Sporotrichosis is a subacute or chronic mycosis acquired by traumatic inoculation or inhalation of fungal conidia. It is caused by the dimorphic fungus Sporothrix, which causes different clinical presentations, being the cutaneous and lymphocutaneous variants being the most frequent. The disseminated cutaneous form is a rare presentation occurring in a minority of cases in Mexico.
Case reportWe report an atypical case of disseminated sporotrichosis in an alcoholic and iatrogenically immunosuppressed patient, whose clinical lesions resembled tumoral-stage mycosis fungoides. Histological examination and culture revealed the presence of Sporothrix schenckii.
ConclusionsThe patient was treated with itraconazole 200mg per day for 4 months with clinical resolution. To the best of our knowledge, this is the first report of this type of clinical manifestation.
La esporotricosis es una micosis subaguda o crónica adquirida por inoculación traumática o inhalación de conidias fúngicas. Está causada por el hongo dimórfico Sporothrix, y puede presentar distintas manifestaciones clínicas, si bien las variantes linfocutánea y cutánea son las más frecuentes. La forma cutánea diseminada es una presentación infrecuente que se ha observado en una minoría de casos en México.
Caso clínicoInformamos de un caso atípico de esporotricosis diseminada en un paciente alcohólico y con inmunosupresión iatrogénica, cuyas lesiones se asemejaban a una micosis fungoide en fase tumoral. La observación histológica y el cultivo demostraron la presencia de Sporothrix schenckii.
ConclusionesEl paciente fue tratado con 200mg de itraconazol diarios durante 4 meses con resolución clínica. Este es el primer informe en relación con esta manifestación clínica.
Sporotrichosis is a worldwide fungal infection caused by the inhalation or traumatic inoculation of spores of the dimorphic fungus Sporothrix schenckii complex.1,9,19 It is a polymorphic disease that has two clinical forms, localized and systemic (disseminated), although the most common presentation is a subacute or chronic subcutaneous process. Molecular studies have shown that the S. schenckii complex includes species that have not been completely characterized, such as Sporothrix albicans, Sporothrix brasiliensis, Sporothrix globosa, Sporothrix luriei, Sporothrix mexicana, and S. schenckii.9 Sporotrichosis has a relatively high incidence in Latin American countries such as Mexico, where it is frequent in the central and occidental