Death certification requires the same effort and dedication as all reports by doctors during their patients’ lifetimes. The physician must follow the basic instructions to complete a death certificate correctly, taking special care to fill in the sequence of causes of death. In the case of a pandemic, completion of the death certificate falls to the primary care physician and therefore the official bodies must publish instructions based on international recommendations. It should be established as soon as possible whether it is possible to report deaths telematically. While this is not possible, in a pandemic procedures should be put in place to enable the immediate reporting of deaths to the health authorities.
La certificación de la defunción es un acto médico en el que el profesional debe poner el mismo esfuerzo y dedicación que en el resto de los informes elaborados en vida del paciente. Para su correcta cumplimentación el facultativo debe seguir las instrucciones básicas, poniendo especial cuidado en rellenar adecuadamente la secuencia de causas de muerte. En casos de pandemia, la cumplimentación del certificado de defunción corresponde a la medicina asistencial y para poder hacerlo, los organismos oficiales deben publicar instrucciones basadas en recomendaciones internacionales. Debe establecerse, cuanto antes, la posibilidad de comunicación telemática de las defunciones. Mientras eso no sea posible tienen que establecerse procedimientos que permitan en situación de pandemia, comunicar de forma inmediata la mortalidad a las autoridades sanitarias.
Documented knowledge of a culture’s own social history and that of the individuals within it is a characteristic of developed societies. One of the factors that influence this social knowledge is the existence of records. Birth and death registries are useful means for learning our social history. In Spain we find documents of records of this type dating from the 16th century, kept in parish churches together with baptism certificates. After some time inscription also took place outside churches. The first place to keep registries of death in the courts of justice was the state of Massachusetts (1639).1
The medical certification of death first appeared in the last third of the 19th century and occurred due to several reasons. On the one hand, the increased closeness of doctors attending to the dying in cities was a factor, together with the scientific basis public hygiene, which was largely based on the development of medical statistics and public preventive measures. This also gave rise to new laws and civil codes, and it was the origin of civil registries. Moreover, the inclusion of medical statistics led to the internationalisation of disease prevention. At the end of the 19th century, almost all European countries had centralised death registration systems.
In 1871, after several attempts, the Registry Office (RO) commenced work in Spain.2 This advance had been preceded by a transition period during which a partial provincial registry office started work for large and medium-sized towns in 1841. The Law made it necessary for all