Sudden unexpected deaths in infancy (SUDI) represents a serious public health problem. The objective of this work is to analyze its epidemiological and clinical-pathological characteristics.
MethodRetrospective population study of SUDI in Bizkaia between 1991-2020. Data from the Mortality Registry and Forensic Pathology Service were examined.
Results1,109 deaths in children under one year were recorded. A forensic autopsy was performed in 107: 61 cases of sudden infant death syndrome (SIDS) and 23 SUDI of explained cause. In other 10 cases SIDS was coded as cause of death without forensic autopsy. The incidence of SIDS was 0.26/1,000/year and decreased from 0.74 (1991-1995 five-year period) to 0.07 (2011-15 and 2016-20 periods). The percentage of SIDS in relation to total mortality decreased from 11.2 to 2.5%. In SIDS, category IB from San Diego (67%) and infants between 1 and 4 months (63%) predominated. An “unsafe sleep environment” was detected in 6 SIDS. 56.5% of the explained SUDI were infectious. Of the 84 autopsied SUDI cases, 70% had no pre-existing disease and 15% were premature and/or low birth weight infants. In 32% there were prodromal symptoms, mainly respiratory tract infection. Microscopic findings suggestive of respiratory infection were diagnosed in 10 SIDS.
ConclusionsThe incidence of SIDS in Bizkaia is low and has decreased notably in the last 30 years. Prodromal symptoms and histopathological signs suggestive of infection are relatively common. Forensic studies provide relevant data, although prospective multidisciplinary and multicenter research would be desirable.
La Muerte Sudden del Lactante (MSL) representa un grave problema de salud pública. El objetivo del trabajo es analizar sus características epidemiológicas y clínico-patológicas.
MétodoEstudio retrospectivo poblacional de la MSL en Bizkaia entre 1991-2020. Se examinaron datos del Registro de Mortalidad y Servicio de Patología Forense.
ResultadosSe registraron 1109 defunciones en menores de un año. En 107 se efectuó autopsia forense: 61 síndromes de muerte sudden del lactante (SIDS) y 23 MSL de causa explicada. En otros 10 casos se codificó el SIDS como causa de muerte sin autopsia forense. La incidencia del SIDS fue de 0,26/1.000 recién nacidos/año y descendió desde 0,74 (quinquenio 1991-1995) a 0,07 (quinquenios 2011-2020). El porcentaje del SIDS en relación a la mortalidad total decreció del 11,2 al 2,5%. En el SIDS predominó la categoría IB de San Diego (67%) y los lactantes entre 1-4 meses (63%). Un “ambiente de sueño inseguro” se detectó en 6 SIDS. El 56,5% de las MSL explicadas fueron infecciosas. De los 84 casos de MSL autopsiados, el 70% no tenía enfermedades previas y el 15% eran prematuros y/o recién nacidos de bajo peso. En el 32% existieron síntomas prodrómicos, principalmente infección de vías respiratorias. Hallazgos microscópicos sugestivos de infección respiratoria se diagnosticaron en 10 SIDS.
ConclusionesLa incidencia del SIDS en Bizkaia es baja y ha disminuido notablemente en los últimos 30 años. La sintomatología prodrómica y los signos histopatológicos sugestivos de infección son relativamente frecuentes. En el futuro serían deseables investigaciones prospectivas multidisciplinares y multicéntricas.
Sudden infant death (SID) is a serious public health problem. Sudden infant death syndrome (SIDS) is the main cause of death during the first year of life in developed countries. It is defined as the sudden and unexpected death of a child under one year of age that occurs during sleep and remains unexplained following a complete post-mortem investigation that includes an autopsy with complementary analyses, an examination of the place where the death occurred and review of the clinical history.1–6 Due to their form of presentation such deaths are considered to be suspicious of criminality and are the object of forensic study.
SIDS has a complex and heterogenic pathogenesis. The triple risk theory is currently the most widely accepted, involving the interaction of environmental and biological factors in a vulnerable child during a critical period of development.7 Several environmental risk factors have been identified in recent decades, which has contributed to the implementation of prevention campaigns which have been effective in reducing its incidence.1–4 The most important risk factor is sleeping in an unsafe environment (prone, in a bed shared with adults or other children)2,4,5,6
A significant improvement in the study of SIDS arose from the standardization of diagnostic criteria using the San Diego Classification. This defines different categories based on the investigation of the circumstances and scene of death, clinical data, autopsy findings and complementary studies (Table 1).8 According to this classification, which was published in 2004, to be classified as SIDS a death has to be unexplained as well as having occurred during sleep.
