To analyze a sample of pregnant patients who underwent pulmonary perfusion scintigraphy to rule out suspicion of pulmonary embolism (PE) during the acute COVID-19 infection hospitalization period in our hospital.
Material and methodsSPECT scintigraphy with a reduced dose (111MBq) of 99mTc-macroaggregated albumin was performed in all the patients (n=5). The images obtained were interpreted by comparing the findings with the radiological images according to the PISAPED criteria.
ResultsOnly one of the 5 patients was diagnosed with PE. Two patients showed pathological scintigraphy findings attributable to radiological alterations due to COVID-19 pneumonia, and the other two had normal pulmonary perfusion.
ConclusionGiven the non-specific features of the clinical manifestations and d-dimer values in COVID-19, as well as their similarity to those of PE, pulmonary perfusion scintigraphy plays a crucial role in the screening of PE in these patients due to its high sensitivity and lower irradiation compared to CT. Despite the limited number of patients, the results obtained have special relevance due to the absence of scientific publications in this group of patients within the exceptional context of the COVID-19 pandemic.
Analizar la muestra de pacientes embarazadas a las que se le realizó una gammagrafía de perfusión pulmonar para descartar la sospecha de tromboembolismo pulmonar (TEP) durante el ingreso en nuestro centro por infección aguda por COVID-19.
Material y métodosA todas las pacientes (n=5) se les realizó una gammagrafía SPECT con dosis reducida (111MBq) de 99mTc-macroagregados de albúmina. Las imágenes obtenidas se interpretaron comparando los hallazgos con la imagen radiológica según criterios PISAPED.
ResultadosDe las 5 pacientes, tan sólo en una se diagnosticó TEP. En dos pacientes los hallazgos patológicos de la gammagrafía fueron atribuibles a alteraciones radiológicas por neumonía COVID-19, y otras dos mostraron una perfusión pulmonar normal.
ConclusiónDado lo inespecífico de las manifestaciones clínicas y valores del dímero-D dentro de la COVID-19, así como su similitud con los de TEP, la gammagrafía de perfusión pulmonar, por su alta sensibilidad y menor irradiación que la TC, tiene un papel crucial en el despistaje de TEP en estas pacientes. Los resultados obtenidos son de especial relevancia, a pesar del número limitado de pacientes, dada la ausencia de publicaciones científicas en este grupo de pacientes dentro de la situación excepcional por la pandemia COVID-19.
Approximately one year after the onset of the SARS-CoV-2 pandemic (January 2020, Wuhan, China), in December 2021, the Pfizer–BioNTech mRNA BNT162b2 and the Moderna mRNA-1273 vaccines were authorized by the Food and Drug Administration1 for use in the general population. Nonetheless, at this time no recommendations were initially given to support or rule out their use in pregnant women, leaving the decision to the criteria of the attending physician. This led to a marked delay in the vaccination of pregnant women, translating into more than 29,000 pregnant women being hospitalized due to COVID-19 infection and the death of 2742. It was not until July 2021 that the (American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) actively encouraged pregnant women to be vaccinated3 following the publication of the first safety results in studies on vaccines in the real population4.
Since the beginning of the pandemic, there has been wide variability in the symptoms and diseases associated with the classical clinical picture of airway involvement (fever, cough, dyspnea, among others), which is predominant in this infection. Among the associated phenomena, of note are venous thromboembolisms (VTE), with pulmonary embolism (PE) being of special relevance due to its high frequency. The physiopathogenesis of these phenomena lies in excessive immune activation of the infection, producing the release of different inflammatory mediators to the blood (cytokines and others) that activate platelets, neutrophils and endothelial cells. This state of hypercoagulability, dysfunction and increase in endothelial permeability favors thrombosis, analytically translating into an elevation of d-dimer and fibronogen5,6.
The hemostatic, hormonal and venous ectasia associated with pregnancy produces a greater predisposition of pregnant women to present VTE compared to non-pregnant women. Moreover, the addition of the period of reduced mobility due to confinement during the pandemic, led to pregnant women being especially taken into account as a group of risk for VTE within COVID-19 infection.
Scintigraphy plays a key role for ruling out the presence of pulmonary thromboembolism (PTE) in patients with severe respiratory insufficiency, respiratory distress or tachypnea within the context of SARS-CoV-2 infection. The main advantages of scintigraphy over computerized tomography (CT) angiography are its high diagnostic sensitivity (100% vs. 83% respectively7) and less irradiation to the patient (effective estimated dose to the mother of 1.62 mSv with a scintigraphy with 111MBq of 99mTc-macroaggregate albumin or 99mTc-MAA vs. 28.39±2.61 with CT)8,9. In regard to the acquisition protocol, single photon emission computed tomography (SPECT) has been described as superior to planar images (sensitivity and specificity of 100% and 87% vs. 64% and 72%, respectively)10–12.