municipalities to create a RO, in which data on the civil status of all Spanish citizens had to be recorded (births, marriages and deaths, etc.) independently of their beliefs. A century later, in 1957, the need to update and renovate the law currently in force was detected, adapting it to the needs of the time. This led to the Law of 8 June 1957, on RO.3 Finally, in 2011 a new RO Law was passed,4 to make it suitable “for the values enshrined in the 1978 constitution as well as the current reality of Spanish society”. Although it had been planned to come into force on 30 June 2020, judicial and organisational measures against COVID-19 have delayed its coming into force once again, this time until 30 April 2021.5
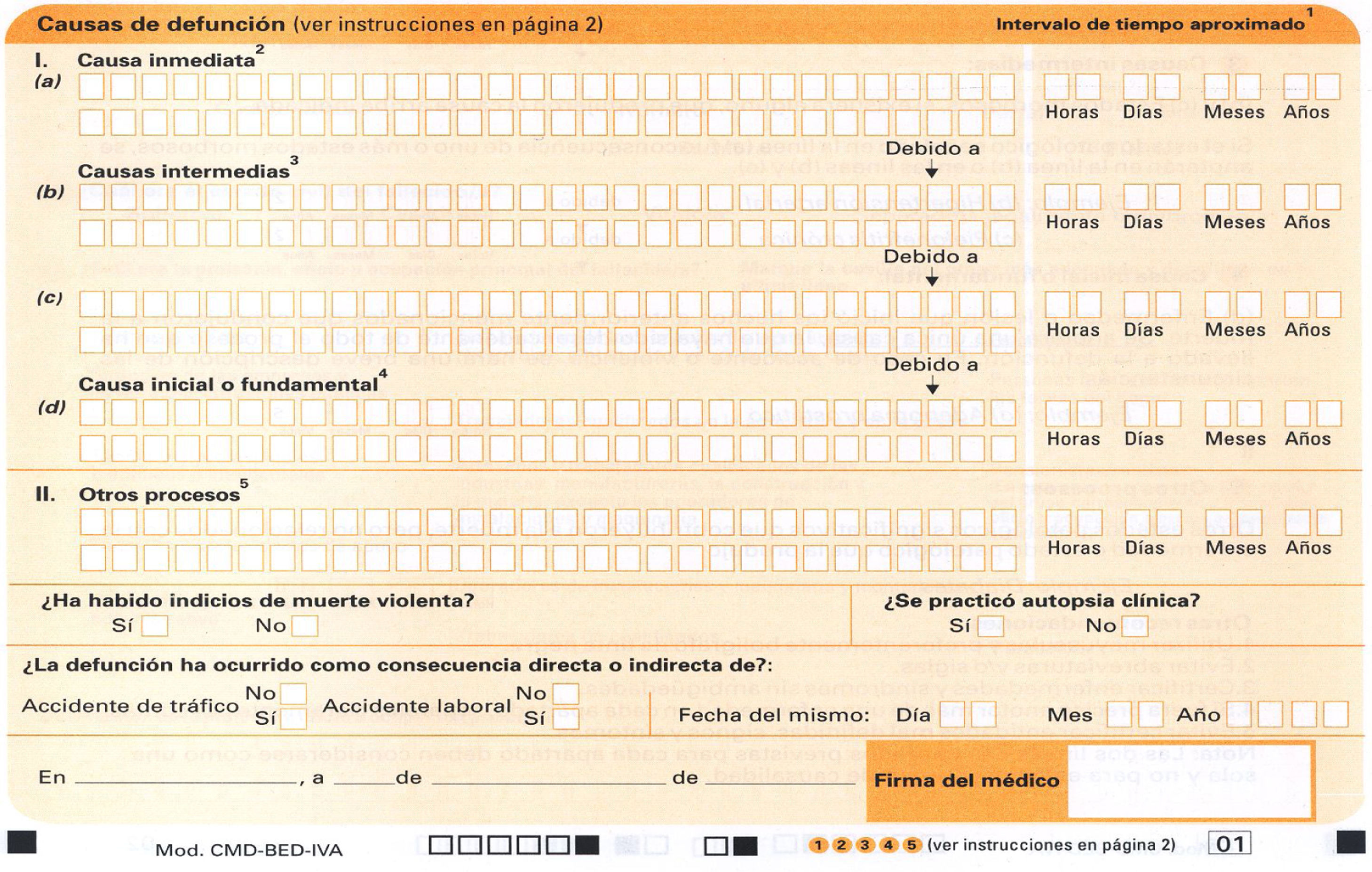
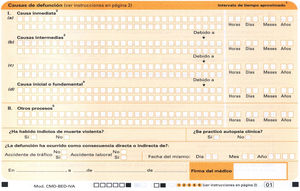
Parallel to the RO, the medical death certificate (MDC) has also evolved. Currently in Spain the model published in January 2009 is in force. This was prepared by the General Board of Official Doctors’ Associations (CGCOM) and the National Institute of Statistics (INE). The change involved the inclusion in a single document of the MDC and the statistical data of the State Deaths Bulletin (Statistical Mortality Bulletin) (BED). The MDC-BED is a document composed of a printed A3 sheet folded in half. As Arimany Manso et al. explain,6 if we consider this document to be composed of 2 sheets, the first corresponds to the Organisation of Associated Doctors (Organización Médica Colegial) (OMC) and it shows the medical data supplied by the certifying doctor who has to