SIDS categories in the San Diego classification.
| Category | Clinical criteria | Circumstances of death | Autopsy |
|---|---|---|---|
| IA | 21 days-9 monthsNormal clinical historyNormal development and growth No similar deaths | Investigation of the scene and circumstances A safe environment | No lethal findingsNo traumaNo thymic stress Negative complementary studies |
| IB | 21 days-9 monthsNormal clinical historyNormal development and growth No similar deaths | No investigation | A complementary study is lacking |
| II | < 21 days > 9 monthsPrematureNeonatal disease resolvedSimilar deaths | Possible mechanical asphyxia or suffocation (unproven) | Abnormal development and growth Changes or marked inflammatory abnormalities |
Source: Molina et al.[8]
In spite of these advances the aetiopathogenesis of SIDS is still unknown, so that multidisciplinary scientific studies are necessary to help clarify its risk factors. Forensic studies offer the necessary clinical, pathological, toxicological and epidemiological data to develop preventive policies. However, in Spain few forensic works on SIDS have been published, and of these the multicentre forensic study published in 2013 stands out. This analysed 488 cases of SID, of which 34% were unexplained.8 Another recent study in the Valencian Community also stands out. This covered a series of 138 infants who died suddenly in the period from 2006–2018, and it is the broadest at state level.5
The main aim of this work is to analyse the clinical, epidemiological and pathological characteristics of SID over the last 3 decades in a clearly defined population, Bizkaia. It analyses the forensic results corresponding to SIDS and cases of SID with a known cause, as well as Mortality Registry data.
Material and methodsPopulation studied and data sourcesThis is a retrospective populational study in infants under one year old who died due to natural causes in Bizkaia from 1991 to 2020. Bizkaia is an industrial province of the Basque Country, and it has a population of approximately 1,100,000 inhabitants. The population of infants under one year of age in the period analysed varied from 8,176 to 10,736. The birth rate ranged from 6.41 to 9.43 per 1,000 inhabitants, and the lowest birth rates correspond to the last five-year period.[9]
A forensic autopsy is a legal requisite for the investigation of violent deaths or ones where there is a suspicion of criminality, including SID. For other natural deaths the attending doctor has to fill out the medical death certificate (MDC). The causes of death shown on the MDC and in forensic reports are then coded according to the CIE-10 in the Mortality Registries.
Two data sources were used in this work: the Mortality Registry of the Autonomous Community of the Basque Country (EUSTAT) and Bizkaia Forensic Pathology Department of the Basque Institute of Legal Medicine.
Mortality registryThe following Mortality Registry variables were analysed: the cause of death, the origin of the registration of death (forensic vs. MDC) and sex of the deceased.
Forensic pathology departmentThe autopsy protocol for SID included the clinical history (pathologies and symptoms prior to death or prodromes), the circumstances of death, examination of the scene, the complete autopsy with macroscopic and microscopic examination of all of the organs, and toxicological analysis. The protocol changed during the period analysed in connection with the complementary studies. Biochemical analyses in the vitreous humour were occasionally required until 2011. Microbiological studies were routinely requested after 1996, to comply with the standardized international autopsy protocol for the study of sudden infant death. This protocol was agreed by the Perinatal and Infant Pathology Workgroup of the Spanish Society of Forensic Pathology.10
The cause of death and the San Diego category were established according to clinical and histopathological criteria. For this purpose the documents of the Forensic Pathology Department, those corresponding to the judicial proceedings, the police statements and the clinical history were all reviewed. The cases were divided into 2 groups: cases of SID that were explained (cases where a structural cause of death had been found) and unexplained cases of SID, where no cause of death was found. The latter cases were included as SIDS and categorized according to the San Diego Classification.
Epidemiological and statistical analysisThe annual rate of total mortality and SIDS in infants aged under one year per 1,000 live new births was calculated for the complete period studied (1991–2020) and for each five-year period. Statistical analysis was performed using the SPSS 21.0 package for Windows.