We analyzed a sample of pregnant women who underwent pulmonary perfusion scintigraphy to rule out the suspicion of PTE during admission to our center (Hospital Universitario Juan Ramón Jiménez, Huelva, Spain) for acute COVID-19 infection. It is important to note that at the beginning of the pandemic we adapted our pulmonary SPECT protocol according to the recommendation13,14 of removing the ventilation component due to the risk of contagion and contamination by SARS-CoV-2, and therefore, we performed perfusion scintigraphy in a SPECT/CT modality. In the case of pregnant women, the CT component was also withdrawn.
Material and methodsFollowing the administration of 99mTc-MAA with a reduced dose (111MBq, estimated effective dose 1.62mSv) pulmonary perfusion SPECT (Symbia Intevo gamma camera) was performed. The images obtained were processed obtaining axial, coronal and sagittal slices. For interpretation, the PISAPED protocol15 was followed, which takes into account the morphology and segmentary/non segmentary distribution of the perfusion defects as well as their correspondence with alterations of the thoracic radiography image. These criteria define one or multiple defects with a characteristic wedge morphology without concordant anomalies in the chest radiography as a defect compatible with PTE, while defects not presenting this morphology and which are less than or equal in extension to the radiological findings are defined as non-compatible with PTE.
We describe a sample of 5 (age 29±7 years) pregnant patients of 28.4±2.7 weeks of gestation who were admitted to our center for clinical manifestations of dyspnea New York Heart Association (NYHA) III (1/5) and IV (4/5) during acute COVID-19 infection of 4.6±3.3 days of evolution. None of the patients had received a previous vaccination dose against SARS-CoV-2. In view of the disproportionate increase in dyspnea during admission, also associated with tachypnea in 2 patients, pulmonary perfusion scintigraphy was requested to rule out pulmonary thromboembolic disease.
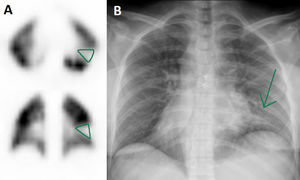
ResultsFor better understanding and correlation, the scintigraphic results visualized are shown in Table 1 together with the gestational status, pulmonary auscultation, d-dimer levels, and chest radiography findings as well as their interpretation according to the PISAPED criteria. At the time of the study, all the patients were receiving anticoagulant prophylaxis.
Results and characteristics of the patients included.
| Gestation (weeks) | Pulmonary auscultation | D-dimer (ng/mL) | Chest radiography | Pulmonary perfusion SPECT | PISAPED | |
|---|---|---|---|---|---|---|
| Patient 1 | 27 | Normal | 3150 | Normal | No perfusion defects | Normal |
| Patient 2 | 32 | Normal | 2339 | Minimum increase of the interstitial tissue in the right lung base | No perfusion defects | Normal |
| Patient 3 | 30 | Crackling in right base | 1874 | Infiltrate in pulmonary bases | Defect in lower segment of the lingula coinciding with area of pneumonia | Abnormal not compatible with PTE |
| Patient 4 | 28 | Vesicular murmur reduced in bases and disperse rhoncus (mechanical intubation) | 3801 | Infiltrate in left pulmonary base | Sub-segmentary defect in upper segment of the LLL coinciding with radiological infiltrate | Abnormal not compatible with PTE |
| Patient 5 | 25 | Minimal sub-crackling in right base | 6664 | Normal | Sub-segmentary defects in upper segment of the LRL and LLL with triangular morphology with pleural base | Abnormal compatible with PTE |
LLL: lower left lobe; PTE: pulmonary thromboembolism.