fill it out. The second sheet is usually filled in by the undertakers with the data supplied by family members of the patient who died, and these data consist of the civil aspects of the subject. It is available in paper format from the provincial Official Doctors’ Associations (Colegios Oficiales de Médicos) (COM). The current MDC-BED has a more medical approach, to comply with the norms of the World Health Organisation (WHO).6
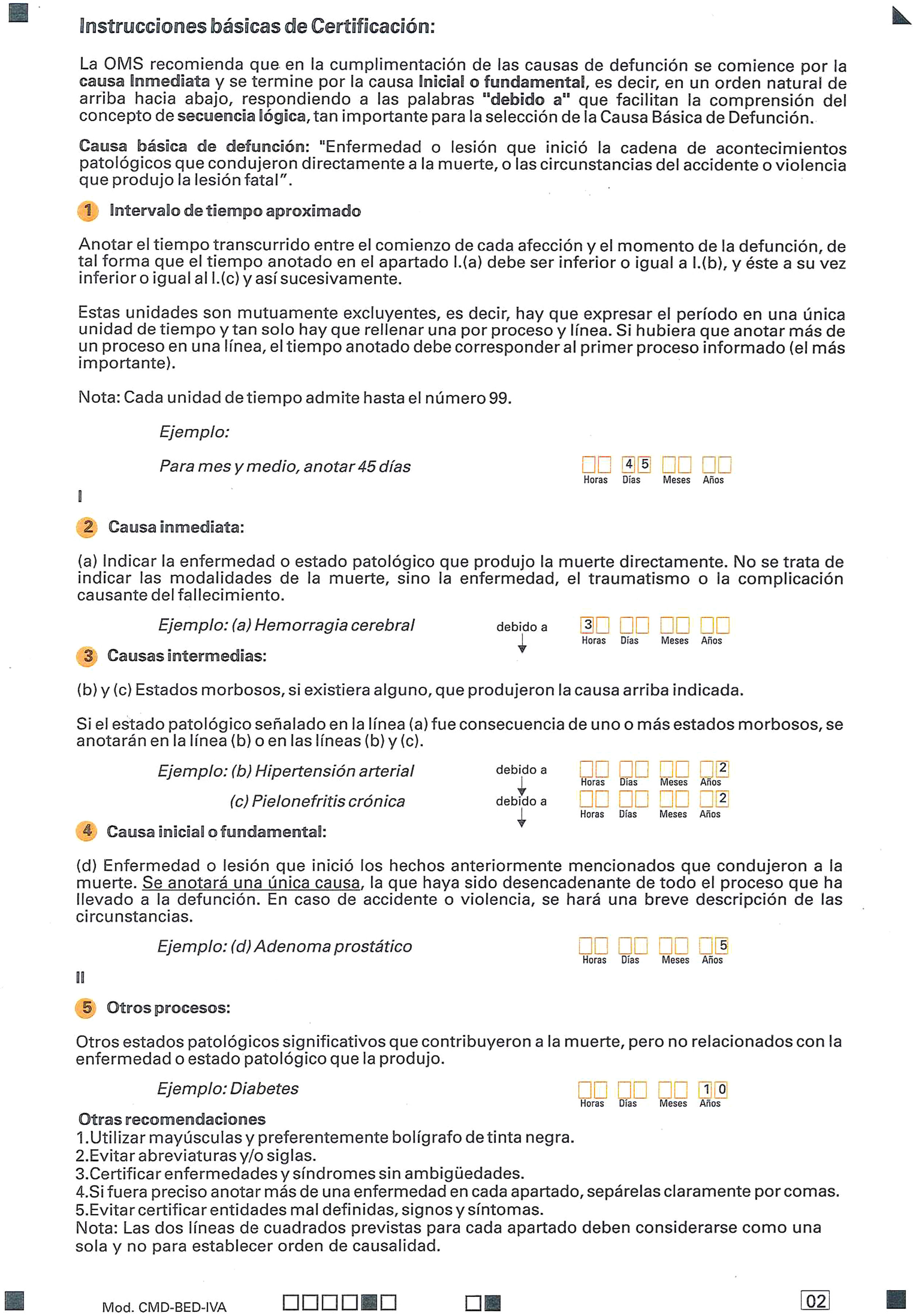
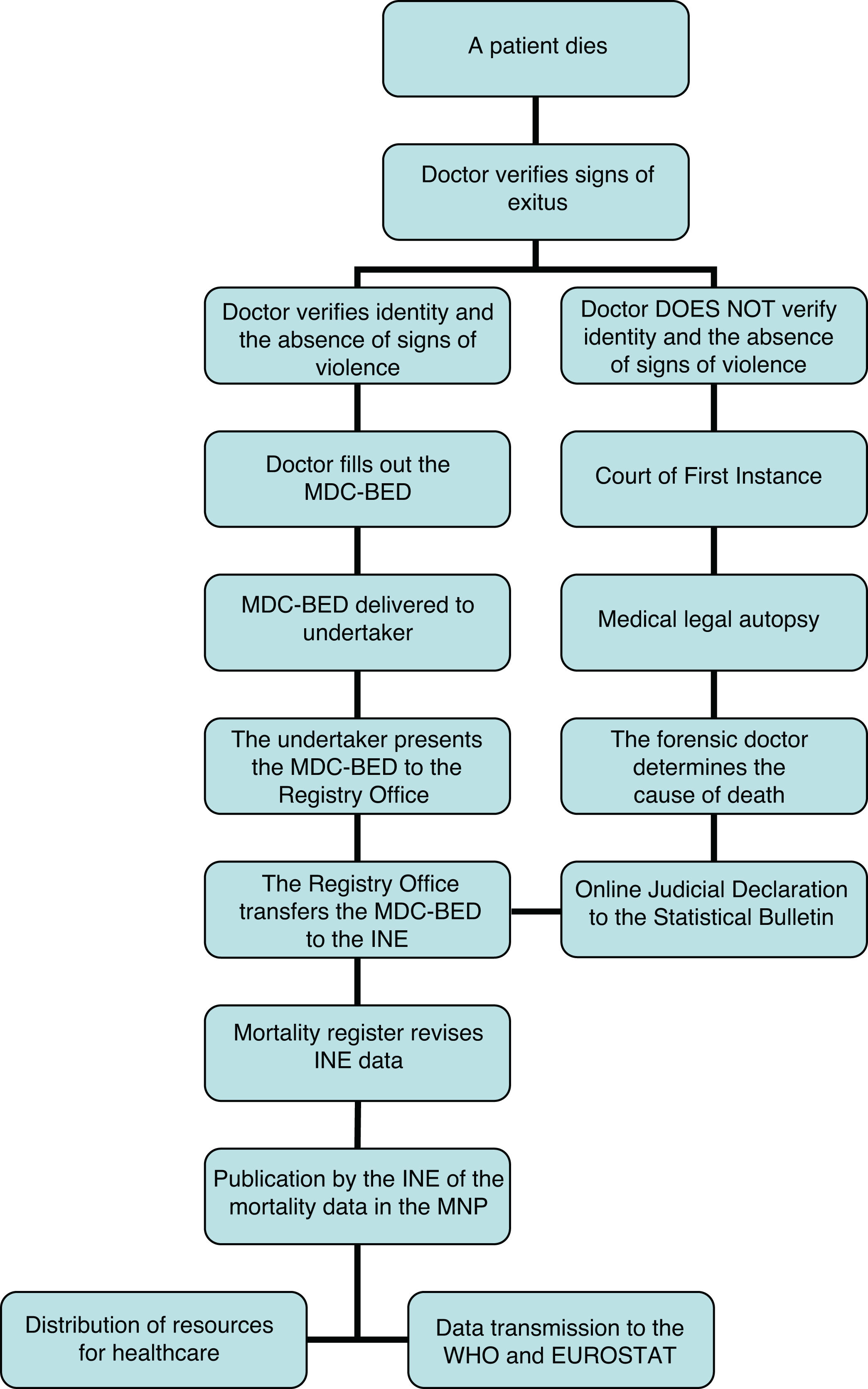
According to the Regulation that expresses the RO Law, the MDC-BED must be filled in by “the doctor who attended the dead individual during their final disease, or anybody else who recognises the corpse”.7 The Medical Ethics Code (EC)8 regulates the obligation to certify a death, stating that “although the doctor who has attended the patient the most is the one with the greatest ethical responsibility to fill out all of the sections of the death certificate, it is not ethically acceptable to reject the obligation to certify this when one has been present at the death, knows the patient or has access to the clinical history”. On the back of the first MDC-BED document we find certain “Basic instructions for certification” (Fig. 1) established by the WHO, to be followed when filling in the certificate. In the case of violent deaths or the suspicion of criminality the MDC-BED should not be signed, and these deaths should be referred to judicial investigation.9 The general procedure for the management and notification of deaths is shown in Fig. 2.