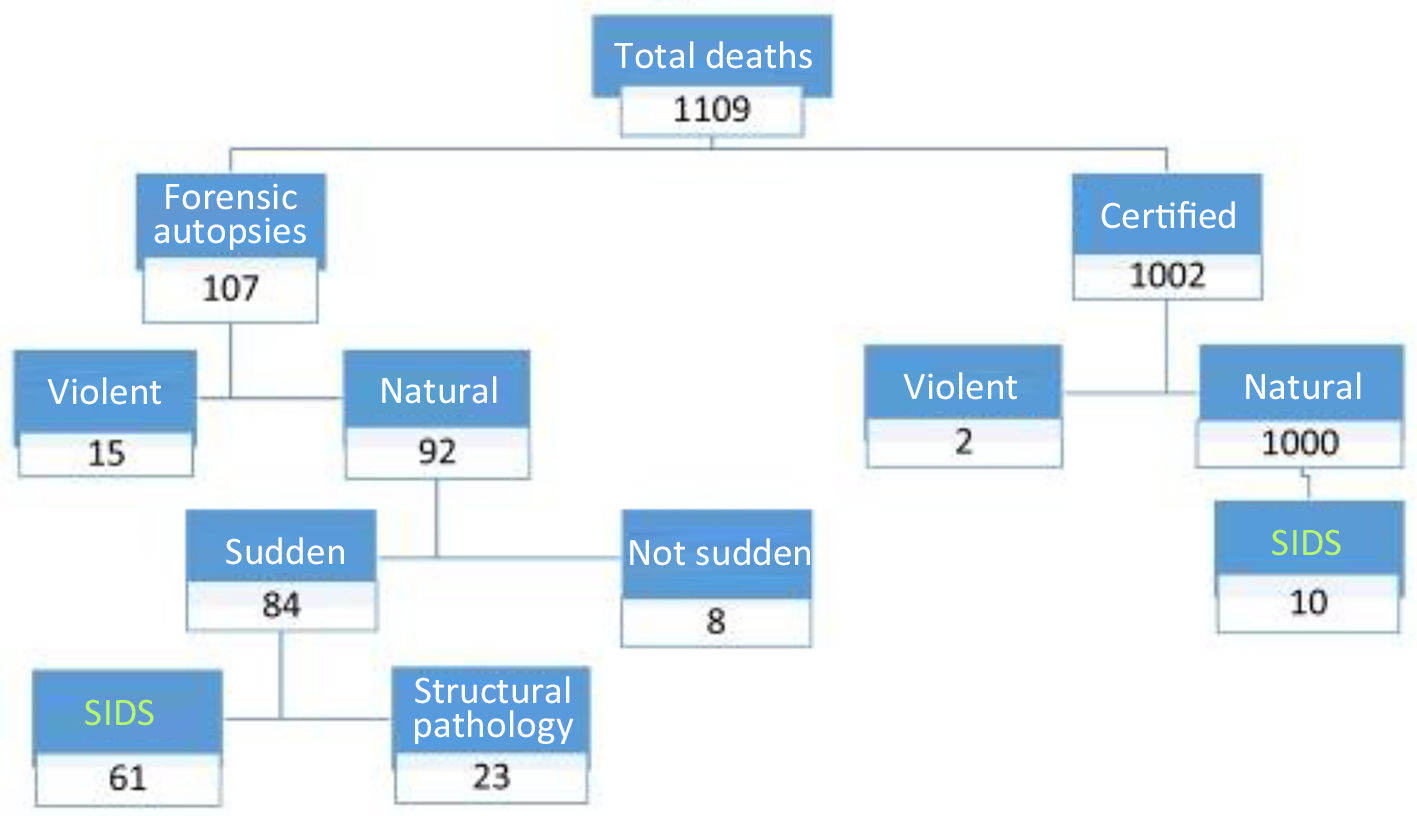
ResultsMortality registry data1,109 deaths occurred in infants under one year of age in Bizkaia from 1991 to 2020 (Fig. 1). A forensic autopsy was performed in 107 (9.6%) of these cases. 78% (n = 84) of the autopsies were classified as SID: 61 cases of SIDS (4 of these occurred before 2014 so are probable SIDS, as when they were evaluated again no information was found as to whether they had occurred during sleep) and 23 cases of SID with an explanation. On the other hand, in 10 cases of the deaths for which a MDC was issued (n = 1,002), SIDS was classified as the cause of death. Therefore a total of 71 cases of SIDS were recorded, of which 59% (n = 42) corresponded to male infants.