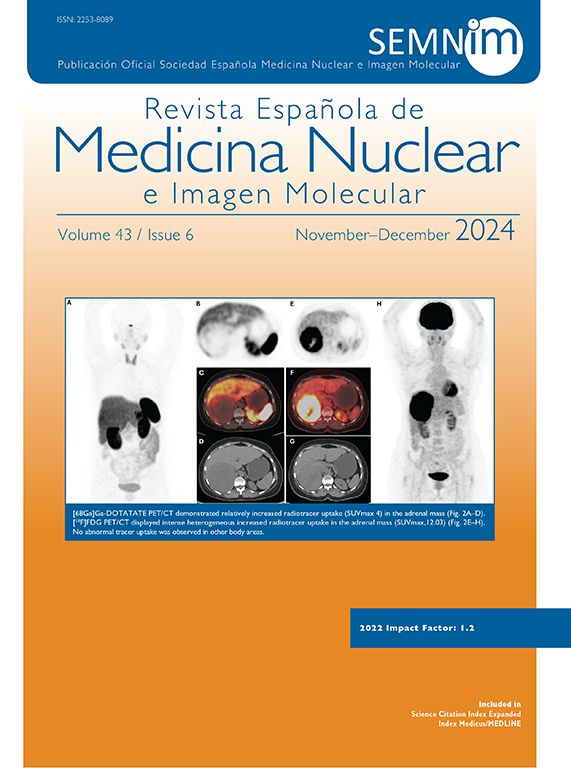
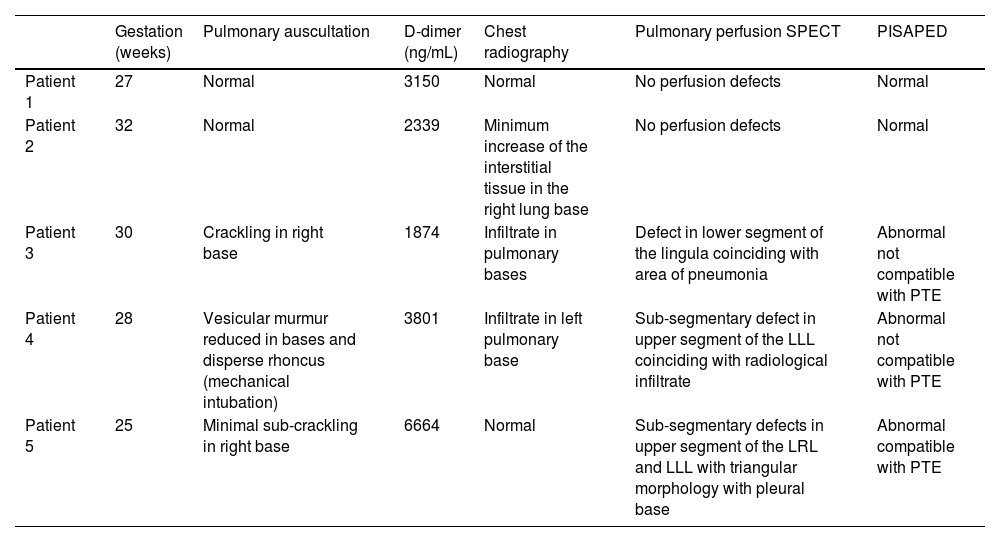
The images were pathologic in 3 of the 5 patients, being compatible with PET in only one patient, localizing sub-segmentary perfusion defects in the upper left segment of both the lower left (LLL) and right lobes (LRL) (Fig. 1). This patient was discharged with anticoagulant treatment and close follow-up due to having a pregnancy at risk and finally delivered at term without complications.
Pulmonary perfusion SPECT performed in patient 5 showing sub-segmentary perfusion defects in the upper segments of the LLL (A, blue, in coronal and sagittal slices) and LRL (red, in axial and coronal slices), with no correspondence with condensations in the radiological images to justify these findings (B), being compatible with PTE. In addition, a defect of linear horizontal uptake (green arrow) can be seen that continues in the cranial SPECT slices in the posterior direction, radiological corresponding with minimal thickening of the minor fissure (green circle).
