The study aimed to evaluate the effect of acupuncture in the treatment of chronic non-specific low back pain (NSLBP).
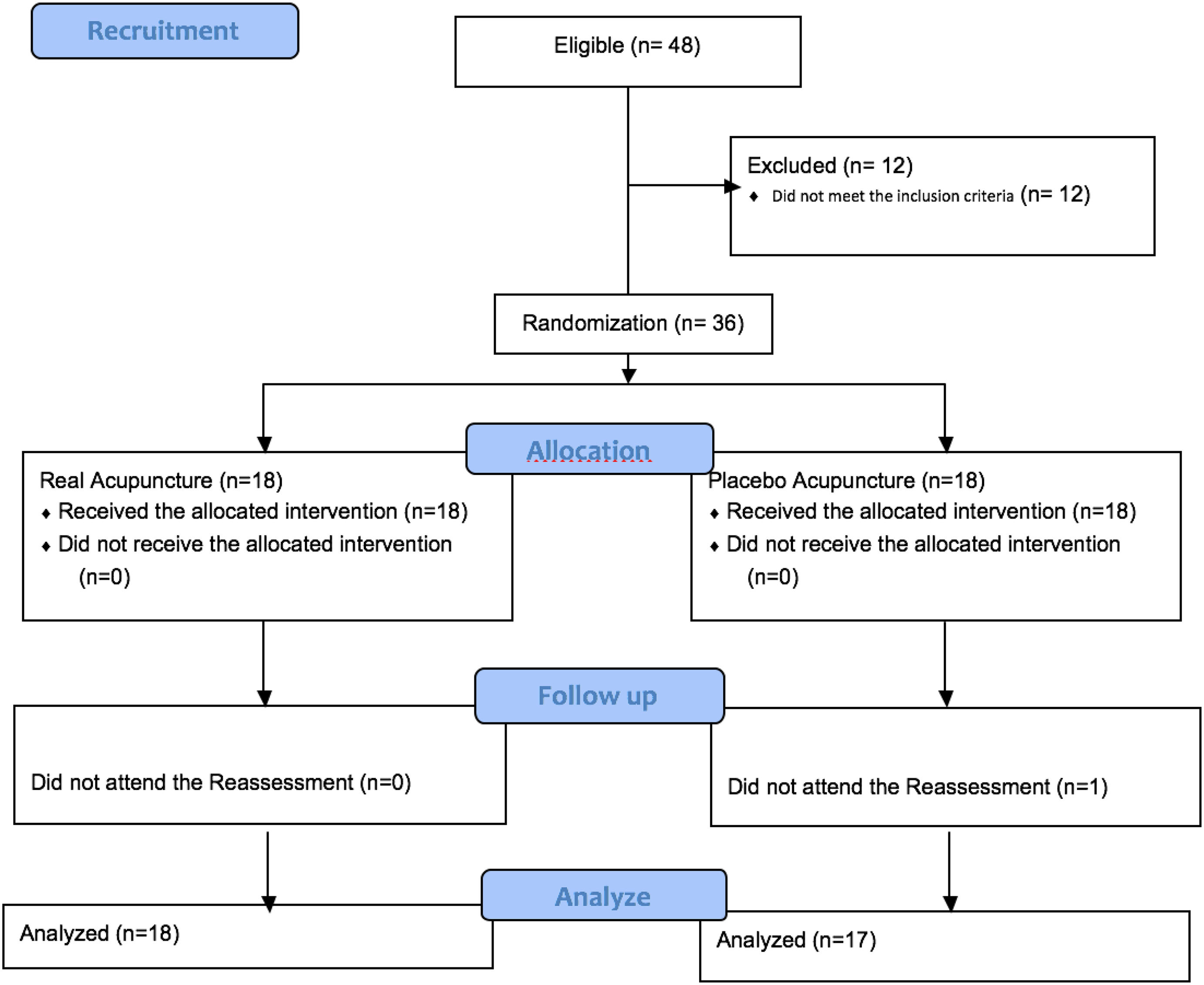
MethodsIt is a randomized, double-blind, placebo-controlled clinical trial. It was developed at the outpatient clinic of the physiotherapy department at the Federal University of Sergipe. 36 individuals were selected and allocated into 2 groups, but finalized 18 subjects in the Real Acupuncture group (RA) and 17 in the Placebo Acupuncture group (PA), due to an individual not completing the treatment with acupuncture or Placebo Acupuncture, being evaluated the intensity and characterization of pain. Subjects were treated three times a week, on alternate days, totaling 10 sessions.
