Dermatophytoses are skin superficial mycoses in which clinical manifestations are directly related to the virulence of the infecting microorganism or the host immunity.
Case reportWe describe a severe case of dermatophytosis associated with exfoliative erythroderma, substantial palmoplantar keratoderma, onychodystrophy affecting all nails, diffuse non-scarring alopecia and tissue fungal invasion by Trichophyton tonsurans, which led us to the diagnosis of AIDS.
Direct examination and culture for fungi from skin scraping from two different sites were performed. Biopsy and histopathological exam were also performed on three different sites. Direct examination of the lesions’ scraping revealed septate hyaline hyphae and arthroconidia, identified as Trichophyton tonsurans by culture in glucose Sabouraud agar and Mycosel agar. A scalp biopsy revealed follicular fungal invasion and Majocchi's granuloma. Due to the severity of the presentation we requested an anti-HIV serology, which was positive. The patient was treated with itraconazole, 200mg/day, for 120 days, which promoted a complete regression of the lesions.
ConclusionsSevere and atypical forms of dermatophytosis could lead to a diagnosis of AIDS.
Las dermatofitosis son micosis cutáneas superficiales cuyas manifestaciones clínicas están relacionadas directamente con la virulencia del microorganismo involucrado y la inmunidad del huésped.
Caso clínicoSe describe un caso grave de dermatofitosis asociado con eritrodermia exfoliativa, con apreciable queratodermia palmoplantar, onicodistrofia de las 20uñas, alopecia no cicatricial difusa e invasión fúngica del tejido por Trichophyton tonsurans, lo cual permitió establecer el diagnóstico de sida.
Se llevó a cabo exploración directa y cultivo de hongos de dos muestras tomadas por raspado en dos localizaciones distintas. También se llevaron a cabo una biopsia de piel y un estudio histopatológico de tres localizaciones. En la exploración directa del raspado de las lesiones se observaron hifas tabicadas hialinas y artroconidios; en el cultivo en agar Sabouraud con glucosa y agar Mycosel se aisló Trichophyton tonsurans. La biopsia de cuero cabelludo mostró una invasión fúngica folicular y la existencia de un granuloma de Majocchi. La gravedad del cuadro motivó la solicitud de la serología para el VIH, que fue positiva. Se trató al paciente con 200mg/día de itraconazol durante 120días, lo que llevó a la remisión completa de las lesiones.
ConclusionesUna dermatofitosis grave o atípica podría considerarse enfermedad reveladora de sida.
Dermatophytoses are superficial cutaneous mycoses that affect keratinized tissues.1 The dermatophyte fungi belong to the genera Trichophyton, Microsporum and Epidermophyton. Regarding their primary habitat, they are classified in zoophilic, geophilic and anthropophilic.
The clinical presentation of infections caused by dermatophytes depends on many factors: host's defenses against fungi, virulence of the infecting microorganism, anatomical site of infection and environmental characteristics. Dermatophyte infections cause specific humoral and cellular immune response, and the protective response against dermatophytes is mainly mediated by hypersensitivity reaction of the delayed type.2
HIV patients usually have superficial mycoses in many stages of the disease. The lesions may be atypical, extensive and severe.2 Although Trichophyton rubrum is the main cause of dermatophytosis among these HIV patients, we report a serious and atypical case caused by Trichophyton tonsurans, with extensive involvement of the skin, nails and hair, follicular tissue invasion and formation of Majocchi's granuloma, which led us to the diagnosis of AIDS.
Clinical case studyA 45-year old male, construction worker, divorced and chronic alcoholic was referred to the National Institute of Infectious Diseases/FIOCRUZ in Rio de Janeiro. The patient reported a two-year history of erythema and scaling of the entire tegument associated with palmoplantar hyperkeratosis. Ten years before, similar symptoms were treated in another medical service with clinical improvement.