The MDC-BED is a medical–legal document in which a doctor should employ the same effort and dedication as in the other reports drawn up during the lifetime of the patient. Clinically and ethically, it is possible to sign a certificate using presumptive criteria if the outcome is possible and the information about the circumstances of death and the patient’s history of pathology. Nevertheless, it is not acceptable to sign it if shielding oneself in a possible offense of falsity contained in the Penal Code. Our experience and that of other authors confirms that it is unlikely that a doctor who, in good faith and after examining a patient, would be prosecuted after certifying a death as natural when it was not,10 it being an ethical duty to fill out the MDC-BED. In this situation the priority is to reduce the suffering of family members, over and above unreasonable legal doubts, humanising treatment under circumstances of such intense emotional suffering.11
Since it was published in 2009, the MDC-BED has undergone some modifications. In the first version of the MDC-BED what are now termed “intermediate causes” are also denominated “antecedent causes”. After less than 2 years, the INE found that this variable was being filled in mistakenly, and it drew up a document which was sent to doctors through the CM.12 This stated that “many doctors have interpreted this field to refer to clinical antecedents and not, as should be understood, noting in the [so-called] antecedent causes the process that due to the initial cause brought about the immediate cause of death”. Recently, these have been modified by including a QR code and recording the 9-figure membership number, in independent boxes to be appropriately filled out.
Correctly filling out the MDC-BED has important consequences in terms of medical policy. Based on them, the INE extracts the causes of death from these documents to generate official mortality statistics. According to the results obtained, measures for prevention are applied and the necessary resources are used to meet existing needs by implementing medical policies. Not filling out the causes of death correctly (Fig. 3) may be highly important in epidemiological terms.13 The result of this would be a poor organisation of the resources destined for health purposes, in terms of research into diseases as well as the implementation of preventive policies.
The medical death certificate during epidemicsThere is little experience in our field in connection with the certification of deaths during epidemics. It is understood that in case of multiple deaths, procedures for action may be similar to those used in catastrophes. As Barbería and Xifró14 state, catastrophes are a public health problem because they are likely to increase morbimortality and reduce quality of life. Epidemics clearly fulfil these criteria. The role of certification of the causes of death in major catastrophes corresponds to forensic medicine15 while certification in epidemics corresponds to healthcare providers.16 However, the comparison may be useful in establishing procedures for the management of corpses and certification of death in case of multiple deaths during epidemics.17
The sole example we have in Spain of an epidemic with multiple deaths and registration of the same is the influenza pandemic of 1918. This outbreak led to many scientific studies, statistical analyses and strong reaction by the press after May 1918. It was a terrible experience for society and gave rise to multiple ways of fighting it by governments, as well as an extraordinary response by healthcare professionals and the population in general. Studies of the influenza pandemic in 1918 have covered not only morbimortality data analysis, these data being intrinsically highly important, but have also led to an understanding of the epidemic that goes beyond statistics.