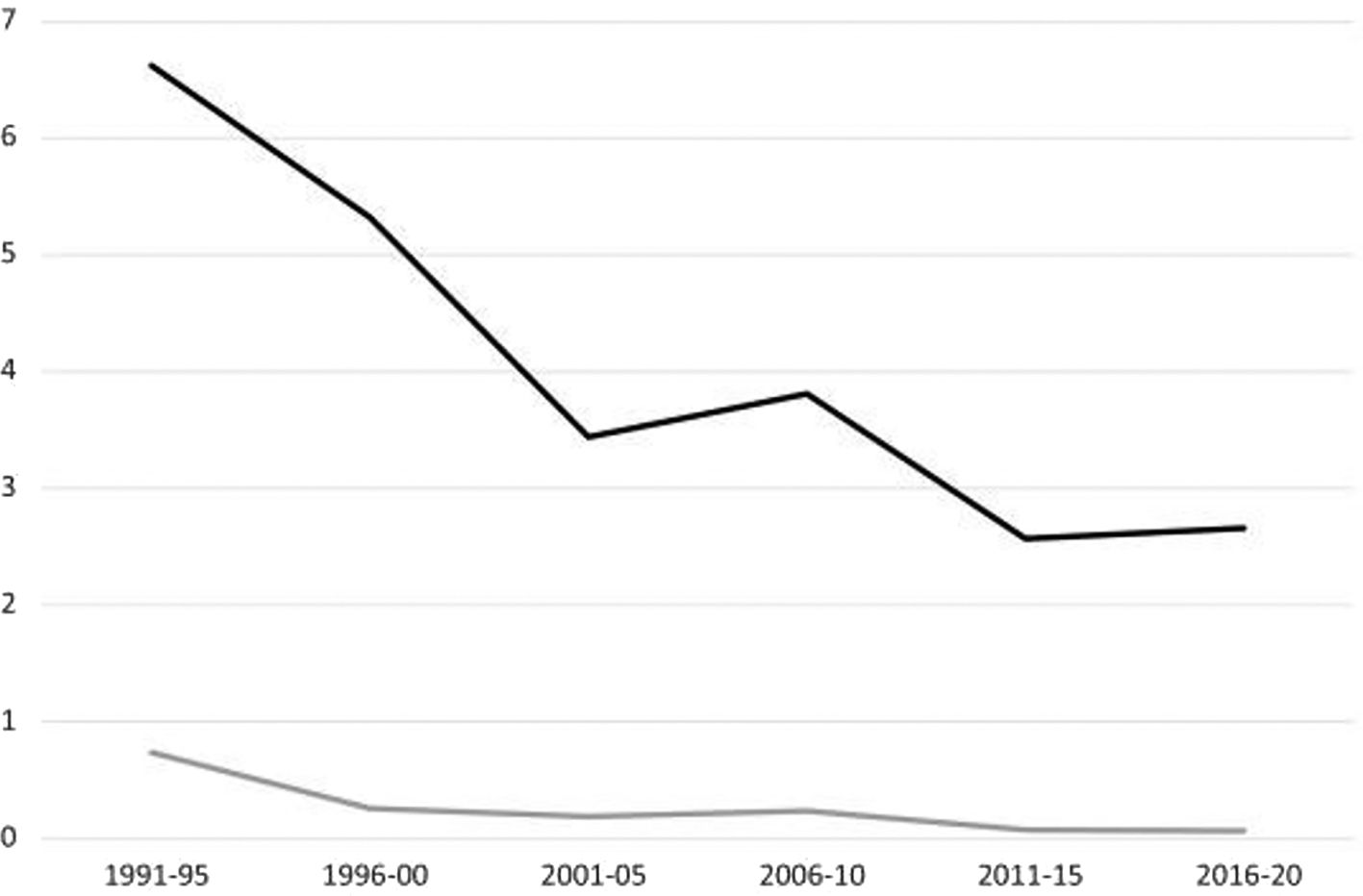
In the period 1991–2020, the total mortality rate in infants aged under one year was 4.06 and the corresponding rate of SIDS was 0.26/1,000/year. Respecting the distribution per five-year period, the absolute figure (Table 2) and the incidence (Fig. 2) of the total number of deaths and for SIDS fell gradually, chiefly in the first 2 five-year periods (Fig. 2). The recorded incidence of SIDS fell the most quickly from the first (rate 0.74) to the second 5-year period (rate 0.26); it remained stable in the next 3 5-year periods, before falling against in the 5th and 6th lustra (incidence rate 0.07). (See Fig. 3.)
