephalization of vessels and pleural effusion. The EKG showed a pacemaker rhythm (Fig. 1). She was diagnosed with heart failure in the context of right basilar pneumonia and was started on endovenous diuretics and antibiotic treatment. Progressively, enalapril and bisoprolol were added.
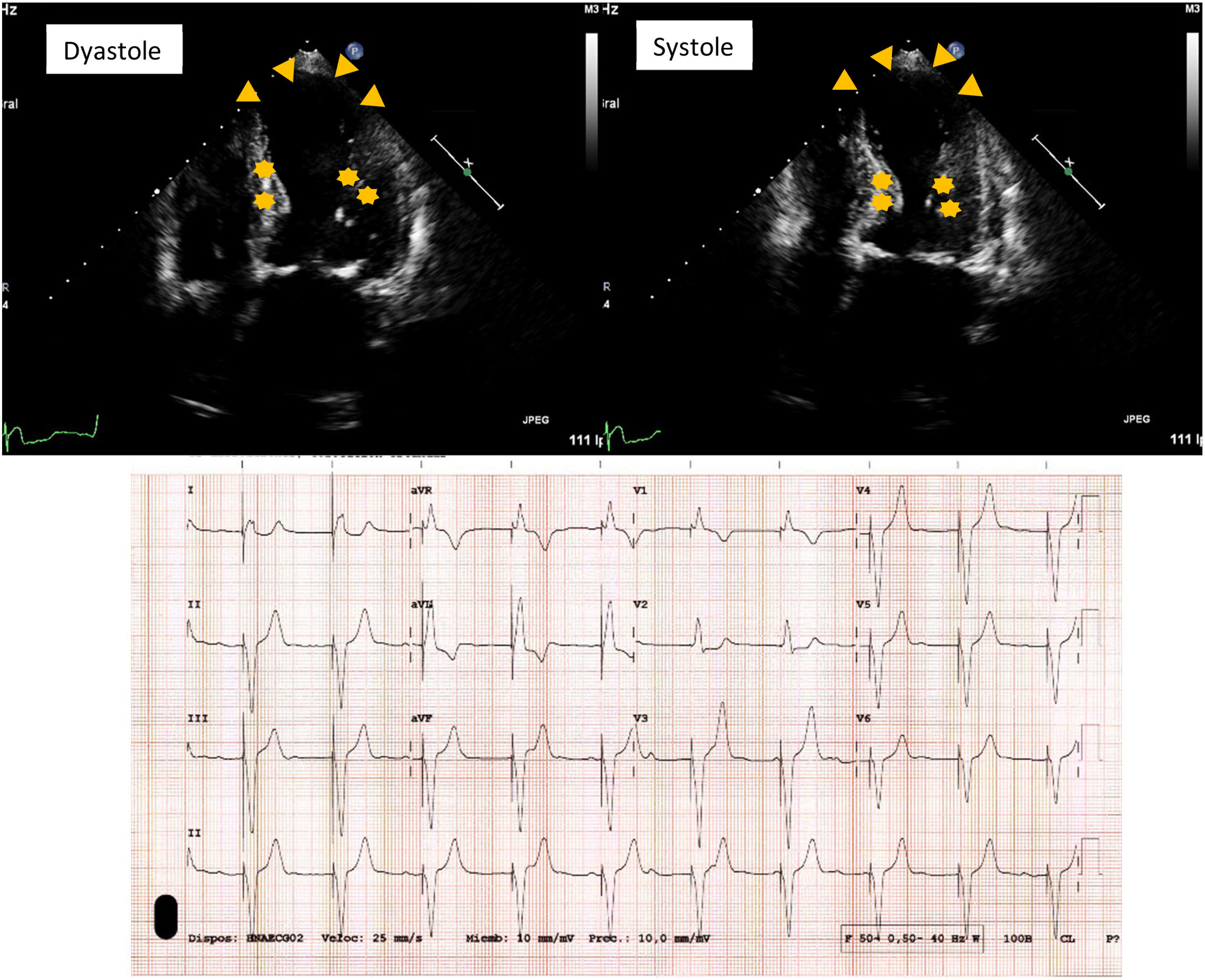
In the echocardiogram, triangles show apical akinesia a ballooning and stars show hypercontractility in bases. The EKG shows a sinus rhythm with complete AV block and a ventricular pacemaker stimulation that causes a broad QRS and leftward QRS axis, with a concordant repolarization image in D-I.
In spite of having optimized pharmacologic treatment and an initial improvement, after the first 24h, the patient's dyspnea got worse and she spiked a fever, so treatment was intensified and antibiotics were switched. She presented no chest pain. On the third day, an echocardiogram (Fig. 1) was performed, where asynchrony and akinesia of the apex, as well as hypercontractility of the bases and a low left systolic output (45–50%) were described, all of which would be compatible with an already resolving Tako-tsubo syndrome. We drew more blood and found an elevation in troponin I, the peak reaching 1550pg/mL. After joint evaluation with Cardiology, treatment was again optimized by emphasizing beta-blockers and a new echocardiogram was performed 7 days after that, where the motility abnormalities in the apex were almost completely solved, there was no intraventricular gradient and systolic output was normal. The patient did not receive anticoagulant therapy due to the preexisting trombopenia and anemia.
The patient showed a progressively good clinical evolution and was discharged 14 days after admission.
DiscussionWe consider this case to be important and illustrative due to the fact that acute coronary syndrome is the typical form of presentation of stress myocardiopathy (Tako-tsubo) and our patient denied having presented any form of chest pain throughout her hospital stay. Some cases where this entity has presented without chest pain have been described in literature,6 but they are few and far between and cases in older patients with atypical presentation are mostly absent.
There is also a hypothesis about the pathophysiology of this syndrome that suggests that a sympathetic hyperstimulation in the context of an excess of catecholamine activation in relation to stress may be the main cause.7 In this context, this case report leads us to conclude there may be a chronological relationship between the death of her daughter and the Tako-tsubo syndrome. Moreover, cases related to stressful events, albeit with typical symptoms, have been described in older adults.8,9
Normally, an evaluation of the permeability of the coronary arteries is essential in order to diagnose Tako-Tsubo Syndrome. This did not take place in our case because the patient was hemodynamically unstable at the time and the Cardiologists that evaluated the echocardiogram found the image to be highly suggestive of the definite diagnosis.
Furthermore, this case is relevant because it describes a very elderly patient with an atypical presentation and, taking into account that the population is progressively aging, this type of presentation of coronary syndromes might become increasingly more common. Furthermore, atypical or lesser-symptom presentations are well known by geriatricians, but it is important to highlight this type of case so that all the specialties that treat older adults consider them. Thus, this patient is an example of how important inter-specialty collaboration is.
Funding/SupportNM-V received funding from “la Caixa” Foundation (ID 100010434), under agreement LCF/PR/PR15/51100006.
Conflict of interestNone reported.