Arguments of a diverse nature ranging from epidemiological to diagnostic justify the need to include the biomechanics of impact as part of the medico legal diagnosis of the cause of cervical post-traumatic syndrome (whiplash associated disorders). Biomechanical research comprises two distinct stages of forensic interest: firstly, laboratory research, using animals, corpses, and volunteers and, secondly, the study of actual collisions. This has contributed to the development of data collection devices which have helped to identify the physical parameters of an impact such as changes in velocity and acceleration in relation to the risk of whiplash injuries as well as other risk factors.
Although the literature regarding the forensic use of thresholds that define the risk of injury is not population specific, there is sufficient evidence to individualise these thresholds of risk of injury in the medico legal diagnosis of causality, although this requires further research.
Argumentos de diferente naturaleza (impacto epidemiológico, indefinición diagnóstica, ausencia de pruebas objetivas de daño) justifican la necesidad de la biomecánica del impacto en el diagnóstico médico-legal de causalidad del síndrome postraumático cervical (whiplash associated dissorders) en terminología anglosajona. Su investigación biomecánica tiene dos etapas bien definidas de interés médico-legal: la investigación en laboratorio (animales, cadáveres, y fundamentalmente voluntarios) y el estudio de colisiones reales, a lo que ha contribuido el desarrollo de dispositivos de recogida de datos. Esta investigación ha permitido identificar parámetros físicos de la colisión (cambio de velocidad, aceleración) relacionados con el riesgo de lesiones cervicales, así como otros factores de riesgo. Aunque la utilización médico-legal de los umbrales que delimitan el riesgo de lesión poblacional no es pacífica en la literatura, existen suficientes evidencias que permiten individualizar estos umbrales de riesgo de lesión en el diagnóstico médico-legal de la causalidad, si bien exige un profundo conocimiento.
Injury or impact biomechanics studies the impact of stress (forces, moments, etc.) on biological material, focusing on damaged tissues.1 Knowledge of engineering, physics, and related sciences help us identify the necessary magnitude, direction, and duration of forces sufficient to exceed the tolerance level of the biological systems.2 Forensic Biomechanics arises from this discipline, applied to the field of Legal and Forensic Medicine, which shows its greatest validity when it explains how an injury occurs and, to a lesser extent, when it is used to refute the cause of an injury.
The new reform of the Sistema de Valoración de Daños Personales en Accidentes de Circulación [Traffic Accident Personal Injury Assessment System] will introduce, among other modifications, the need to evaluate mild spinal injuries using the causation criteria of intensity, within the field of Forensic Biomechanics, without overlooking the fact that it is immersed in a dialog of causation that cannot be ignored. It is not advisable, save for some exceptions, to reduce diagnoses of causation to a dividing line set at an ideal threshold, which would likely give rise to the model itself losing validity, as has happened in other countries. The threshold that marks the risk of injury will function as a guideline. It is also impossible to dispense with a new field of knowledge that is completely scientifically valid, merely because it is new.3,4
Post-traumatic cervical syndrome (PTCS), despite being a mild injury, is characterised by a paradoxically complex diagnosis. Structural injuries have only been able to be observed at the interapophyseal joint level, despite the fact that other possibilities have been postulated5,6 (injuries to discs, spinal ligaments, nerve structures, muscles, vertebral artery, etc.). This ignorance of the pathophysiological background involves the absence of objective tests of injury with the available diagnostic methods, basing the diagnosis on patient symptoms. This is a pathology that tends to occur more often than it is diagnosed.7
This is added to the fact that, firstly, the symptoms are common to multiple highly prevalent pathologies, with cervical pain being one of the leading causes of consultation in western societies. Secondly, the usual exploratory signs (stiffness, limited mobility, trigger points, muscle tone, etc.) do not exceed statistical interobserver consistency tests.8–11
This lack of objectivity of the usual exploratory signs has led to the proposal to modify Haldeman's classic Quebec classifications.12
Finally, it is also important to note that the epidemiological figures of PTCS are influenced by socioeconomic factors,13 and are closely linked to the medico-legal concept of injury simulation (pure simulation, exaggeration, pretext, etc.). Capilla et al.14 recently conducted a study in which more than 100 primary care physicians participated. Sixty percent of them considered that the primary cause of simulation in their usual patients was PTCS. In our specific case, out of some 2000 patients examined in the past few years, approximately 40% had experienced more than one accident with this diagnosis, and more than half had suffered at least two accidents with identical injuries, even cases with more than 4 episodes.
