Obstetrics and gynecology is one of the specialties most involved in malpractice claims. However, there are few studies that provide scientific information on this topic. The aim was to analyse the characteristics of medical liability rulings in Spain in public healthcare in the speciality of obstetrics and gynecology.
MethodsCross-sectional observational study that analysed the rulings handed down in the contentious-administrative jurisdiction by the Superior Courts of Justice (2008–2020), in the speciality of obstetrics and gynecology. The variables were administrative, clinical, judicial, and compensatory.
ResultsWe analysed 1015 rulings, of which 142 (13.99%) related to the speciality of obstetrics and gynecology. A total of 67.61% of the rulings were dismissed at first instance and 89.28% at second instance. The most frequent reasons for an upheld ruling were diagnostic and/or therapeutic malpractice (40.90%), lack of information (20.45%), and loss of opportunity (18.18%). The most frequently claimed damage was sequelae (66.14%). The median award was 53 758.50 euros (2000–800 000).
ConclusionsThe high frequency of claims in obstetrics and gynecology indicates that these are “high risk” specialties for litigation. The vast majority of judgements are dismissed, i.e. in favour of the administration. The analysis of these results helps to structure the role of lawsuits and to increase professionals' knowledge of the medico-legal aspect of healthcare.
La obstetricia y ginecología es una de las especialidades más involucradas en las demandas por mala praxis. Sin embargo, existen pocos estudios que aporten información científica sobre este tema. El objetivo fue analizar las características de las sentencias sobre responsabilidad médica en España en la asistencia sanitaria pública en la especialidad de obstetricia y ginecología.
MétodosEstudio observacional transversal que analizó las sentencias dictadas en la jurisdicción contencioso-administrativa por los Tribunales Superiores de Justicia (2008–2020), en la especialidad de obstetricia y ginecología. Las variables fueron administrativas, clínicas, judiciales e indemnizatorias.
ResultadosSe analizaron 1.015 sentencias, de las cuales 142 (13,99%) se refirieron a la especialidad de obstetricia y ginecología. Las sentencias fueron desestimatorias en un 67,61% en primera instancia y el 89,28% en segunda instancia. Los motivos de sentencia estimatoria más frecuentes fueron la mala praxis diagnóstica y/o terapéutica (40,90%), el déficit de información (20,45%) y la pérdida de oportunidad (18,18%). El daño más reclamado fueron las secuelas (66,14%). La mediana de las indemnizaciones fue 53.758,50 euros (2.000–800.000).
ConclusionesLa alta frecuencia de las demandas en obstetricia y ginecología indica que se trata de especialidades de «alto riesgo» de litigiosidad. La inmensa mayoría de las sentencias son desestimatorias, es decir, a favour de la administración. El análisis de estos resultados coadyuva a estructurar el papel de las demandas judiciales y a aumentar el conocimiento de los profesionales en la vertiente médico-legal de la asistencia sanitaria.
Medical liability is now considered a public health problem and is a major concern for professionals, health systems, and patients. In fact, the World Health Organisation has taken a special interest in studying the policies of various countries in relation to obstetric malpractice.1 This is primarily because the study of negligence may help to reduce harm and thus improve patient safety.2 The literature on negligence is largely confined to the English-speaking world, which is a handicap when comparing our results, as healthcare systems, legal systems, and the social context itself are very different. Given the paucity of research on this topic, this is a perfect scenario for fears of a liability claim to emerge. Defensive medicine is the most common response to this, which has collateral effects throughout the healthcare system.
The risk of a physician being sued or facing a claim depends on several factors, one of which is the specialty.3 Obstetrics and gynaecology is recognised worldwide as a high-risk specialty4; that is, the likelihood of being sued is higher than in other specialties. In addition to the high number of claims brought against it, the specialty tends to see the most claim payouts.5 This speciality has 2 aspects, obstetrics, dedicated to the care of women before, during, and after childbirth, and gynaecology, which focuses on the diagnosis and treatment of diseases of the female reproductive system. Most claims made are related to obstetrics, internationally6 and in Spain.7
Medical malpractice in the Spanish public health system has seldom been the subject of study in the specialty that covers the gynaecological and reproductive health of women throughout their lives. We must emphasise that the liability that can be claimed falls within the lex artis ad hoc, in other words, there is an obligation of means and not of result, which includes the right to information. Therefore, there is no obligation to cure, but rather to use all the means available according to the state of science at the time the healthcare is provided. In this sense, the link that is commonly made between medical error and negligence must be highlighted. It must be emphasised that error by itself, or a harmful outcome, does not give rise to liability, the error has to have been negligent. Moreover, in the Spanish public system, the claim is received by the administration and never directly by the professional.