Distribution of total infant mortality in those aged under one year and SIDS in five-year periods (Mortality Registry data).
| 5-year period | Population < 1 year of age | Total mortality (N) | SIDS(N) | Percentage (%) SIDS/Total |
|---|---|---|---|---|
| 1991–95 | 8,490 | 276 | 31 | 11.2 |
| 1996–00 | 8,276 | 221 | 11 | 5 |
| 2001–05 | 9,574 | 163 | 9 | 5.5 |
| 2006–10 | 10,736 | 200 | 13 | 6.5 |
| 2011–15 | 9,974 | 132 | 4 | 3 |
| 2016–20 | 8,176 | 117 | 3 | 2.5 |
| Total | 1,109 | 71 | 6.4 |
Changes in the annual rates of total mortality in children under one year of age and SIDS in five-year periods (Mortality Registry data). The total rate of mortality in infants aged less than one year (black line) and the SIDS rate (grey line) are shown in No. of cases/1,000 live births/year.
During the period 1991–2020, 6.4% of the total number of deaths in infants under one year of age were due to SIDS. This percentage gradually fell, from 11.2% in the first five-year period to 2.5% in the last five-year period (Table 2).
Sudden infant death data from the Forensic Pathology Department of Bizkaia (forensic autopsy)
The distribution of 61 cases of SIDS and 23 cases of SID with a known cause over five-year periods is shown in Figure. While a falling trend may be seen for SIDS, the frequency of SID with a known cause remained stable.
Death caused by infections predominate in cases of SID with a known cause (56.5%), chiefly lung infections, among which interstitial pneumonia stands out (n = 5). Congenital disease is located in second place (n = 5) (Table 3).
Sudden death with a known cause (N = 23).
| Causes of structural sudden death | n (%) |
|---|---|
| Infection | 13 (56) |
| Interstitial pneumonia | 5 |
| Bronchopneumonia | 3 |
| Lymphocytic myocarditis | 2 |
| Miliary tuberculosis | 1 |
| Botulism | 1 |
| Meningococcemia | 1 |
| Congenital disease | 5 (22) |
| Cardiac malformations | 2 |
| Intraparenchymal cerebral haemorrhage due to AVM | 1 |
| Disease cause by lipid deposition | 1 |
| Lowe’s syndrome | 1 |
| Others | 5 (22) |
| Cerebral haemorrhage of unknown origin | 2 |
| Meconium aspiration syndrome/amniotic fluid | 2 |
| Bronchopulmonary dysplasia | 1 |
AVM = Arterial-venous malformation.
Of the 61 cases of SIDS, 20 (33%) were classified as category II of the San Diego Classification based on the following criteria (which are not mutually exclusive): age < 21 days or > 9 months (n = 4); prematurity (n = 4); resolved neonatal disease (n = 2), unsafe sleeping environment (n = 6) and changes or marked inflammatory abnormalities (n = 6). The others were classified as category IB, as all of the complementary studies necessary to classify a SIDS as IA were not performed in any case, and/or the environment and circumstances of the death were unknown.
The scene of death was only examined in 44% of the total number of SID cases (Table 4).