All of the above circumstances constitute a challenge to the medico-legal expert. A wide knowledge is needed to analyse each and every one of the elements that support the causality, organising their validity in order of importance in each case so we may observe that there is no single deterministic causality, irrefutable proof of injury. In this context it becomes necessary to introduce the criterion of intensity in the study of causation, evaluating the risk of injury based on biomechanical knowledge of collisions,5–19 constituting one of the major criteria of causality.18
Evolution of the biomechanics of impact in the study of cervical injuriesInjury criteria and thresholds are studied, to be used to improve the safety of vehicles and their components. The threshold of injury tolerance which establishes the risk of injury is permanently reviewed through epidemiological studies.20,21 Research on the biomechanics of impact in cervical injuries does not have its own medico-legal profession.
In the second half of the last century, research was based on experimentation with animals, corpses, dummies, and primarily volunteers subjected to typical in-line vehicle-vehicle collisions. The United States and Canada led the research in this first phase. Since 2000, the research has focused on the analysis of real collisions, especially since the development of black box-type devices incorporated into vehicles (Event Data Recorder [EDR] and Crash Pulse Recorder [CPR]). This second phase is being led by Europe, and in particular Germany and Sweden.
The biomechanics of impact focuses on three issues:
- •
Understanding the mechanisms of injury and onset of symptoms. Experimentation with volunteers in laboratory crash sleds with cineradiography has been very useful in this regard. Through these studies, the previous idea of the injury-type mechanism (hyperextension-flexion) has been discarded in favor of a more complex model in which the forces of compression (thoracic ramping) and shearing, associated with extension-flexion and cervical rotation, come to the forefront. This would explain, for example, injuries in the interapophyseal joints.
- •
Clarifying the collision parameter that relates to the accident's injury potential and identifying the population/human safety threshold for this parameter that can be used to improve the safety of vehicles and their components (bumpers, seats, headrests, etc.). Research on real collisions, especially on vehicles with EDR or CPR devices has been very useful in this regard.
- •
Improving safety. Two elements have been identified as essential in preventing the risk of cervical injuries: the seat and the headrest. These have reduced permanent disability arising from cervical injuries by up to 11% annually between 1998 and 2012 and reduced by 6.5% the duration of symptoms over one month within the same period.22
Various injury criteria and other parameters, such as expression of the energy of the collision have been proposed. Most injury criteria are intended for laboratory tests (seat and dummy standardisation, validity of numerical models, etc.), thus making it very difficult, if not impossible, to apply them practically.20 The most well-known are the Neck Injury Criterion and the Intervertebral Neck Injury Criterion.
Today the magnitude of a collision that can cause damage to the soft tissues of the neck is expressed in terms of change in speed and acceleration.23 The most used physical parameter is Δv (Δv), considered the indicator of a collision's magnitude in the absence of intrusion into the passenger compartment.24 It represents the change in speed of a vehicle's center of gravity/mass during the time that it is in direct contact with another vehicle during the collision, which is approximately 100ms15,25 in most collisions. Experts in accident reconstruction (engineers) calculate this based on the damage suffered by the vehicles (photographs, witnesses, accident records, collision drawings, expert reports, repair invoices, etc.), commonly using the momentum-energy-restitution method.26 Laboratory tests of similar vehicles are used as comparative models,15 linearly relating the mean acceleration and peak acceleration with the collision speed,19 although it is considered that comparative test studies with the calculations made may have a margin of error of between 4% and 9%.26 Although this is the most common way to calculate it, using EDR or CPR is more precise, because these directly measure and record the acceleration pulses experienced by the vehicles in which they are mounted. Experts affirm that conventional reconstruction methods are not useful, especially computer programs designed for the study of plastic collisions (with visible damage) that are usually high energy.27
The value Δv (Δv) has been used to define the concept of low speed rear-end collisions, corresponding to those in which Δv is less than 8–15km/h20,26 (according to the authors). In research, collisions with Δv less than 16km/h are considered low impact, between 16 and 24km/h are considered medium impact, and above 24km/h are considered high impact.28
The change in speed necessarily implies acceleration. Also, during the speed change period (Δv), acceleration is not uniform, with a distinguishable peak in acceleration and a mean acceleration. Mean acceleration corresponds to the mean acceleration value during the collision pulse, which is the time that elapses until the acceleration changes from positive to negative values, reaching 90% of Δv. Another relevant finding is that mean acceleration is not always the same for a particular Δv, and it is not possible to identify a typical mean acceleration for a known Δv, whether in the laboratory or in real life.23,29 Even collision pulses are different for the same vehicle and the same Δv, giving rise to different mean acceleration values. The shorter the collision pulse for a same Δv, the greater the mean acceleration. Therefore, the shape of the collision pulse will be important in the assessment of the risk of cervical injuries.