This research study aims to determine the characteristics of rulings on financial liability in the specialty of obstetrics and gynaecology in Spain. Thus, an in-depth study of malpractice rulings can improve how professionals and institutions manage the risks inherent in clinical practice. We also believe that it can contribute to reducing fear and, therefore, defensive practices.
MethodsThis is a cross-sectional observational study of healthcare liability rulings in the higher courts of justice (chambers of administrative litigation) in Spain, handed down between January 2008 and August 2020. Supreme Court rulings are excluded, since access to cassation is extraordinarily restricted, and therefore their inclusion would produce clear biases in the final results. Criminal jurisdiction is also excluded, as it refers to actions or omissions constituting criminal offences. Likewise, we exclude civil jurisdiction because it primarily concerns private healthcare.
From a methodological perspective, both first and second instance judgements are included. At this point, it should be borne in mind that, depending on the case, the higher courts of justice may rule in the first and only instance, or in the second instance when the case has been previously settled by a lower court (Administrative Court). The variability of one case or the other depends on the amount claimed and the body of the health administration that has the competence to resolve the prior claim. It should also be noted that in liability claims in the field of public healthcare, claims can only be brought against the corresponding health administration and not directly against the professional involved in the case.
The public database CENDOJ (Judicial Documentation Centre) was used for the analysis of the rulings. The search key was “responsabilidad patrimonial sanitaria” (healthcare liability), obtaining a first group of 11 767 rulings. The variables studied and collected through a data sheet by year are classified into 4 sections: (a) administrative: instance, appellant; (b) clinical: scope of the medical act, specialty involved, medical activity involved; (c) judicial: damage claimed, reason for the ruling and award, and (d) amount of compensation.
The sample size was obtained using the Granmo 7.12. programme (sample size calculator), which measures various parameters to perform the calculation. In this case, given the absence of previous data on the prevalence of rulings, an estimated proportion of p=.50 was taken, with a confidence level of 95% (alpha=0.05) and a precision of 5%. This resulted in a sample size of at least 350 rulings. To increase the reliability of the data, it was decided to extend the sample to 1015 rulings. A total of 80 rulings per year were included, except in 2020 when 55 rulings were included, because 8 months of the year were evaluated. The sampling was systematic, with analysis of 1 out of every 8 rulings included in the CENDOJ database. There were 3 inclusion criteria: clinical motivation of the judicial pronouncement, consequences for the patient, and amount of compensation. Rulings that merely reject the claim on formal grounds (e.g., limitation period for claiming); rulings in which more than one specialty is involved; rulings that arise from claims in which claims were made against the insurance company only, and rulings not related to the object of the study were excluded.
The descriptive statistics are performed as a whole and separately according to the specialties studied. The categorical variables are shown as absolute values, percentages, and 95% confidence interval (CI), and the quantitative variable as median and interquartile range (IQR). For the quantitative variable, the type of distribution was checked beforehand using the Kolmogorov–Smirnov Z-test. The Kruskal–Wallis test, which is a non-parametric test, was used to compare quantitative variables with qualitative variables. This was used to test whether the relationship between a categorical variable and a quantitative variable (in terms of median) is statistically significant. In this case, p-values <.05 are considered significant. The data were analysed using IBM SPSS Statistics version 24 (Licence Python 2.7.6. and 3.4.3.).
ResultsOf the 1015 claims, traumatology and orthopaedic surgery was the specialty against which the most were brought, 172 cases (16.90%; 95% CI: 14.68–19.39). In second place, the specialty of obstetrics and gynaecology was involved in 142 cases (13.99%; 95% CI: 11.91–16.27). Obstetrics had 77 cases (54.23%; 95% CI: 45.66–62.60), gynaecology 62 cases (43.66%; 95% CI: 35.36–52.23), and 3 missed cases (2.11%; 95% CI: 0.43–6.05).