ResultsAfter each of session, pain intensity was significantly lower at rest (p<0.028) and movement (p<0.035) in the RA group. In the PA group, pain intensity at rest (p=0.008) and movement (p=0.038) were significantly lower after 10 sessions. There was a significant reduction in the number of words selected (NWC; Br-MPQ) in the RA group when comparing sessions 1 and 10 (p=0.004). And there was a significant decrease in NWC between 1st and 10th session in the PA group (p=0.017). Regarding the pain classification index (PCI), there was a significant reduction (p=0.001) when comparing the 1st and 10th session in the RA group. When comparing RA and PA groups, the only significant difference was that CST of the right lower back was significantly lower in the AP group after the 1st and 10th sessions (p=0.028).
ConclusionIt was concluded that acupuncture on NSLBP patients in the RA group decreased intensity of pain after each session, the NWC and the PCI in the measurement of pain. However, there was no evidence of improvement in sensory tests, psychoemotional aspects and quality of life.
El estudio tuvo como objetivo evaluar el efecto de la acupuntura en el tratamiento del dolor lumbar crónico inespecífico (IDLC).
MétodosEs un ensayo clínico aleatorizado, doble ciego y controlado con placebo. Fue desarrollado en la consulta externa del departamento de fisioterapia Universidade Federal de Sergipe. Se seleccionaron 36 individuos y se distribuyeron en 2 grupos, pero finalizaron 18 sujetos en el grupo de Acupuntura Real (RA) y 17 en el grupo de Acupuntura Placebo (PA), debido a que un individuo no completó el tratamiento con acupuntura o acupuntura placebo, siendo evaluado el intensidad y caracterización del dolor. Los sujetos fueron tratados tres veces por semana, en días alternos, totalizando 10 sesiones.
ResultadosDespués de cada sesión, la intensidad del dolor fue significativamente menor en reposo (p <0.028) y movimiento (p <0.035) en el grupo de AR. En el grupo de AF, la intensidad del dolor en reposo (p = 0,008) y el movimiento (p = 0,038) fueron significativamente menores después de 10 sesiones. Hubo una reducción significativa en el número de palabras seleccionadas (NWC; Br-MPQ) en el grupo RA al comparar las sesiones 1 y 10 (p = 0,004). Y hubo una disminución significativa en NWC entre la 1ª y la 10ª sesión en el grupo de AF (p = 0,017). En cuanto al índice de clasificación del dolor (ICP), hubo una reducción significativa (p = 0,001) al comparar la 1ª y la 10ª sesión en el grupo de AR. Al comparar los grupos de AR y PA, la única diferencia significativa fue que el CST de la parte inferior de la espalda derecha fue significativamente menor en el grupo de AP después de la primera y la décima sesión (p = 0.028).
ConclusiónSe concluyó que la acupuntura en pacientes con IDLC en el grupo de AR disminuyó la intensidad del dolor después de cada sesión, la NWC y la PCI en la medición del dolor. Sin embargo, no hubo evidencia de mejora en las pruebas sensoriales, los aspectos psicoemocionales y la calidad de vida.