The latest research studies, which use data from real collisions, have shown that mean acceleration is a better predictor for the risk of injury, the severity of the injury, and the duration of symptoms.16,26,30 In research, collisions with mean acceleration below 4.5g are considered low impact, 5.5g medium impact, and above 6.5g high impact.28
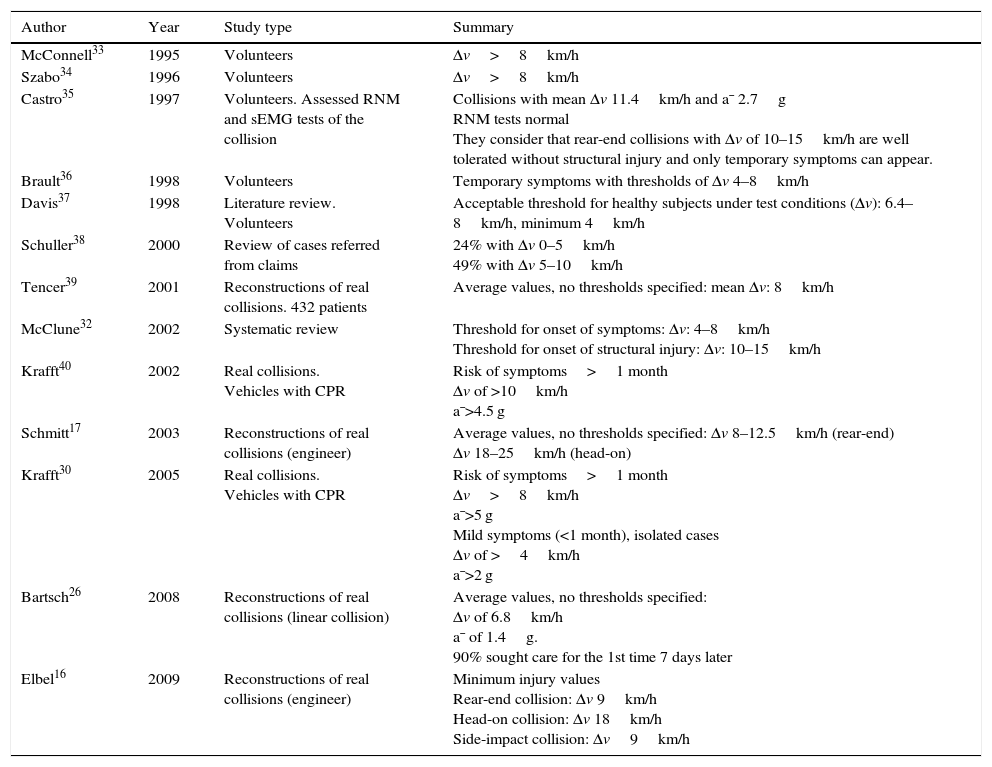
The greatest risk of cervical injuries occurs with Δv values between 9 and 20km/h. Three-quarters of cases occur with Δv less than 15km/h and only 7% with Δv higher than 25km/h.31 It has also been postulated that the threshold for the onset of symptoms is between 4 and 8km/h, while the threshold for causing structural injuries and tissue damage is 10–15km/h.20,17,32 It may be illuminating to list some of the thresholds considered to cause injury by different researchers (Table 1), referencing the research methodology (volunteers, real collisions, etc.).