In the first instance, there were 105 cases (73.94%; 95% CI: 65.91–80.94) and in the second instance, 37 (26.06%; 95% CI: 19.05–34.08). In the second instance, if the appellant was the patient and/or family, there were 28 cases (75.67%; 95% CI: 58.80–88.22) and if the appellant was the health service and/or the insurer, there were 9 cases (24.32%; 95% CI: 11.77–41.19).
Action was non-urgent in 131 cases (92.25%; 95% CI: 86.56–96.07) and urgent in 11 cases (7.75%; 95% CI: 3.93–13.43).
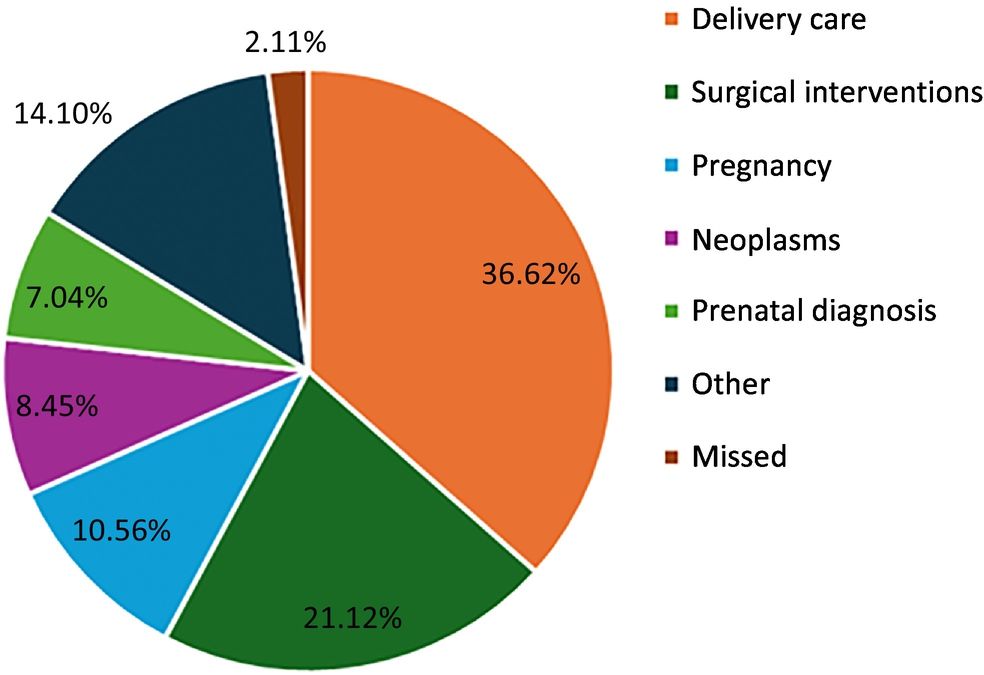
The medical activities involved in the claims were: 52 cases related to delivery care (36.62%; 95% CI: 28.70–45.11), 15 cases to pregnancy follow-up (10.56%; 95% CI: 6.03–16.82), 10 cases due to prenatal diagnosis (7.04%; 95% CI: 3.42–12.57), 12 cases due to neoplasms (8.45%; 95% CI: 4.44–12.29), 30 cases due to surgical interventions (21.12%; 95% CI: 14.73–28.76), 20 cases classified as other (14.08%; 95% CI: 8.82–20.91), and 3 missed cases (2.11%; 95% CI: 0.43–6.05). Fig. 1 shows the medical activities involved in the claims.