To be able to evaluate the repercussions of the influenza epidemic on mortality we have the information contained in the Movimientos naturales de población prepared by the INE and the monthly Medical Demography Bulletins published by the Ministerio de la Gobernación. Nevertheless, these data are not enough to allow us to go into detail. For example, they do not permit examination of data associated with city quarters. Porras-Gallo18 studied the demographic statistics drawn up annually by Madrid Town Hall Statistics Department, as well as the yearly summaries of the said Demographic Statistics. Crossing these data with those of the RO records and books of registered deaths corresponding to the years 1918 and 1919 made it possible to determine the evolution of morbimortality in detail during the pandemic in Spain.19
Nevertheless, in the past and like today, mortality statistics change depending on the criteria which are applied to them. Thus for example, in the case of Madrid, the gross rates of general mortality and the specific rates in 1918 and 1919 obtained from RO data and general annual summaries of the Demographic Statistics of Madrid Town Hall were very different. This was because deaths were registered in the district corresponding to the place of death, while the Town Hall prepared its statistics on the basis of cemetery data, where deaths were recorded in the district where the individuals had lived rather than the one where they had died. This is an example of the complexity of studies of historical morbimortality.18,20
National and international recommendations for the medical certification of deaths in connection with COVID-19On 29 March 2020, the CGCOM issued a communication in which, according to the definitions proposed by the WHO, the National Committee of Public Administrations reported on the procedure to be followed in certifying deaths during the current COVID-19 epidemic.16 This document states that deaths caused in an epidemic are natural deaths. There is no need to inform the medical-legal or judicial fields of deaths. The judicial intervention of the forensic doctor will be restricted to cases of violent death or those in which there is a clear suspicion of criminality. In these cases, in which investigating the death corresponds to the medical-legal field, the fact of having a positive PCR SARS-CoV-2 indicates a datum that is of epidemiological interest, one that should perhaps be taken into account as an aggravating factor if the death occurred at another time from the traumatic event. However, it corresponds to forensic professionals to analyse this possible contributory cause. In all other cases, certification of death corresponds to healthcare doctors, regardless of whether they work in the public or private domain, as is the case in other neighbouring countries.21,22 We said beforehand that when somebody dies, reducing the suffering of family members should take priority over any unreasonable legal doubts when certifying the death, humanising how they are treated in circumstances of such intense emotional suffering11: in circumstances such as those experienced during this pandemic, this principle is more necessary than ever.
The CGCOM document establishes 2 scenarios when certifying deaths due to COVID-19. The first refers to cases where although there is no analytical confirmation, the symptoms are compatible with the disease. In these circumstances it is recommendable to certify the fundamental cause of death as unconfirmed or suspected COVID-19 coronavirus infection. As the immediate cause the proposal is to use “multiple organ failure””, “respiratory distress” or “acute respiratory failure”. Intermediate causes may also be cited if there are any or if any are known, such as “pneumonia”, “sepsis” or “coagulation pathology”. The second scenario is that where COVID-19 have been confirmed by a laboratory test. In such cases the fundamental cause of death should be confirmed COVID-19.
An important question for all of the above scenarios is how to register comorbidity of patients who died due to COVID-19.23,24 The OMC document states that any existing diseases or comorbidities involving a greater risk of developing a serious disease should be recorded in the section referring to other processes: “cardiovascular diseases”, “arterial hypertension” or “diabetes”.
The question sometimes arises of whether to record death due to COVID-19 or death with COVID-19, and it may be hard to determine whether COVID-19 caused the death or whether it was a pre-existing disease. This has to be decided by the doctor who signs the certificate in the light of the data on the clinical evolution of the patient, which may require an in-depth study of their medical history. In any case, the content of the MDC-BED is evaluated later on by the professionals working in the Mortality Registries. This enables modifications to the fundamental cause of death after study of the clinical history and communicating, if applicable, with the professional who had certified the death at the time.
The CGCOM document is based on the WHO international guide for the certification of COVID-19. This was subsequently modified in a publication dated 16 April 2020, which contained examples for the certification of deaths not caused by COVID-19.25
To codify deaths the WHO establishes code U07.1 for deaths caused by COVID-19 and confirmed by analytical study, and code U07.2 for deaths without confirmation by a test, in which the diagnosis of COVID-19 is based on clinical or epidemiological criteria (probable or suspected).26
For the purpose of decision-making, this document uses the following differential definitions for “suspected” or “probable”. For those who survive the disease it defines cases as “probable”:
- •
When the patient has an acute respiratory disease (i.e., with fever and at least one sign or symptom of respiratory disease, such as coughing or difficulty breathing, for example), without any other aetiology that could completely explain the clinical manifestations, and with a history of travel or residency in a country, area or territory where local transmission of COVID-19 had been reported during the 14 days prior to the onset of symptoms;
- •
When a patient with an acute respiratory disease has been in contact with a confirmed or probable case of COVID- 19 during the 14 days prior to the onset of symptoms;
- •
When a patient with a severe acute respiratory infection (i.e., fever and at least one sign or symptom of respiratory disease, such as coughing or difficulty breathing, for example) and who required hospitalisation and has no other aetiology which completely explains the clinical manifestations.