Summary of injury thresholds by different researchers, taking into account the study type.
| Author | Year | Study type | Summary |
|---|---|---|---|
| McConnell33 | 1995 | Volunteers | Δv>8km/h |
| Szabo34 | 1996 | Volunteers | Δv>8km/h |
| Castro35 | 1997 | Volunteers. Assessed RNM and sEMG tests of the collision | Collisions with mean Δv 11.4km/h and a¯ 2.7g RNM tests normal They consider that rear-end collisions with Δv of 10–15km/h are well tolerated without structural injury and only temporary symptoms can appear. |
| Brault36 | 1998 | Volunteers | Temporary symptoms with thresholds of Δv 4–8km/h |
| Davis37 | 1998 | Literature review. Volunteers | Acceptable threshold for healthy subjects under test conditions (Δv): 6.4–8km/h, minimum 4km/h |
| Schuller38 | 2000 | Review of cases referred from claims | 24% with Δv 0–5km/h 49% with Δv 5–10km/h |
| Tencer39 | 2001 | Reconstructions of real collisions. 432 patients | Average values, no thresholds specified: mean Δv: 8km/h |
| McClune32 | 2002 | Systematic review | Threshold for onset of symptoms: Δv: 4–8km/h Threshold for onset of structural injury: Δv: 10–15km/h |
| Krafft40 | 2002 | Real collisions. Vehicles with CPR | Risk of symptoms>1 month Δv of >10km/h a¯>4.5 g |
| Schmitt17 | 2003 | Reconstructions of real collisions (engineer) | Average values, no thresholds specified: Δv 8–12.5km/h (rear-end) Δv 18–25km/h (head-on) |
| Krafft30 | 2005 | Real collisions. Vehicles with CPR | Risk of symptoms>1 month Δv>8km/h a¯>5 g Mild symptoms (<1 month), isolated cases Δv of >4km/h a¯>2 g |
| Bartsch26 | 2008 | Reconstructions of real collisions (linear collision) | Average values, no thresholds specified: Δv of 6.8km/h a¯ of 1.4g. 90% sought care for the 1st time 7 days later |
| Elbel16 | 2009 | Reconstructions of real collisions (engineer) | Minimum injury values Rear-end collision: Δv 9km/h Head-on collision: Δv 18km/h Side-impact collision: Δv9km/h |
We note that thresholds for the onset of symptoms are lower in real collisions, which could be related to the multiple factors related to the risk of injury, many of them not present in laboratory testing with volunteers and that reflect the multitude of conditions that occur in the real world (attention, position, predisposing physiological and psychological factors, etc.). Another possible influencing factor, not addressed in any of the studies in real collisions, is that all the subjective diagnoses have been considered valid, despite being cases in the context of the insurer and in some cases susceptible to simulation (pure, exaggeration, pretext, allegation).
There is no doubt (extensive scientific evidence) about the relationship between Δv and the injury potential of a collision in general terms.24,41 Given this general principle, and with regard to low-speed collisions, we have noted in the research in real collisions that there is no linear correlation between Δv and/or mean acceleration and the severity and prognosis of the injury.6,12,16,17,22,26,30,42 However with low Δv values, in most cases, there were no symptoms or these were very mild and temporary. It is very important to distinguish between the Δv threshold and/or mean acceleration for the risk of injury, the severity of the injury and duration of symptoms.43
The Δv and/or mean acceleration are not very reliable as predictors of the severity and prognosis of cervical injuries. Nevertheless, they have been shown to be good predictors with high sensitivity and specificity when their values return low or very low results. Elbel establishes that for all collision types (rear-end, front, side-impact, rollover) it is impossible to set a Δv value that precludes the occurrence of cervical injuries with acceptable sensitivity, while simultaneously predicting the occurrence of injuries with acceptable specificity.16 It returns sensitivity and specificity criteria that only yield absolute results (0% and/or 100%) with very low (4km/h) Δv values.
We recommend mean acceleration as a medico-legal criterion of intensity, given that algorithms are already available to calculate these by comparison with results from low-speed collision test databases. Nevertheless, in the case of vehicles equipped with data collection devices (EDR, CPR or similar), it would be preferable to use all information recorded about the acceleration pulse (duration of the collision, mean vehicle acceleration and peak acceleration reached). Modern EDR and CPR devices detect maximum acceleration values of about 2g, that is, they record acceleration pulses with very low mean acceleration, lower than 2g. However, we continue to maintain Δv as a reference given its accessibility and its acceptable validity in very low-speed collisions.