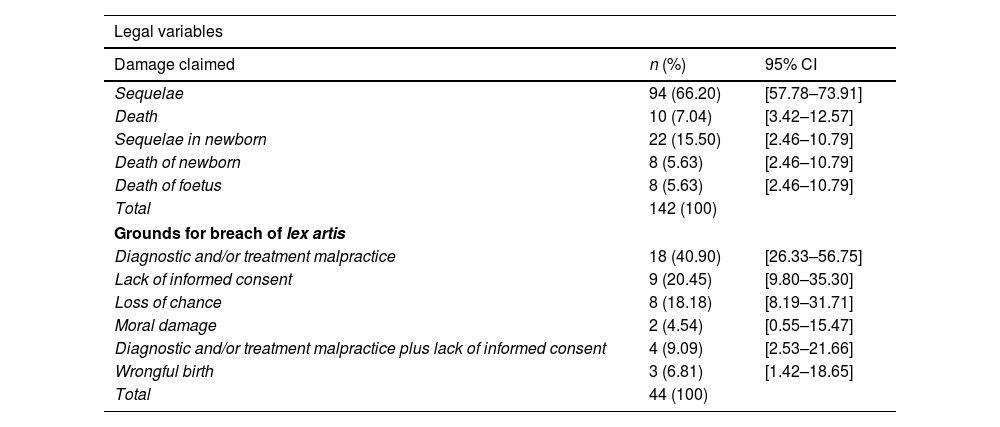
Among the legal variables, the damages claimed were: sequelae in 94 cases (66.20%; 95% CI: 57.78–73.91), death in 10 cases (7.04%; 95% CI: 3.42–12.57), newborn (NB) sequelae in 22 cases (15.50%; 95% CI: 9.91–22.51), NB death in 8 cases (5.63%; 95% CI: 2.46–10.79), and dead foetus in 8 cases (5.63%; 95% CI: 2.46–10.79).
Of the 142 rulings, breaches of best clinical practice (lex artis) were detected in 44 cases (30.98%; 95% CI: 23.50–39.28) on the following grounds: malpractice in diagnosis and/or treatment, 18 cases (40.91%; 95% CI: 26.33–56.75); lack of information, 9 cases (20.45%; 95% CI: 9.80–35.30); and for dead foetus, 9 cases (20.45%; 95% CI: 9.80–35.30); loss of chance in 8 cases (18.18%; 95% CI: 8.19–32.71); diagnostic and/or treatment malpractice plus information deficit, 4 cases, (9.10%; 95% CI: 2.53–21.66); wrongful birth, 3 cases (6.82%; 95% CI: 1.42–18.65), and moral damage, 2 cases (4.54%; 95% CI: 0.55–15.47).
In the first instance ruling variable, out of a total of 105 cases, 71 cases were dismissed (67.62%; 95% CI: 57.78–76.42), 33 cases were partially upheld (31.43%; 95% CI: 22.71–41.21), and fully upheld (0.95%; 95% CI: 0.02–5.19). In the second instance, out of a total of 37 cases, if the appellant was the patient and/or the family (28), 25 cases were dismissed (89.29%; 95% CI 71.77–97.73) and 3 cases were partially upheld (10.71%; 95% CI 2.26–28.22). When the appellant was the health service and/or the insurer (9), 3 cases were dismissed (33.33%; 95% CI: 7.48–70.07), 3 cases were partially upheld (33.33%; 95% CI: 7.48–70.07), and 3 cases were fully upheld (33.33%; 95% CI: 7.48–70.07). Table 1 shows the legal variables.