The same WHO document defines suspected cases as those which are probable for which the laboratory test for COVID-19 has been performed without conclusive results.
Other bodies in different countries have expressed themselves in the same terms for recommendations on MDC-BED in this pandemic.27–29 The Italian model29 has the peculiarity that the chain of events in its model is inverted respecting what is usual: it starts with the basic cause and ends with the immediate cause.
Reporting deathsAs we said, the general procedure for managing and reporting deaths is shown in Fig. 2.
In Spain and other countries there has been clear controversy regarding the number of deaths caused by COVID-19.30 The daily mortality data for all causes is obtained from the General Notaries Registry of Births, Marriages and Deaths of the Ministry of Justice, distributed among all of the Autonomous Communities and including 52 provincial capitals. During the year 2020, the Mortality Monitoring System (MoMo) in Spain includes deaths due to all causes from 3929 computerised registry offices (through Inforeg), representing 92% of the Spanish population.31
During this crisis a delay has been observed in recording deaths in the RO due to the high number of deaths and the effects on working of the measures established because of the state of emergency. For this reason, the General Board of Judicial Security and Public Trust of the Ministry of Justice issued a circular so that the heads of the RO sent the number of burial licences issued every day to the Ministry of Justice.
Nevertheless, these measures do not include information on the causes of death. Swift and direct reporting of mortality registrations and the causes of the same would help to achieve a suitable level of knowledge regarding mortality in an epidemic crisis such as the current one. The procedure for reporting deaths to the INE by the RO currently consists of the monthly remittance of MDC-BED to the provincial offices of the INE. In terms of reporting deaths, the implementation of data transmission to report deaths would speed the process up and make this communication faster. Regarding obtaining information from the RO, Corera32 defends applying the new RO law as soon as possible,4 with a single computerised and electronically accessible RO for the whole of Spain. Deaths will be reported by data transmission when it comes into force, and this will, as the author says, undoubtedly offer faster knowledge of deaths.
Until such time as data transmission is used, it may be useful to establish exceptional procedures, such as the one introduced in Castile-La Mancha.33 Other suggestions, such as the participation of the Legal Medicine and Forensic Sciences Institutes (IMLCF) in specific mortality monitoring systems, would make it possible to learn of deaths in real time as well as their causes, in circumstances as exceptional as the current ones. This participation is based on the supervision of MDC-BED by forensic doctors working for the RO in some IMLCF in Spain. This task, which is usually restricted to large towns, could be expanded to the monitoring of the MDC-BED received in all of the RO in this community. Thus the IMLCF would report daily on the information contained in the MDC-BED to the public health services of each community. This participation, which has been successfully undertaken in Castilla y León, would bring great added value to the usual notification circuits.
From a practical point of view, we should be able to access sufficient death certificates, certificates that can be accessed in the provincial COM. In a pandemic, and especially in one where lockdown measures have been applied, fast and simple remittance mechanisms must be available between the COM and undertakers or medical organisations.
To conclude, we underline that filling out a MDC-BED is an important medical act. It requires evaluation of the whole pathological history of the patient, and it helps to humanise communications with the patient’s family in circumstances of intense emotional suffering. Mortality reporting methods have to be improved, creating the possibility of certification using data transmission. In epidemics and pandemics it is necessary to issue clear recommendations on certification by official bodies and establish, if data transmission cannot be used, faster circuits that make it possible to know mortality rates in real time.
Please cite this article as: Teijeira Alvarez R, León Sanz MP, Castro Herranz S, Floristán Floristán Y, Salazar Lozano MI, Moreno Iribas MC. La certificación de la defunción de casos de COVID-19 en España. Rev Esp Med Legal. 2020;46:101–108.