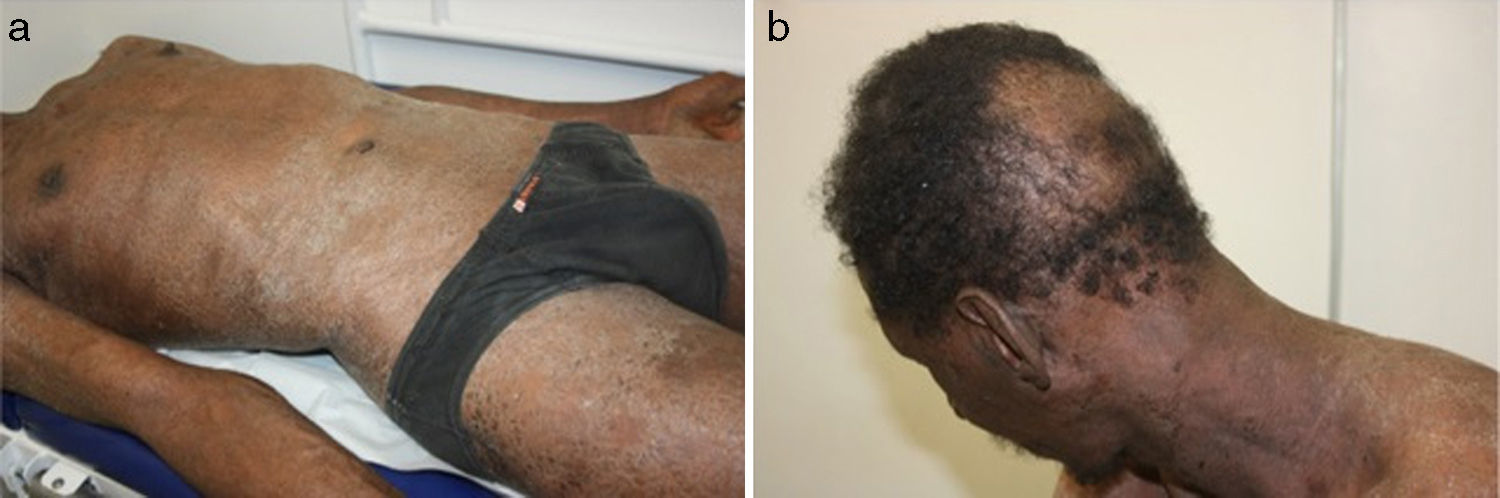
The physical examination revealed erythema and scaling of the entire skin surface, thus establishing the diagnosis of exfoliative erythroderma (Fig. 1a) associated with subungual hyperkeratosis dystrophy of all nails and onychogryphosis. The patient also had cervical, axillary and inguinal lymphadenomegaly, and we observed areas of diffuse non-scarring and circumscribed alopecia on the scalp (Fig. 1b) as well as face infiltration and madarosis. In the palmoplantar areas, substantial hyperkeratosis was present, forming corneous projections of up to 3cm (Fig. 2a and b). The patient's tongue was bright and smooth with no papillae and white plaques on the oral mucosa consistent with the diagnosis of oral candidiasis.
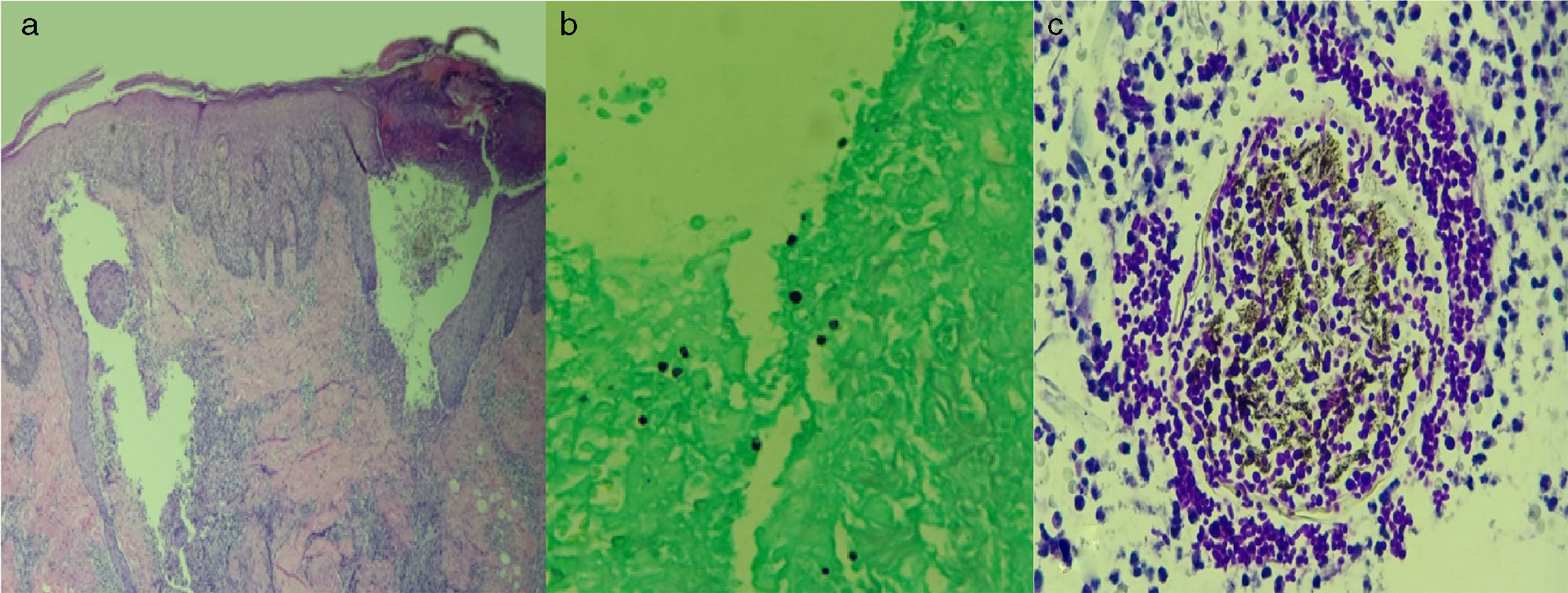
The diagnosis could be crusted scabies or dermatophytosis. We requested anti-HIV (reactive) and anti-HTLV (non-reactive) serology; the hemogram revealed leukopenia while other laboratory tests were normal. We performed three skin biopsies (scalp, upper right eyelid and right arm). Histopathology revealed acanthosis and hyperkeratosis with fungal hyphae present in the stratum corneum (arm and right eyelid). It also showed follicular inflammation and rupture of the adnexal epithelium with lymphohistiocytic granulomatous infiltrate and fungal elements at the follicular epithelium/dermal interface (scalp), compatible with Majocchi's granuloma. (Fig. 3a–c).
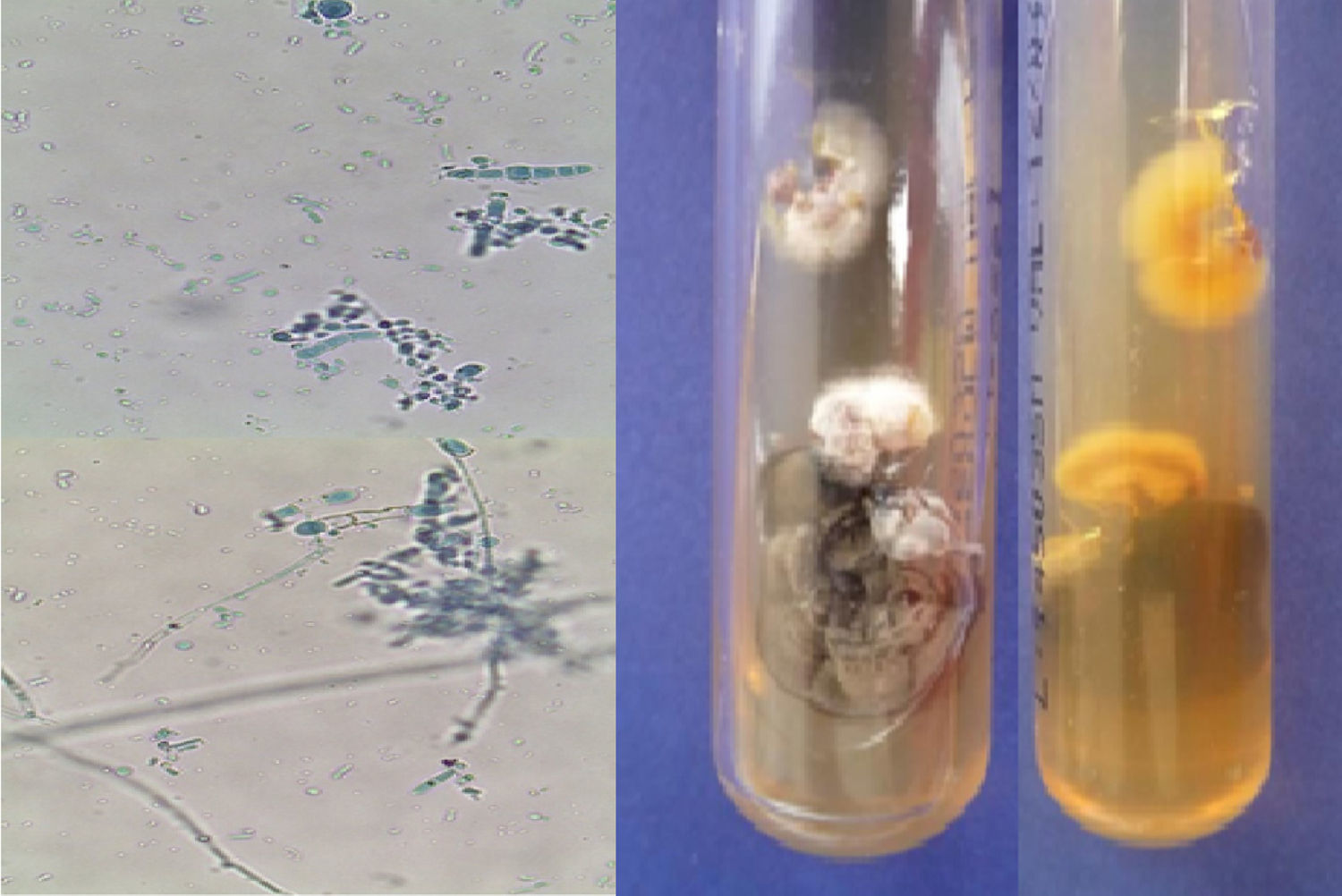
No ectoparasites were found. However, the scrapings from the right arm and the palmar hyperkeratosis were subjected to fungal culture wich revealed septate hyaline hyphae growth with tear-drop-shaped microconidia and cigar-shaped macroconidia with transverse septa, which led