In biomechanic expert analysis, in addition to the reference Δv value, we must expand the information to some collision factors that may be equally relevant (direction, type of vehicle, seat, headrest, among others), and we should identify the criteria taken into account in the engineering report (methodology, sources of information, starting study data, etc.), obviously without going into technical considerations, since, as Kieser44 reminds us: in the face of complex mathematical formulas, medical experts suffer an attention disorder.
Factors associated with the risk of injuryThe validity of these two physical parameters in the medico-legal practice is not the only topic of discussion. Issues regarding the methodology and information used for calculating them are also commonly discussed, as well as other questions such as the difference between the vehicle and occupant thresholds, the age of the vehicles, the importance of the safety equipment, passenger position, or direction of the collision, etc.
Freeman reminds us of the initial difficulty of estimating risk of injury in modern vehicles, as it may seem at first sight that there is no material damage due to the elasticity of modern bumper materials45 (except when performing an inspection with dismantling of the vehicle) even with Δv values of 13km/h. Conversely, there may be visible damage which corresponds to very low values of the injury risk parameters, making it necessary to regulate the sources of information that must be taken into account during accident reconstruction. On the other hand, this validates Walz and Muser's recommendations that doctors should not interpret car damage in relation to the potential harm. This suggests that clinicians should not offer opinions on the accident speed or impact energy without sufficient biomechanical training.46
The difference in the change in speed and acceleration values between the vehicle and the occupant often generates considerable concern. Gabauer and Gabler compare Δv and the occupant impact speed using EDR.47 This is based on Michie's Flail Space Model, which assumes that a vehicle's occupant is a single unstable mass in its interior with randomised 0.6m longitudinal and/or 0.3m transversal displacement. This is used to calculate the difference in speed between the occupant and the passenger compartment when reaching a 0.6m longitudinal and 0.3m lateral displacement. This model assumes that the severity of an occupant's injuries is related to the speed with which he/she impacts against the vehicle's interior and/or with the acceleration forces generated. They conclude (only in head-on collisions) that the occupant's impact speed does not offer a predictive advantage with regard to Δv.
Freeman establishes the correlation between the acceleration values (peak acceleration) of the vehicle and of the head, where with very low to low Δv values (4.8–8km/h), the peak acceleration of the head is lower than that of the vehicle.45 Howard et al.2 agree that for low Δv values (<10km/h) values and acceleration lower than 4–6g, the head/vehicle acceleration ratio tends toward 1:1, compared to the ratio for collisions with greater Δv values, the ratio for which is 2.5:1. Similar conclusions were recently proposed by Hoyes and Henderson.41 It is important to note that this argument loses validity as the collision becomes more atypical.
We also question whether position in the vehicle, use of seatbelt, twisting of the neck, or angle relative to the back rest should be taken into account. No information is available concerning most of these variables (neck turned, trunk inclined, etc.) in real collisions, although presumably any circumstances could have existed. However, various studies have been conducted with volunteers sitting in different positions, with the neck turned, inclining, etc., with Δv values from 2.5 to 8km/h. The work by Keifer et al. in 200548 is the most recent and complete. They cause aligned rear-end collisions with mean Δv of 7.67 and volunteers sitting in four different positions (normal, torso inclined 10°, head bent 20°, and torso inclined 10° with head bent 20°). They compare acceleration in each of the different positions and note that the acceleration of the head is similar in the normal position and with bent head, while it appears slower and reduced with the torso inclined. Chest acceleration is higher than that observed in the vehicle's center of gravity. The symptoms were variable, affecting the head-scapular girdle complex and lasting from hours to a few days, except in one case in which they lasted less than a month.