Clinical history of the cases of SIDS and SID with a known cause subjected to forensic autopsy (n = 84)a.
| SIDSN = 61 | SID known cause N = 23 | TotalN = 84 | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sex | |||
| Male | 38 (62) | 12 (52) | 50 (59) |
| Female | 23 (38) | 11 (48) | 34 (40) |
| Age (months) | |||
| ≤1 month | 3 (5) | 6 (26) | 9 (11) |
| 1–4 months | 45 (74) | 8 (35) | 53 (63) |
| >4 months | 13 (21) | 9 (39) | 22 (26) |
| Season | |||
| Spring | 12 (20) | 3 (13) | 15 (18) |
| Summer | 13 (21) | 3 (13) | 16 (19) |
| Autumn | 17 (28) | 6 (26) | 23 (27) |
| Winter | 19 (31) | 11 (48) | 30 (36) |
| Source of cadavera | |||
| Unknown | 1 | 0 | 1 |
| Removed | 28 (47) | 9 (39) | 37 (44) |
| Dead on arrival | 32 (53) | 12 (52) | 44 (53) |
| Death in Emergency Department | 0 | 2 (9) | 2 (2) |
| Activitya | |||
| Unknown | 5 | 8 | 13 |
| Sleeping | 56 (100) | 7 (47) | 63 (89) |
| Other | 0 | 8 (53) | 8 (11) |
| Clinical historya | |||
| Unknown | 4 | 1 | 5 (6) |
| None | 47 (82) | 8 (36) | 55 (70) |
| Diagnosed with the disease while alive | 0 | 4 (18) | 4 (5) |
| Prematurity/or low weight new bornb | 4 (7) | 8 (36) | 12 (15) |
| Other minor factorsb | 8 (14)b | 4 (18) | 12 (15) |
| Prodromesa | |||
| Unknown | 9 | 3 | 12 |
| No | 39 (75) | 10 (50) | 49 (68) |
| Yes | 13 (25) | 10 (50) | 23 (32) |
| Respiratory infection | 9 | 2 | 11 |
| Feverish syndrome | 3 | 3 | 6 |
| Gastroenteritis | 1 | 1 | 2 |
| General discomfort | 0 | 4 | 4 |
59% of the SID were male. The median age was 3 months, and percentiles 25 and 75 are 2 and 5 months, respectively. 26% of cases of SID with a known cause were less than one month old, while in the SIDS cases the corresponding percentage was 5%. The majority of the SIDS cases (74%) were concentrated between one and 4 months of life (Table 4).
SID occurred the most often (63%) in the months of autumn and winter. In 6 infants who died due to SIDS, death was associated with an “unsafe sleeping environment”: 5 because they shared a bed, and one who appeared with their head covered by a sheet.
Clinical dataIn 70% of cases (36% in the SID group with a known cause vs. 82% in SIDS) no relevant previous illness was recorded. A history of prematurity and/or new born with low weight were present in 15%. In 50% of SID with a known cause and in 25% of SIDS cases prodromal symptoms were recorded which evolved over less than 24 hours. The majority of symptoms were associated with infection, chiefly symptoms of upper airway infection or bronchitis (Table 4).
Complementary studiesA toxicological analysis was requested in 81 of the 84 cases. All of them were negative for substances of abuse. Drugs to bring down fever and/or antibiotics were found in therapeutic concentrations in 7 infants.
Histopathological analysis was decisive in diagnosing the cause of death in the majority of the SID cases with a known cause (Table 3). In SIDS, microscopic study showed discrete inflammatory infiltrates (which were not important enough to explain the death) in the respiratory system in 6 cases: laryngotracheobronchitis (n = 3) and pulmonary inflammatory infiltrate that was insufficient for the diagnosis of interstitial pneumonia (n = 3). Granulomas were detected in 2 cases: necrotizing in the liver (n = 1) and non-necrotizing in the liver and lungs (n = 1). Other microscopic findings with one case each were focal myocarditis, focal esophagitis, microvesicular steatosis and suprarenal gland neuroblastoma.
In 19 autopsies of the SIDS group, biochemical studies were requested that supplied no relevant data. In the 34 autopsies corresponding to SIDS microbiological studies were requested that gave negative or inappreciable results except in 2 cases: a human herpesvirus (HHV-6) was isolated in one case, and in the other a type A influenza virus (H1N1) was detected in an infant with prodromal symptoms of catarrh. Nevertheless, there was no histopathological correlation in either of the 2 cases.
DiscussionIn this study in Bizkaia during the period 1991–2020, SIDS was the main cause of sudden death in infants under one year old (73% in our work), which is a higher percentage than those in other published series.11
Cases of SID with a known cause amounted to 27%, a percentage that falls within the broad margin - from 20% to 57% - of the different studies. The most common disease in SID with a known cause is infection (56% in our series) followed by congenital malformations.5,11 In spite of the major advances that have been made in prenatal diagnostic techniques, a sudden death may exceptionally be the first manifestation of these malformations.