Low back pain is a disease with multifactorial origin that affects a considerable part of the population. It is the leading cause of disability in the world; however, in 85–90% of cases, it is not possible to make any specific diagnosis. This pathological condition can promote serious repercussions on the functional, psychosocial and socioeconomic aspects of the individual.1,2 Clinical disorders involving low back pain are often related to fatigue and muscle deficiencies indicative of inadequate and repeated postures, and consequences influence the individual in society as a whole, which can cause loss of health, loss of function, limitation of daily activities, work and leisure.3
There is an evolution in the treatments for analgesia and the clinical paradigms for patients with low back pain are rapidly evolving, mainly with regard to the decrease of pharmacological approaches, and the increase of non-pharmacological approaches, as for example transcutaneous electric nerve stimulation (TENS), among others, and the adoption of alternative therapies, such as acupuncture.4,5
Acupuncture has been reported as a safe, simple and effective pain treatment in clinical trials, the effects and mechanisms of action include production of steroids, opioids and other peptides in the central and peripheral nervous systems, through the introduction of needles in the body, decreasing the inflammatory process.6 It also has neuroendocrine mechanisms that stimulate the release of β-endorphin precursor substances that remain circulating throughout the body thus promoting prolonged analgesia.7
Although acupuncture is a widely used ancient technique, its isolated effect is still not well known, as this technique appears more associated with other conventional therapies. Although we know that the combination of different interventions has been the most recommended, and perhaps even more effective, for this pathological condition that is chronic pain, it is necessary to understand and be aware of the contribution of each technique alone. Therefore, the present study aims to evaluate the effect of acupuncture in the treatment of non-specific chronic low back pain.
Material and methodsType of studyThe study is a randomized, double-blind, placebo-controlled clinical trial. The patients were evaluated and treated at the outpatient clinic of the Federal University of Sergipe.
Patient recruitmentThe inclusion criteria in the study were: (1) to have a diagnosis of non-radicular low back pain and to present low back pain for more than three months; (2) age range of 20–55 years. Exclusion criteria included: (1) being in physical therapy in the last three months; (2) previous experience with acupuncture; (3) pregnant or puerperal women who gave birth in the last three months; (4) important deformities and/or amputations of lower limbs; (5) low back pain due to infection, tumor, radiculopathy or acute inflammatory processes; (6) cutaneous lesions in the affected region; (7) active infectious processes; (8) another disease of nervous or dermal tissue affecting the lumbar region; (9) invasive spinal surgery or examinations in the last three months; (10) inability to understand instructions or consent to the study; (11) psychiatric diseases; (12) neurological diseases (e.g., stroke, Parkinson's, Alzheimer's, brain tumor, dementia, multiple sclerosis, substance abuse) or pulmonary diseases such as chronic oxygen-dependent obstruction, which could seriously affect the test results.8; (13) heart disease, such as cardiac arrhythmia, angina pectoris, congestive heart failure, decompensated hypertension9; (14) severe comorbidity; (15) presence of auditory, visual or communication disorder; or (16) have severe cognitive/psychiatric disorders,9 patients were invited to participate due to a campaign offering the service of people with low back pain throughout the university campus.
For the calculation of the sample size, we considered data referring to the pain intensity variable in the pilot study, measured by the 11-point numerical scale, assuming standard deviation = 2, difference to be detected = 2. Significance level less than or equal to 5%, power of the test = 80%, obtaining a sample size of 17 subjects for each group, this number of subjects is on average, according to similar researches already carried out.10
Ethical aspectsThe project met the determinations of the Helsinki Resolution and complied with the determinations of Resolution 466/12 of the National Health Council (CNS) and was approved by the Human Research Ethics Committee of the Federal University of Sergipe (UFS). The same was registered in the Brazilian Registry of Clinical Trials (REBEC) with code RBR-4qxt3z. All subjects included in the study signed a free informed consent form (ICF) prior to the evaluation.
Study groupsSubjects were randomly allocated in two study groups, through numbered opaque envelopes, where the even and odd number, indicated which group the subject was directed to, this procedure was performed by an investigator who was responsible for directing the treatment, and had no contact with the researchers who carried out the evaluations, and guaranteed a double-blind study, since neither the patient nor the evaluator researcher knew which group the subject was allocated to: Real Acupuncture (RA) and Placebo Acupuncture (PA). In all groups, the subjects were instructed not to take analgesics and anti-inflammatories. The acupuncture points used were: B22, B26, B50, B53 which are points of the bladder meridian related to low back pain. In the Placebo Acupuncture group, the needles were placed at the same points used in group 1, but immediately after puncture, the needle was withdrawn so that it did not cause any systemic effects.11 The subjects were treated with acupuncture three times a week, every other day (Mondays, Wednesdays and Fridays), and totaling 10 visits.