In recent years the back-headrest combination has been considered the element that most influences the prevention of cervical injuries in low-speed collisions. Vehicles equipped with anti-whiplash devices significantly reduce the risk of injury,22,31,49–51 up to between 20% and 50% in rear-end and side-impact collisions. As already mentioned, research in this field has enabled the development of headrests and seats that have reduced permanent disabilities derived from cervical injuries by up to 11% annually between 1998 and 2012, and reduced the duration of symptoms longer than one month by 6.5% in the same period.22
Other factors that must be taken into account are what is known as physiological and psychological risk,6 without disregarding the medico-legal context.52,53 Being a woman and psychological predisposition have been shown to be the most relevant risk factors, unanimously accepted throughout the scientific literature. The risk of injury is generally double in women and psychological predisposition is even capable of causing cervical pain symptoms in placebo collisions.35
The comparison between head acceleration values in low-speed collisions and some daily life situations (such as sneezing or dropping into an armchair) is often brought into the medico-legal discussion, trying to minimise an accident's injury potential. Nordhoff attempts to undermine the validity of this comparison, alluding to the protection offered by learning mechanisms and/or evolutionary memorisation of these common situations and affirming that there is no scientific evidence that humans have adapted during evolution to traffic accidents.54 Nonetheless, Hoyes and Henderson compare three collisions with different Δv values with three daily life activities (sitting in different types of seats), observing that with low Δv values (<3mph), chest and head accelerations are similar in collisions and the proposed activities.41
In summary, we can identify different types of variables that are associated with a higher risk of, or protection from, cervical injuries in low-speed collisions. While sex and seat-head rest geometry differences seem consistent, other variables studied show uncertain behavior such as position in the seat, the relative difference between vehicle/occupant acceleration, or position in the vehicle. However, we can observe that in very low-speed collisions (Δv around 6km/h), some of the most commonly discussed questions are irrelevant (such as position of the neck/chest before the collision or vehicle/head acceleration). Other pathological, physiological and/or psychological variables that will influence the prognosis are not taken into account in research studies, designed to increase the safety of vehicles in the general population.
Medico-legal application of injury thresholds. CausalityWhile the specialised literature on the biomechanics of impact on cervical spine injuries is uncontroversial, it becomes very controversial when we attempt to extrapolate the results to the insurance and legal fields in order to reject claims due cervical injuries in low-speed collisions. Here is when geographical contextualisation becomes necessary to understand the majority of “scientific” production in this area.
From the mid-1990s, an insurance practice became widespread in the US consisting of, as a general rule, considering claims for personal injuries to be fraudulent when the structural damage to the vehicle was less than US$1000. This practice is known as minor impact soft tissue and is still current today. Numerous American medical experts have written about the lack of relationship between the concept of minimal damage and the risk of cervical injury, understanding this concept in the US context of minimal damage (structural damage to the vehicle less than US$1000). Freeman and Croft are notable among these experts.
In the same context (USA), in recent years this situation has given rise to the spontaneous creation of an industry around legal biomechanics in low-speed collisions.25 However, biomechanical reports in low-speed collisions have progressively lost prominence in legal proceedings, due to the system of assessing evidence in civil proceedings (Daubert Standard), partly due to experts’ inability to calculate potential error,4,25 a necessary requirement in this standard for assessment of expert evidence.
There are few publications about the use of injury thresholds in low-speed collisions in the medico-legal context.6,13,18 It is a relatively recent field and in a very specialised context, under-represented in leading publications or those with higher impact indexes and with little penetration among medical experts in Forensic Medicine and/or with medico-legal expertise. Limited knowledge of this field also applies to experts in accident reconstruction. With the intensity criteria in the study of causation of mild spinal injuries being inserted into the legal context, it would be advisable to set a quality standard for accident reconstruction reports and forensic biomechanical reports. Although there is a natural polarisation of opinion in the judicial context, the rigor imposed in the methodology of biomechanical studies should be sufficient for efficient development of this discipline as a real aid to the justice system. Among other issues, the debate should be resolved with each of the experts involved (doctor and engineer) being limited to the domain of their expertise. The engineer should provide the physical data (Δv, mean acceleration (preferably), peak acceleration, collision pulse, collision direction, vehicle type, specific characteristics of the security elements: seat, headrest, etc.), while the physician should insert this data into the discussion of causality, along with other causation criteria.
Freeman reminds us that analysis of the risk of injury is not equivalent to the diagnosis of simulation.4 We must bear in mind the medico-legal context. This means that it is not about questioning the reality of the patient's clinical symptoms, unless an irrefutable diagnosis of simulation is made. The problem is that the patient's nonspecific symptoms or the diagnosis of post-traumatic cervical syndrome by an emergency or outpatient care professional are insufficient for medico-legal diagnosis of causality. The medico-legal diagnosis is more complex in cases in which an organic cause of pain is not identified (such as an interapophyseal injury, etc.) or the symptoms are not accompanied by any pseudo-objective manifestation (loss of mobility, loss of muscle tone, etc.).