Epidemiology of SIDSIn Bizkaia from 1991 to 2020 a gradual fall was detected in the total mortality of infants under one year of age, and this has also occurred in almost all industrialized countries. This falls may be partially explained by the reduction in the incidence of SIDS.1,2,12–14
Based on our study, there are several indicators according to which the impact of SIDS on infant mortality has fallen since the 1990s to date. The main indicator is the marked and progressive fall in its incidence. In the first five-year period the mortality rate was 9 times higher than it was in last 2 periods (2011–2020). Another relevant datum is the decline in the percentage of SIDS respecting the total mortality in infants under one year of age, which fell from 11.2% to 2.5%. The third indicator is that while SID with a known cause has remained stable, SIDS has not. While in the first five-year period 90% of SID cases were SIDS, from 1996–2010 the corresponding percentage was 66% and from 2011–2020 it was 35%. These findings indicate that SIDS is no longer a clearly dominant factor in infant mortality.
These data agree with the fact that the preventive campaigns implemented in Western countries in the 1990s led to a fall in the incidence of SIDS.1,2,12–14 A study which analysed mortality rates in the years 1990 and 2000 found a generalized fall in 13 countries of from 50% to 75%.13 The corresponding percentage in Bizkaia was 71%. Nevertheless, from 2011 onwards the rate has stabilized, so that work is still necessary in the fields of research and prevention.5
The incidence of SIDS varies widely geographically and over time. In the developed countries the annual rate over recent decades ranged from 0.1 to 0.5 per 1,000 live births.1,2,12–14 The annual rate in Bizkaia over the entire period (1991–2020) was 0.26, and in the last 2 five-year periods it was less than 0.1. These figures are among the lowest described. In the Valencian Community from 2006–2018 the annual incidence per 1,000 live births was 0.12, ranging from 0.05–0.17.5 Unlike Bizkaia, in the Valencian Community no fall was detected after the five-year period 2006–2010.
Different works should be compared with caution due to several reasons: diagnostic criteria vary, as does the percentage of cases in which an autopsy was performed. There is little rigour in applying the San Diego Classification, and there are no precise diagnostic markers for SIDS and other potentially lethal entities such as asphyxia in unsafe sleeping environment, etc.6,15,16
Demographic dataIn connection with SIDS, the results agree with those found by the majority of studies:5,16–19 there is a higher proportion of the male sex (62%) and those aged from the 1st to the 4th months of life (74%), indicating greater vulnerability in this critical period of development. Nevertheless, in the deaths with a known cause - and contrary to other findings in the literature -, no differences exist in terms of distribution according to sex.18 Unlike SIDS, in SID with a known cause the high incidence of cases during the first month of life stands out (5% vs. 26%), and this was also found in the series of infants in the Valencian Community, where neonatal problems and congenital malformations stood out.5
The increased prevalence of SID in autumn and winter months, coinciding with epidemics of respiratory viruses, has been described in other works.5,20,21,22
Clinical dataSIDS occurs in previously healthy infants: up to 82% had not previously been diagnosed with any relevant disease while alive. On the contrary, and in agreement with what other series describe,5,23 previous disease is the most common condition in the deaths with a known cause. Prematurity and low weight at birth are two of the most important risk factors for infant mortality and SIDS, in comparison with newly born infants at term. In our work this factor was recorded in 15% of the cases of SID, although this figure is lower than those in other series.5,24
The presence of clinical signs (prodromes) of mild infections in the days before death, which occasionally ran sub clinically, is a relatively frequent finding. Such infections may function as triggers for SIDS in a vulnerable infant.25,26 In our series, 25% of the SIDS cases had a symptoms suggestive of a viral infection, chiefly of the upper airways. This symptoms was even more common in the cases of SID with a known cause.
The most common risk factor for infants in their sleeping environment in the Valencia series was sharing a bed. This factor was present in 42% of SID cases, of which the majority were classified as SIDS (85%).5 In other series3,27 the frequency of bed sharing varied from the Bizkaia figure (10%) to those of Valencia. In Bizkaia, this risk factor was present less often, and other risk factors such as sleeping in prone decubitus, overheating, etc. were not taken into account. Nevertheless, this 10% figure may be an underestimate, given that the body was only removed in 47% of the SIDS cases.