Patient assessmentPain assessmentTo measure the intensity of pain, the numerical scale (NS) of 11 points (0–10) was used.12 Pain intensity was investigated during rest and movement. Values were recorded before and after each session. We also calculated the variation in pain intensity after each session (intensity of pain after the session subtracted from the intensity of pain before the session). It was also used the McGill Pain Questionnaire (BR-MPQ), translated and validated for Brazilian Portuguese by Pimenta and Teixeira (1996).13
Sensorial testsThe cutaneous sensory threshold (CST) was evaluated by the light static touch with von Frey monofilaments (North Coast®, Gilroy, California, EUA).
To assess CST at the pain site,14 the touch was performed at the A1 point bilaterally, located at the midpoint of the paravertebral muscle at the third lumbar vertebra level, with the patient positioned in the ventral decubitus position. A point distal to the pain site, point A2, located at the midpoint of the anterior tibialis muscle (ATM) at the anterior tubercle of the tibia, laterally was also chosen.
Pressure pain threshold (PPT)Pressure pain threshold (PPT) was measured with a digital pressure algometer (EMG System®, São José dos Campos, SP, Brazil, área of 1 cm2). The subjects were instructed to report when the sensation ceased to be just a pressure and became pain. The PPT test was performed at the same sites from CST testing. We also evaluated the temporal summation (TS), and conditioned pain modulation (CPM) phenomena, which are indirect neurophysiological measures of central facilitation and central pain inhibition, respectively.15 Through the TS test, it was verified whether a constant pressure stimulus would increase the magnitude of the perceived pain. In the MCD, it was observed if the ischemic pain in the opposite limb managed to inhibit the pain in the limb which the painful stimulus is being performed.