Legal variables.
| Legal variables | ||
|---|---|---|
| Damage claimed | n (%) | 95% CI |
| Sequelae | 94 (66.20) | [57.78–73.91] |
| Death | 10 (7.04) | [3.42–12.57] |
| Sequelae in newborn | 22 (15.50) | [2.46–10.79] |
| Death of newborn | 8 (5.63) | [2.46–10.79] |
| Death of foetus | 8 (5.63) | [2.46–10.79] |
| Total | 142 (100) | |
| Grounds for breach of lex artis | ||
| Diagnostic and/or treatment malpractice | 18 (40.90) | [26.33–56.75] |
| Lack of informed consent | 9 (20.45) | [9.80–35.30] |
| Loss of chance | 8 (18.18) | [8.19–31.71] |
| Moral damage | 2 (4.54) | [0.55–15.47] |
| Diagnostic and/or treatment malpractice plus lack of informed consent | 4 (9.09) | [2.53–21.66] |
| Wrongful birth | 3 (6.81) | [1.42–18.65] |
| Total | 44 (100) | |
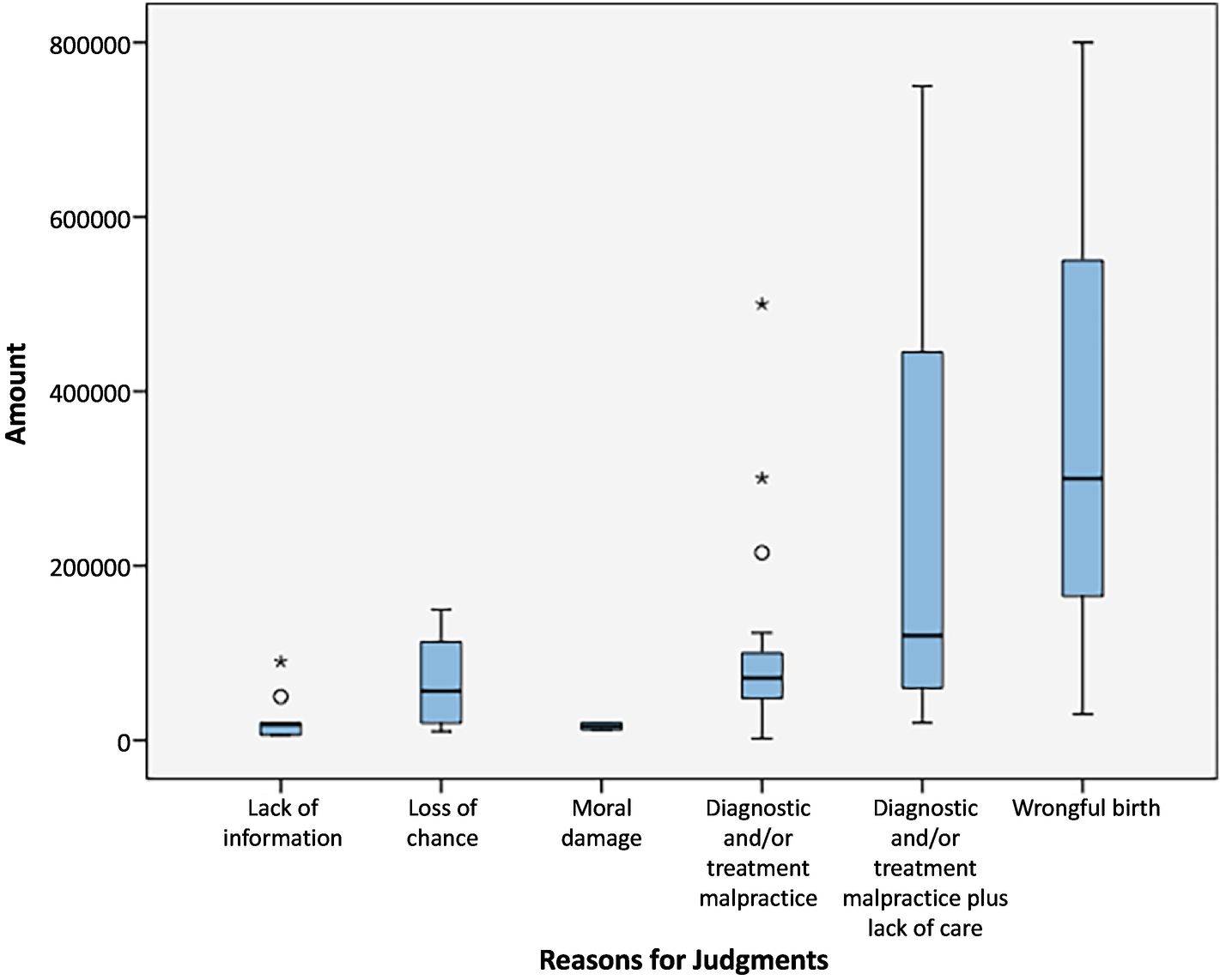
The median compensation award was 53 758.50 euros (IQR 80 885.34), with a minimum of 2000 euros and a maximum of 800 000 euros. The median number of grounds for breaches of the lex artis were; diagnostic and/or treatment malpractice 71 317.39 euros (IQR 60 521.42), loss of chance 56 500 euros (IQR 109 756.57), information deficit 18 000 euros information deficit 120 000 euros (IQR 55 750), and wrongful birth actions 300 000 euros (Fig. 2). A statistically significant difference in relation to the median was found in the grounds for the judgements (p=.024).
DiscussionThere are 3 main characteristics of claims for financial liability in the specialty of gynaecology and obstetrics: (a) they occur in non-urgent care; (b) the medical activity most involved was delivery care; (c) most are dismissed, i.e., ruled against the patient and/or relatives.