areas of the country.6,19 It is seen in both genders and at all ages, although it is more common among children and young adults in this part of the world.4,6,19 It is considered an occupational infectious disease because miners, farmers, gardeners, and carpenters are frequently affected due to exposure to the natural habitat of this microorganism.1,6,19 Indirect vectors such as rats, mice, cats, and squirrels have also been described.1 We present the case of an alcoholic and iatrogenically immunosuppressed patient with disseminated cutaneous sporotrichosis with mycosis fungoides-like lesions.
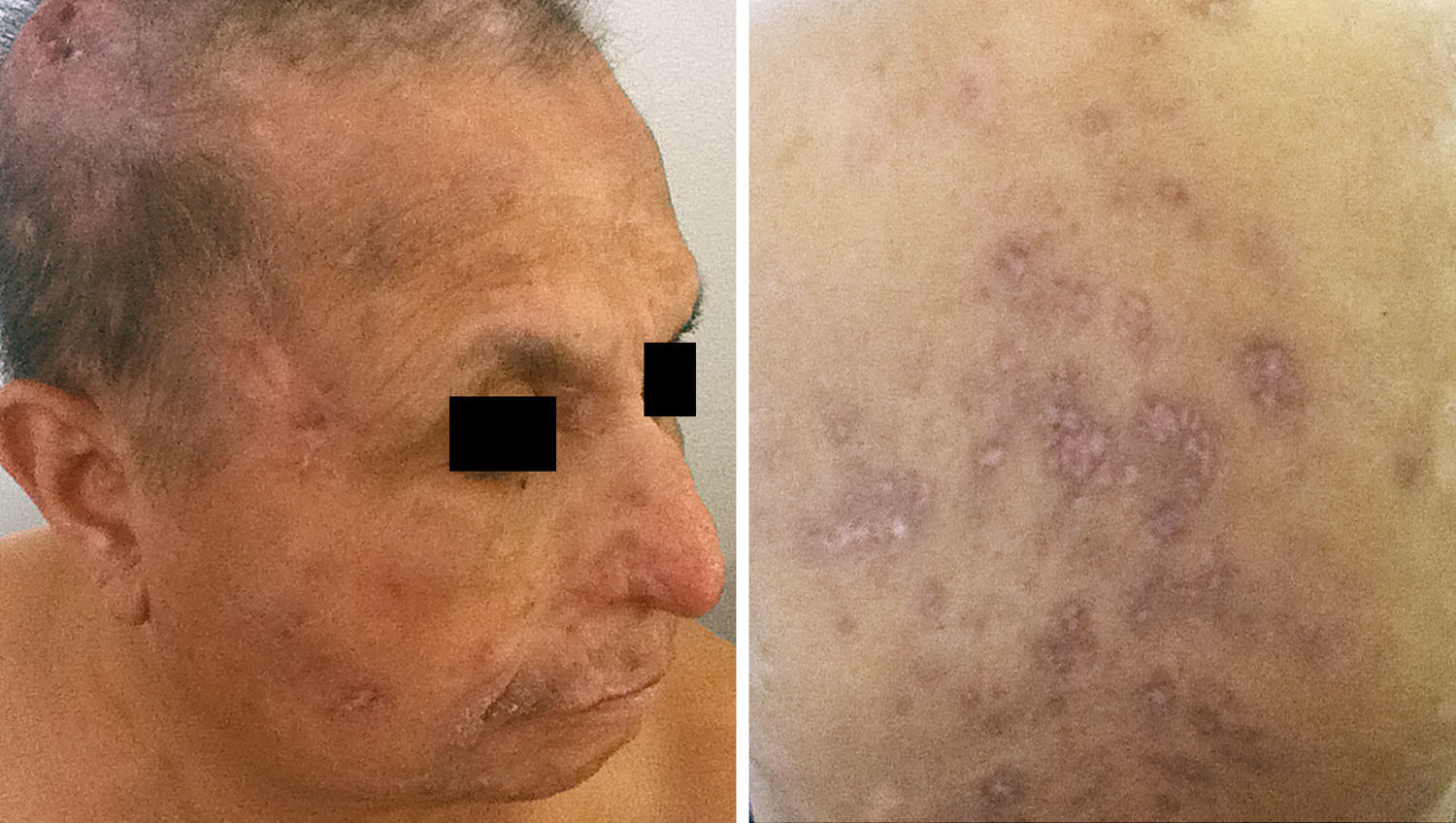
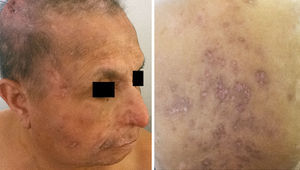
Case reportA 68-year-old male farmer from Durango, Mexico, presented to his local family physician with a 4-year history of asymptomatic scaly nodules and plaques on his face. These lesions were treated with topical antibiotics and steroids with transient and partial involution. Five months later, the nodules and plaques progressively increased in size evolving into tumors. Similar lesions appeared on the thorax, abdomen and limbs. Symptoms of malaise, intermittent fever, and a 10% loss of his usual weight were also present. The patient was reexamined by an internist who prescribed oral prednisone 50mg/day, and topical mometasone 0.1% with a presumptive diagnosis of mycosis fungoides, supported by the clinical presentation and the histological study of a facial lesion. After three weeks of treatment, the patient exhibited clinical worsening with new nodular lesions, ulceration, and tumor enlargement. The patient was referred to a dermatology center.
The patient had a 20-year history of high blood pressure with irregular treatment, a 18 pack-year history of smoking, and 500g of alcohol consumption per week. He did not remember any scratching, trauma, or skin puncture by thorns or organic material. Physical examination revealed asymptomatic multiple scaly nodules, tumors and ill-defined plaques 2 to 8-cm in diameter without tenderness, disseminated to the head, thorax and limbs, some with ulceration (Fig. 1). Painless bilateral cervical and clavicular adenopathy was found.
A complete blood cell count showed hemoglobin of 9.5g/dl, and hematocrit of 29.5%. The white cell count was 17,769 neutrophils/mm3, 2160 lymphocytes/mm3, and 4080 eosinophils/mm3. A buffy coat smear for Sézary cells, a chest X-ray and a thoracoabdominal CT scan were normal. Serology for HIV was negative.