By adding the intensity criteria to prove the causality of a spinal injury, we must first define whether intensity must be expressed qualitatively (causation qualifiers) or quantitatively (statistical variables to measure strength of association). A mixed model, similar to the one proposed by Freeman,4 would be ideal. The problem is that we do not have epidemiological studies to insert the necessary variables into the formulas for calculating association. It would be advisable to create databases similar to those available in other countries, although these also do not collect sufficient data on low-speed collisions.26
Secondly, it would be advisable to know the injury thresholds for the onset of symptoms, the risk of structural injuries, and the severity of the injury. In an ideal model, we would need to set a threshold for each sex, morphotype, psychological profile, type of seat, headrest, etc.: an individualised threshold. This does not invalidate the use of current knowledge in impact biomechanics, using the thresholds that have been called populational/human type, taking as a reference the lowest values at which no injuries have been confirmed (research with human volunteers and real collisions) or, at most, isolated cases of passing symptoms have occurred. As was justified previously, both Δv and mean acceleration (a¯) can be used, while knowing that a¯ is a better predictor, and so when both are available, a¯ is more valid. The more information (and the more supported information) that the reconstruction report can offer (Δv, a¯, peak acceleration, collision pulse shape, the vehicle's anti-whiplash equipment, etc.), the higher the diagnostic sensitivity of causality will be in the forensic biomechanical report.
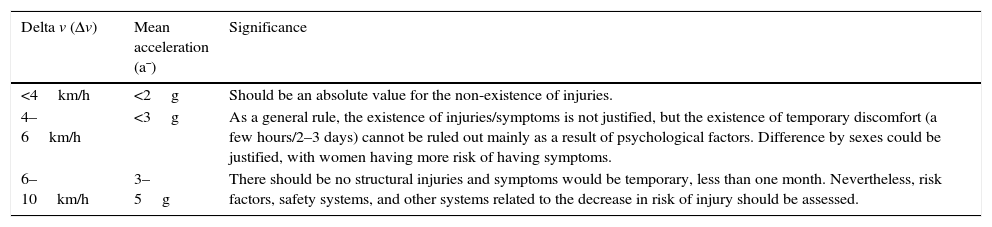
In summary, we propose the following values as a reference in the study of causality, for the case of cervical injuries in rear-end collisions, modified from Represas and Luna,18Table 2.
Recommended thresholds for the intensity criteria in the study of the medico-legal causality of PTCS.
| Delta v (Δv) | Mean acceleration (a¯) | Significance |
|---|---|---|
| <4km/h | <2g | Should be an absolute value for the non-existence of injuries. |
| 4–6km/h | <3g | As a general rule, the existence of injuries/symptoms is not justified, but the existence of temporary discomfort (a few hours/2–3 days) cannot be ruled out mainly as a result of psychological factors. Difference by sexes could be justified, with women having more risk of having symptoms. |
| 6–10km/h | 3–5g | There should be no structural injuries and symptoms would be temporary, less than one month. Nevertheless, risk factors, safety systems, and other systems related to the decrease in risk of injury should be assessed. |
For pure side-impact collisions there is no consensus on injury thresholds and, although significantly greater values have been postulated than for rear-end collisions, studies in real collisions have shown values closer to the latter.16 For head-on collisions, the thresholds may be even double those for rear-end collisions.16,30,55 The proposed thresholds correspond to collisions that are technically more harmful: those that generate linear accelerations (linear collisions). There are many variants in real life that must be studied, especially angular collisions that create rotational acceleration, with lower injury potential than those that generate linear acceleration in a low-speed context, and that are so common in daily life, especially angular collisions at low speeds in roundabouts.
ConclusionWe recommend using Δv (delta v) and a¯ (mean acceleration) as intensity criteria in the study of the medico-legal causality of post-traumatic cervical syndrome, keeping in mind, however, that a¯ is more sensitive. Although these two are not good predictors of the severity and prognosis of the pathology, they are good indicators of the likelihood of injury or onset of symptoms, with high specificity in very low-speed collisions.
Conflict of interestThe authors declare no conflict of interest.
Please cite this article as: Represas Vázquez C, Muñoz Barús JI, Luna Maldonado A. Importancia de la biomecánica del impacto en la valoración pericial del síndrome del latigazo cervical. Rev Esp Med Legal. 2016;42:72–80.