The frequency in obstetrics and gynaecology (13.99%) places it in second place among all the specialties, indicating that it is a high legal risk specialty. Although the methodology, sources, health services, and legal systems differ widely from other studies, our results are consistent with those found internationally. In all of them, the specialty of obstetrics and gynaecology is considered high-risk, making it one of the specialties against which the most claims are brought. A study in the USA found that this specialty was ranked seventh in order of frequency.8 According to a report by the UK NHS (National Health Service) (2021–2022), obstetrics ranks first in frequency and gynaecology fourth.9 In a study in the field of civil liability in Italy, the specialty came third in frequency of malpractice claims.10 In Spain, a study analysing 5426 cases in Catalonia closed between 1986 and 2005 showed that the specialty was again in second place in order of frequency of the claims analysed.11 Another study obtained the same results, although there are methodological differences with respect to our research study.12
Claims related to obstetrics, 54.22%, and gynaecology, 43.66%, obtained results that were practically the same as those obtained in a study in Spain analysing rulings on civil and administrative actions.7 In the case of medical care related to the rulings analysed in our study, the highest proportion relates to delivery care, 36.62%. Our data are consistent with those obtained in a study in Spain that analysed 885 claims in the specialty of obstetrics and gynaecology in Catalonia between 1986 and 2010. In this study, 33.1% of the claims were related to delivery care.13
The essential finding of the present research study is that 67.61% of the claims are dismissed at first instance, and, if the appellant is the patient and/or the family, 89.28% are dismissed at second instance. We found only one full ruling in favour of the patient and/or family at first instance. A study in Spain that analysed claims in the surgical area in Murcia between 2002 and 2018 found that, in the case of gynaecology and obstetrics, the outcome was in favour of the claimant in 17.7%.14 These data in favour of the administration are similar in first and second instance to those obtained in the specialties of cardiology and cardiovascular surgery (74.1%–75%)15 and emergency medicine (68.1%–64.6%)16 in the public sector in Spain. In the case of neurosurgery, the results are less favourable to the administration in the first instance (51.85%) and similar in the second instance (88.88%).17 In the USA, a study analysed claims between 1991 and 2005, and found that more than 38% of claims against obstetricians resulted in a compensation payment.8
As we can see, the vast majority of rulings are in favour of the health administration. This means that, even if a claim is brought, the outcome is largely in favour of the administration. Our results support our view that defensive medicine is a disproportionate response to the fear of litigation. Defensive medicine is a phenomenon that emerged in the USA in the late 1960s due to the insurance crisis. However, although it had a very definite origin, its use has spread throughout the world.18 The study of defensive practices is very complex, surveys among professionals are one of the most common methods used. In a UK survey involving 23.5% of obstetrics and gynaecology specialists, 78% reported some form of defensive medicine.19
In terms of compensation amounts, we highlight those relating to wrongful birth actions. These rulings have the highest median (300 000 euros), increasing the median of all compensation awards practically 6-fold. Although these rulings are the most infrequent (only 3 cases in our study), we consider it essential to make special mention of these types of ruling given their social repercussions as a whole. The practice of pre-conception or pre-birth diagnoses has resulted in society no longer seeing as a product of chance or fate the fact that people given such a diagnosis are not informed of risks or dangers for their future offspring, or that they are informed that there are none, when in fact there are, when this information is possible in accordance with the lex artis ad hoc for the specific time in question.
In such circumstances, as the future offspring is threatened by the risk of an incurable disease that could have been detected prior to conception or within the legally fixed period for terminating the pregnancy, a liability claim arises on the grounds that this lack of information has prevented the parents from taking an informed and responsible decision on whether or not to give birth to the sick child.20
The problem of professional liability has at its core a set of lawsuits in which the claimant demands compensation from the doctor for damages caused at the beginning of life in very special cases. These are the wrongful actions, first jurisprudentially recognised in Spain21–24 (STS 495/1997 of 6 June) 26 years ago.21 These cases were first raised in the 1970s in the USA, in the 1980s in the UK, and in the 1990s in France, Spain, and Germany, causing considerable legal, medical, philosophical, and ethical controversy in all these countries, in the absence of clear regulation by the legislature to provide legal certainty to this type of situation, in which negligent behaviour is found, which prevents the plaintiff from exercising a legally recognised right.