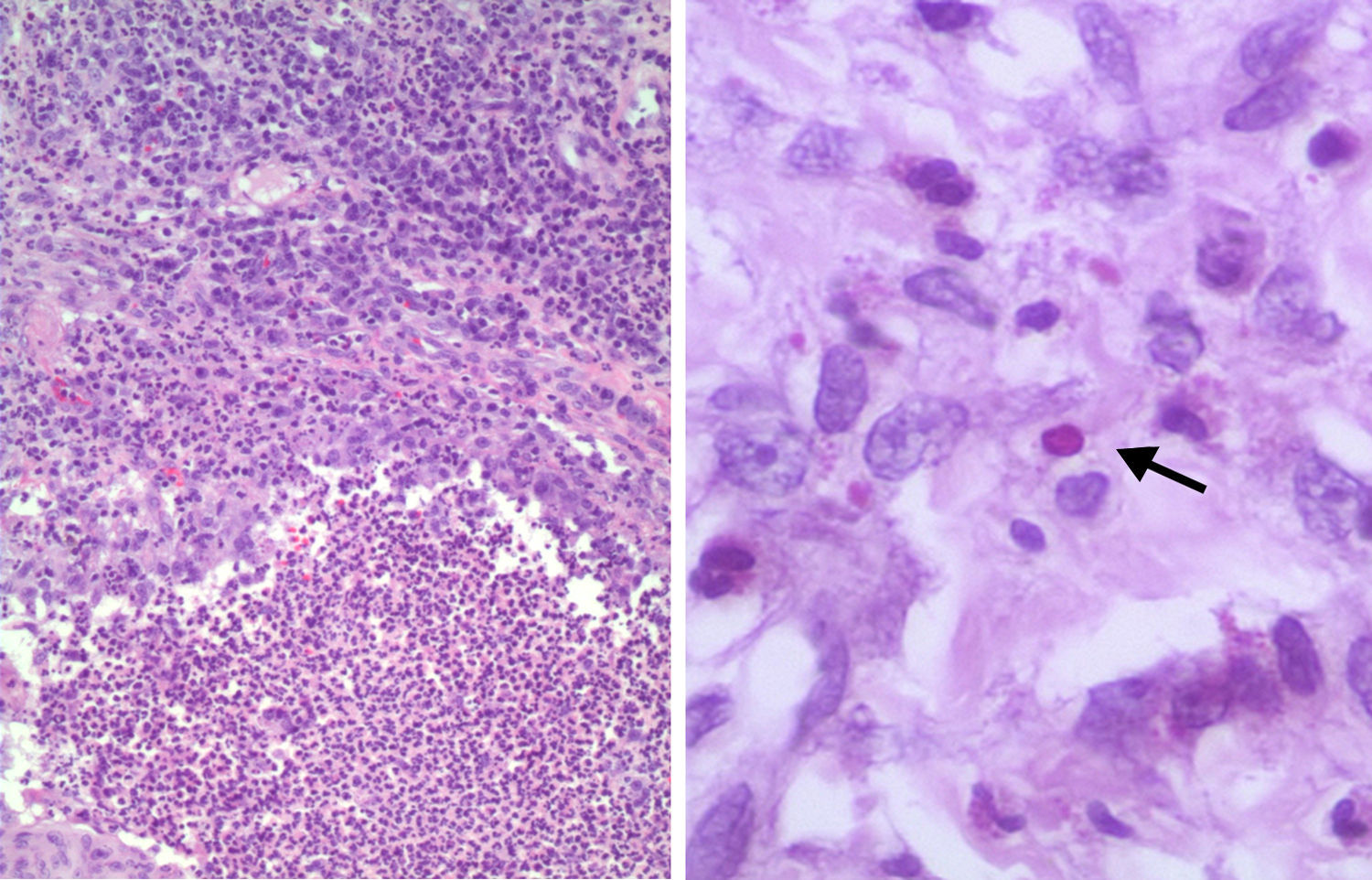
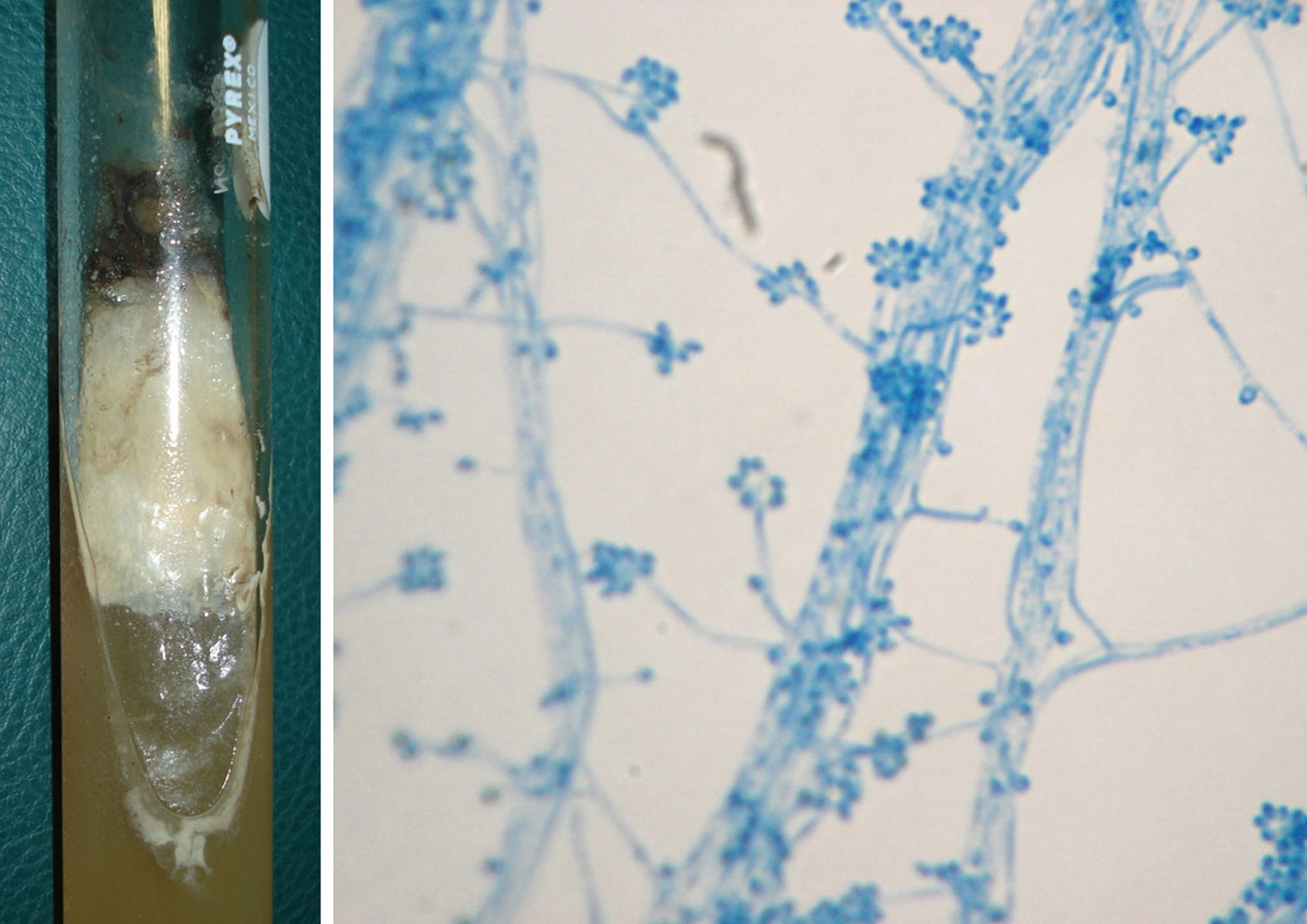
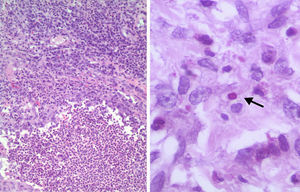
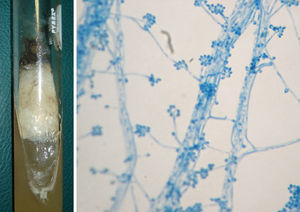
Histologic examination of nodules on the right cheek and upper thorax revealed a suppurative granulomatous dermatitis. A biopsy specimen showed hyperkeratosis, acanthosis, and a diffuse infiltrate of granulocytes, lymphocytes, and plasma cells throughout the dermis. Periodic acid-Schiff (PAS) stain revealed the presence of yeast forms, 2–4mm with enhancement of their walls (Fig. 2). Special stains for bacteria and acid-fast bacilli were negative. Tissue fungal culture on Sabouraud agar grew Sporothrix schenckii. Septate hyphae with conidia arranged in rosette-like clusters were observed after staining with lactophenol aniline blue (Fig. 3). The treatment was started with oral itraconazole, 200mg/d which showed marked improvement over the first six weeks with normalization of white blood cells parameters, and complete remission after 4 months of treatment (Fig. 4).