to identify the isolate as Trichophyton tonsurans. The patient was treated with itraconazole 200mg/day and applications of salicylic vaseline at 25% in palmoplantar areas. There was a complete regression of exfoliative erythroderma and palmoplantar hyperkeratosis after 28 and 90 days, respectively. (Fig. 4a and b).
DiscussionDermatophytosis, particularly tinea pedis and/or onychomycosis, is common in HIV patients.3–5 Da Silva evaluated 44 HIV-positive patients and 40 patients with AIDS and did not find a relationship between the risk of developing dermatophytosis and the CD4+ lymphocyte count and/or CD4+/CD8+ratio. These findings suggest that there is no direct relation between the immunosuppression degree and the risk of developing dermatophytosis.6 However, the same author observed that dermatophytosis was more frequent in patients with viral load greater than 100,000copies.
On the other hand, atypical forms of dermatophytosis have been linked to AIDS.7 This report emphasizes the severity of clinical manifestations that led us to the diagnosis of AIDS. During the investigation, the CD4+ count was 177cells/mm3 and the viral load was 30,455copies/ml, which configure an advanced immunosuppression. It is possible that the association of alcoholism/immunosuppression resulted in the severity of the clinical manifestations.
Dermatophytosis in pacients with HIV and Majocchi's granuloma is commonly due to T. rubrum. However, in this case, the agent found was T. tonsurans. Among 84 HIV patients, Da Silva did not find any case of dermatophytosis caused by T. tonsurans, while Ilkit, in an article review of 79 cases of Majocchi's granuloma, found T. tonsurans in only 7.5% of them.8 Clinically, Majocchi's granuloma is presented as perifollicular papules in areas subject