In the absence of positive regulation, this situation has been dealt with by means of 2 legal actions known as wrongful birth and wrongful life. The distinction between the 2, at least initially, is simple. A wrongful birth action is brought by the parents of the child against the doctor, alleging that, by failing to detect or to inform them of the possibility that the mother would give birth to a child with unavoidable congenital malformations or diseases, they have been deprived of the ability to make an informed decision on whether or not to give birth.25–30 In contrast, a wrongful life action is configured differently, as it is not brought by the parents, but by the child against the doctor. Its argument is that ‘but for’ the inadequate medical advice or action, the claimant would not have been born to experience the suffering inherent to their disorder.
In other words, a wrongful birth action implies that the physician's guilt lies in a mistake that led to the birth of the claimant parents' child, whereas a wrongful life action implies that the physician's error is the error that resulted in the life of the sick child, who is the claimant. The legal literature, including the medical literature, translates wrongful birth as ‘avoidable birth’, and wrongful life as ‘failed eugenics’. This is a creative translation, as it is more correct to use the literal version of both terms to speak, respectively, of ‘wrongful birth’ and ‘wrongful life’, terms that better fit the underlying problem.
The Supreme Court (STS 585/2002 of 7 June, STS 1002/2005 of 21 December) has taken a 3-fold approach to medical negligence: (a) negligence in diagnosis, the doctor makes an error in making a diagnosis in the pregnant woman and does not detect the congenital disease of the foetus; (b) negligence in information, the doctor does not inform the parents in due form or informs them belatedly, when there is no longer any possibility of resorting to a termination because the legal period has elapsed; and (c) negligence in advice, the doctor does not advise a prenatal diagnosis, when they should have.
The last requirement on which the claim for compensation is based is the damage or harm caused. In Spanish jurisprudence, the most widely accepted way of claiming wrongful birth (we have found no cases of wrongful life) is the illegitimate deprivation of the right to termination of pregnancy, which violates the sexual and reproductive rights of women. The Supreme Court (STS 969/2008 of 24 October, STS 3021/2008 of 25 May) understands that negligence of the doctor in the course of the prenatal diagnosis causes the parents to receive false or erroneous information about the condition of their future child, whom they believe to be healthy, which unjustly deprives them of the power to decide, in one way or another, on voluntary termination of the pregnancy. This deprivation, it is argued, causes the parents non-pecuniary damage per se and pecuniary damage arising from the special condition of the child's illness or disability. Indirect pecuniary damages (par ricochet, according to the courts) are also widely accepted in case law: the parents, as indirect injured parties, can be compensated for the damage caused to them psychologically and financially by the illness or disability of the child (indirect victim, since the initial victim is the mother), allowing the number of injured parties to be extended (e.g., to siblings or grandparents, who will have to prove moral damage).
The main limitation of this study is that it focuses on the legal route, since it analyses rulings in the area of the High Courts of Justice in the contentious-administrative chamber, therefore, pecuniary claims were excluded and, if applicable, those that were resolved out of court. Lastly, in this study, we do not address civil and criminal proceedings, i.e., the results obtained are limited to the public administration's liability for healthcare damages.
ConclusionsThe results of the present study indicate 3 fundamental conclusions. The first is that the specialty of obstetrics and gynaecology is one against which most claims are brought. The second conclusion is that, despite being a high-claim-risk specialty, most rulings dismiss the claims of the patient and/or family members, i.e., are in favour of the administration. The third is that most medical liability claims refer to pregnancy and childbirth, most being wrongful birth actions.
We believe that the analysis of these results can improve professionals' knowledge and understanding of certain medicolegal aspects inherent to their specialty. This knowledge could provide a scientific basis for developing novel strategies in the management and prevention of medical risks. Our findings also encourage us to initiate new lines of research, already present in other countries, to reduce the disproportionate perception of the risk of legal action. In turn, defensive medicine and its negative consequences for professionals and patients could be reduced.
FundingThis research received no specific funding from public sector agencies, commercial or non-profit organisations.
Please cite this article as: Hernández Herrero M, Tomillo Urbina J. Obstetrics and gynecology: An analysis of malpractice in the Spanish public health system. Revista Española de Medicina Legal. 2024. https://doi.org/10.1016/j.remle.2024.07.001.