Suppurative granuloma with central microabscesses composed of neutrophils surrounded by epithelioid cells, and a peripheral zone infiltrated by lymphoid and plasma cells (hematoxylin-eosin stain, 100×) (left). An oval body (4μm in diameter) with a lighter center and darker stain at the periphery is seen, suggestive of Sporothrix yeast (PAS stain, 400×) (right).
Sporotrichosis is a polymorphic disease with lymphocutaneous, fixed, and disseminated clinical variants.1,9,19 The most common lesions are fixed and lymphocutaneous. The typical course of disease begins days to weeks after inoculation with a nodule or ulcer at the site of entrance.1,9,19 Lesions enlarge slowly, and form satellite nodules progressing along regional lymphatics. Disseminated cutaneous sporotrichosis is characterized by more than three skin lesions in two different anatomical sites without extracutaneous involvement.19 This clinical presentation is rare, accounting for less than 2% of the cases, and is usually associated to immunosuppression, where the fungus acts as an opportunistic pathogen.1,9,19 Host immunity is hypoergic or anergic.1,5,19 Risk factors include alcoholism, diabetes, AIDS, pregnancy, malnutrition, malignancy, and immunosuppressive therapy.5,19 In these settings, lesions are usually nodules, gums, and ulcers. Some disseminated variants have been associated to pyoverrucoid syndromes consisting of necrotic ulcers, erythematous nodules, and verrucous plaques with hematic crusts.5 However, most cases are not easily recognized due to unusual histological and clinical manifestations for even years before the diagnosis.5 These atypical presentations may be related to the pathogenicity, virulence and infectivity of the Sporothrix strains, geographical factors, site of inoculation, and immunological status of the patient, among others.1,8 However, no differences between the pathogenicity and clinical setting among several species of Sporothrix complex have been proved.8
Although the diagnosis of cutaneous sporotrichosis is basically clinical, it must be confirmed by culture. Few conditions are considered in the differential diagnosis and these include leishmaniasis, chromoblastomycosis, cutaneous tuberculosis, and chronic staphylococcal lymphangitis.5
There are worldwide reports from endemic countries concerning infrequent cutaneous presentations. Some include keratoacanthoma,7 sarcoidosis,20 arachnidism,10 chronic ulcer,13 cryptococcosis,16 mycetoma,17 moluscum,15 soft tissue tumor,12 leprosy,18 and pyoderma gangrenosum.2 We could not find previous reports of disseminated sporotrichosis manifesting as nodules and tumors such as in mycosis fungoides. The similarity between these lesions and those observed in the tumoral stage of a cutaneous lymphoma may confuse the unskilled physician. However, the clinical history and histological features rule out this diagnosis.
It is assumed that the Sporothrix cell-wall polysaccharide fraction is responsible for its immunogenicity. After fungal antigens are processed and recognized, a TH1 response is elicited.14 Interestingly, we found suppurative granulomas in these lesions, which are common among variants with preserved immunity, such as fixed and lymphangitic.11 Therefore, we think that this clinical expression resembling mycosis fungoides-lesions could have been favored by an indeterminate inflammatory response. This is supported by the absence of the expected tuberculoid granuloma observed in disseminated variants, along with the chronic clinical setting, and the parasitic fungal yeasts observed in tissues.11 Unfortunately, the sporotrichin test was unavailable.
Concerning treatment, a favorable outcome as that observed in this patient confirms the usefulness of itraconazole in sporotrichosis associated to immunosuppression and disseminated clinical forms.3,6 Although this case was complex, it clearly demonstrates that clinical expression is greatly determined by the immune response to the fungus. Therefore, careful attention to the individual's personal life such as this patient's occupation, his history of alcoholism and the fact that he lives in an endemic area, as well as a thoughtful interpretation of the skin biopsy and appropriate culture, should provide a correct diagnosis in similar cases.