to trauma in individuals with chronic dermatophytosis. Occasionally, nodules, plaques or abscesses may appear in immunocompromised patients. Lesions are more common in extremities, rarely shows cephalic involvement.9 Histopathologically, Majocchi's granuloma is characterized by perifollicular dermal granuloma and abscesses associated with the detection of spores, hyphae and arthrospores in hair, hair follicles or dermal inflammatory infiltrate. However, in immunocompromised patients, there may be greater tissue necrosis, major abscess formation and absence of granulomas.10
Adults infections by T. tonsurans usually manifest as tinea corporis,3 with frequent recurrences. In our case, the skin, the hair and all nails were affected. It is possible that our patient had already had a severe dermatophytosis in the past, but it was not possible to determine if he was already HIV positive at that time.
The excellent response to the treatment, with a complete regression of the cutaneous lesions (Fig. 4 a and b) suggests that all clinical manifestations described above are exclusively due to dermatophytosis. Patients with extensive, refractory or chronic lesions, and/or immunosuppression should receive systemic treatment for a long period of time. Contact with the reservoir of infection is relevant due to dissemination, which explains why the study of the patient's close contacts is essential to identify possible sources of reinfection since recurrences are frequent in these patients.3
This case is relevant because its clinical manifestations were rare and severe. There are only few reports of Majocchi's granuloma related to T. tonsurans in HIV patients. It is worth to highlight that severe and atypical forms of dermatophytosis can lead to the diagnosis of AIDS.