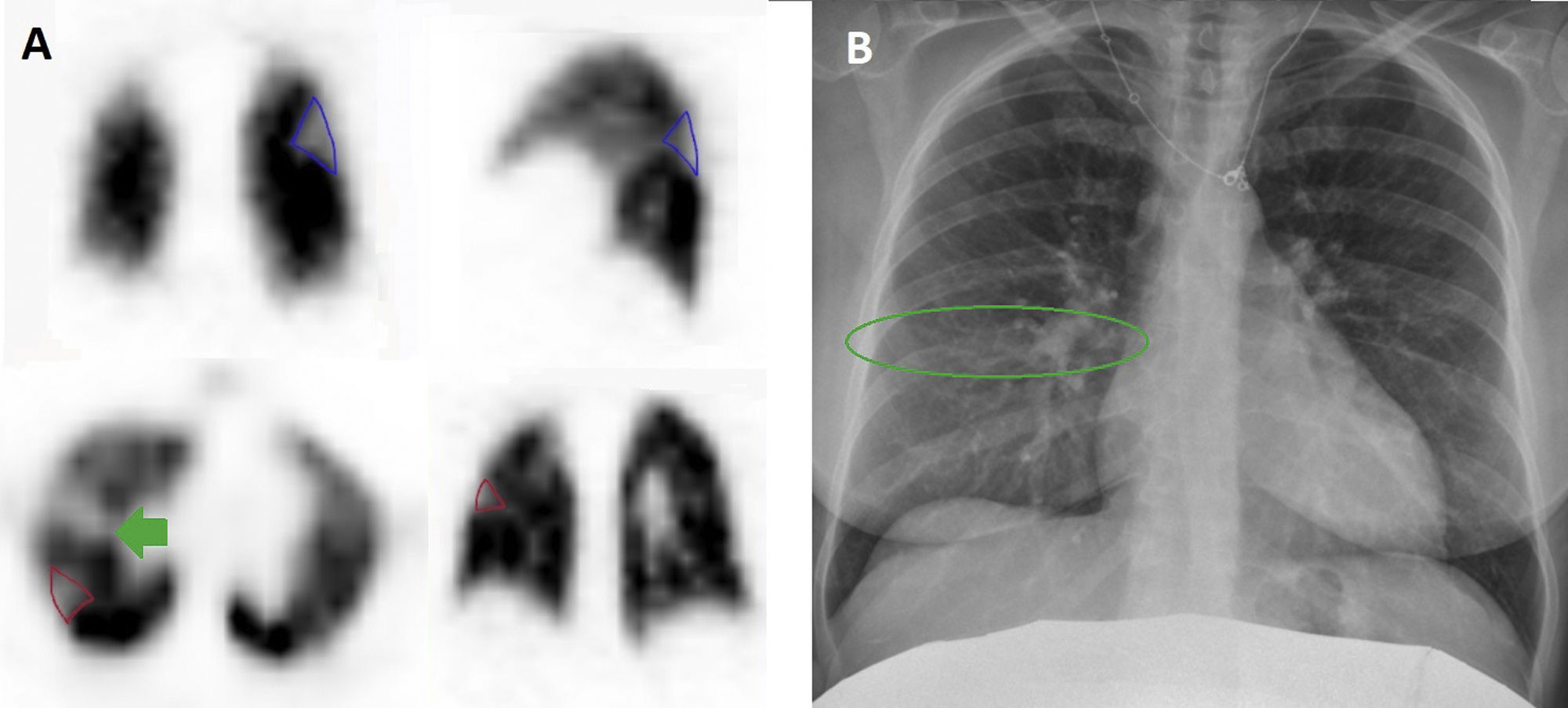
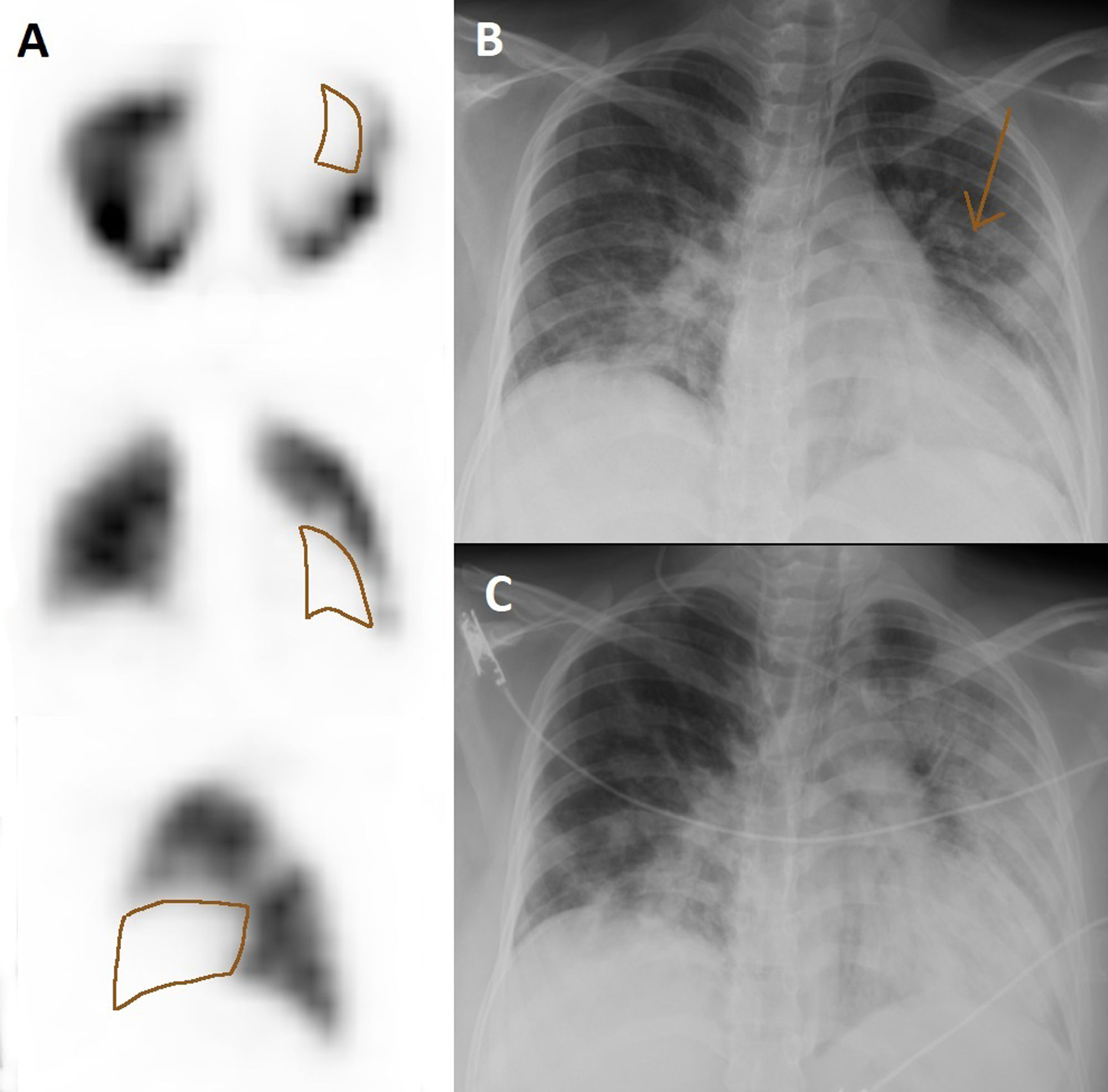
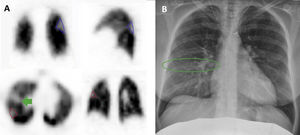
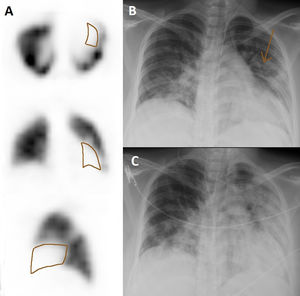
Among the 4 remaining pregnant women in whom PTE was discarded, 2 presented defects coinciding with an area of infiltrate by COVID-19 pneumonia in the chest radiography (Figs. 2 and 3) and the other 2 did not present clear perfusion defects. Anticoagulation was discontinued in all these patients. One woman required an urgent cesarean due to worsening of the pulmonary infection, and the remaining 3 patients delivered at term with no incidences of note.
On minimum suspicion of PTE, pregnant women should receive anticoagulation due to their condition, assuming a greater risk of bleeding and the need for close monitoring, and thereby making it essential to rule out the presence of thrombotic phenomenon early. Although the d-dimer values in patients diagnosed with PTE are practically double those of other patients, this value continues to be a very variable and unspecific parameter. Despite the predisposing factors, PTE was ruled out in 4 of the 5 patients studied, with the progression of COVID-19 thereby more frequently being the cause of clinical worsening in the patients than PTE. If we take into account the medium-long-term effects, it is also more severe for the fetus, since the only patient who had to undergo a cesarean section for fetal suffering was the woman who presented a worsening of COVID-19 pneumonia, ruling out PTE, compared to the women diagnosed and treated for PTE and who had an uneventful delivery at term. In addition, it should be noted that this latter patient presented a peripheral sub-segmentary distribution of the perfusion defects in the scintigraphy in accordance with what other authors have described in patients diagnosed with PTE using this technique during COVID-19 infection16.
Given the unspecific nature of the clinical manifestations and d-dimer values within the context of COVID-19 as well as their similarity with those of PTE, pulmonary perfusion scintigraphy plays a fundamental role in the diagnosis of PTE due to its high sensitivity and less irradiation than CT.
The exponential evolution of the COVID-19 pandemic and the scarce scientific evidence produced a critical time and a challenge for medical professionals responsible for the diagnosis, treatment and psychological support of affected patients and relatives. Most hospital departments have had to adapt their usual clinical practice protocols for the exploration of the airways as in the case of ventilation scintigraphy. Therefore, taking into account the absence of scientific publications in this group of patients within the exceptional setting of the COVID-19 pandemic, we consider that the results obtained are of special relevance, despite the limited number of patients studied.
Conflict of interestThe authors have no conflicts of interest to declare.