Complementary study data in SIDSAs the literature states, the histopathological findings in SIDS are not specific and therefore are not important enough to be life-threatening.28 In our series, the most relevant findings (n = 6) were inflammatory alteration which suggested infection, observed at different levels of the airway and in the lungs. These histopathological signs which suggest infection and the relatively high frequency of prodromal symptoms in the days before death are considered to raise the possibility that an infection is the event which triggers SIDS.16,19
A virus was only isolated in 2 cases of the 34 in which a microbiological study was performed, amounting to 6%. These are very low figures and a lack of correlation between micro- and histo-pathology may be underlined, which is shared with other works.29 This datum may be explained by the existence of very old cases in which the microbiological study was of lower quality, due to difficulties in the interpretation of the post-mortem microbiological analysis, or because the infection occurred quickly with minimum histological changes.
LimitationsThe retrospective design of this study prevented the analysis of certain risk factors associated with the sleeping environment of the infants. In half of the cases the infant was taken to the Emergency Department, where they were found to be dead on arrival, so that no formal removal of the body took place. The result of this is a loss of valuable information about the circumstances of death and examination of the scene, as these are primordial when evaluating environmental risk factors such as sleeping in unsafe surroundings. The frequencies of certain risk factors may therefore have been underestimated in our work. Furthermore, in 4 cases catalogued as SIDS in the forensic reports that were issued at the time, it is not known whether death occurred during sleep. These are therefore probable cases, as the San Diego Classification requires death to have occurred during sleep.
Another limitation is that during the first five-year periods no microbiological studies were requested. No routine microbiological studies were carried out either, due to their complexity. Molecular autopsy technique has not been used, although within the short term this will probably become a habitual diagnostic tool in the investigation of SIDS because of the increasing amount of knowledge about its underlying genetic causes.
Lastly, the size of the sample is relatively small, and it is based solely on the experience of a population within a single province. Given this, it would be interesting to undertaken multicentre forensic studies.
ConclusionsThe incidence of SIDS has fallen markedly since the 1990s to date, and the rate in Bizkaia is one of the lowest described anywhere in the world (0.26 per 1,000 live births for the whole period). The percentage of SIDS in comparison with total infant mortality and total SID cases has fallen considerably, while the cases of death with a known cause remained at similar levels over the 30 years studied.
The highest number of SIDS cases occur from the first to the fourth months of life. This is the most vulnerable stage for infants, with a slight predominance of the male sex.
The relatively high frequency of prodromal infection symptoms and histopathological signs which suggest infection stand out, as infections may have triggered SID in vulnerable infants.
The causes of 27% of SID cases were explained. Without an autopsy, some of them may have been considered to be SIDS. A MDC should never be issued in case of sudden infant death or a violent death (of which there were 2 cases in this series), and the forensic process should always be activated. Forensic autopsy is an indispensable tool to discover the causes and mechanisms of death, as well as risk factors.
A forensic investigation should always be protocol-governed and meticulous. The autopsy should always include a study of the infant’s sleeping environment and their personal and family histories of pathology. A case of SID will therefore always require the intervention in person of the forensic doctor in the procedure of the removal of a cadaver. The protocols governing the actions of legal medicine institutes should be strengthened to ensure that a complete analysis of risk factors is carried out. This requires examination of the scene even when the infant has been admitted as a cadaver to a hospital or health centre, something which on the other hand occurs quite habitually. Complementary toxicological, histopathological and microbiological studies are essential for the correct categorization of a SID.
We would like to thank the members of Bilbao Forensic Pathology Department for their cooperation with this study, and Covadonga Audicana for her help with Mortality Registry data.
The described work has been published previously in the context of Eneko Belmonte’s dissertation.
Please cite this article as: Belmonte E, Monzó A, Morentin B. Evolución epidemiológica y causas de muerte sudden en lactantes: estudio poblacional desde 1991 a 2020 en Bizkaia. Revista Española de Medicina Legal. 2022. https://doi.org/10.1016/j.reml.2022.06.002