Muscle strength assessmentA lumbar dynamometer (EMG Systems do Brasil, São José dos Campos, SP, Brazil) was used to evaluate the strength of the musculature of this region, the patient was positioned in orthostatism, supported and parallel feet, extended knees, initially flexed at an angle of 130°–140°. At the verbal command of the evaluator, the subject used the greatest possible force during the movement of lumbar spine extension.
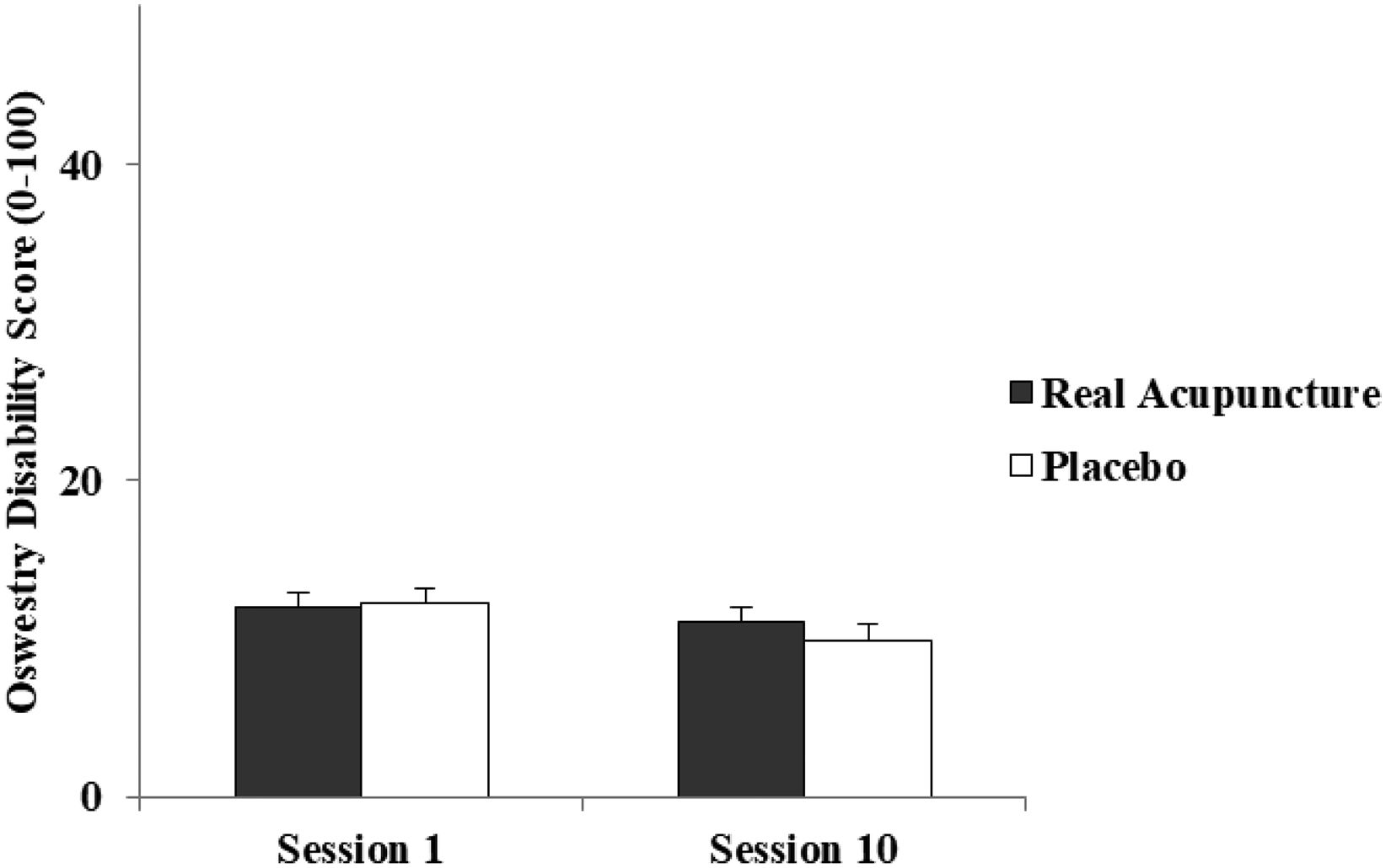
Motor function assessmentWe used the Oswestry Disability Index (ODI) scale, which evaluates pain-related withdrawal time in the last year.16 The subject was instructed to indicate the alternative that best represented his physical state. The Roland Morris Disability Questionnaire (RMDQ) was used as a valid and reliable measure for assessing the physical disability associated with chronic pain.17 The subjects were instructed to mark the alternatives considered true, according to their physical condition. These instruments were applied at the beginning of treatment and after 10 sessions in each group.
Psychoemotional evaluationThe Pain Catastrophizing Scale was used in the validated and adapted to Brazilian Portuguese version18 to measure negative perceptions and emotions associated with actual or predicted pain experiences.
The Tampa Kinesiophobia Scale was used to assess the subject's fear of moving and generating a new lesion.
In addition, the Fear Avoidance Beliefs Questionnaire (FABQ) was used in its was used in its Brazilian version version,19 this is an evaluation tool developed according to behavioral cognitive models that approach the fear, beliefs and avoidance behaviors of individuals with low back pain chronic illness in relation to physical activity and work.
Quality of life assessmentThe EuroQol EQ-5D instrument, which defines health through five dimensions, namely mobility, personal care, habitual activities, pain/discomfort and anxiety/depression20 was used to assess quality of life. This instrument was applied at the beginning of treatment and after 10 sessions in each group.
Statistical analysisInitially, the data were transported to an Excel for Windows 2010 spreadsheet and then to the SPSS program (Statistical Package for Social Sciences) version 16.0. Descriptive analysis was performed, with measures of mean and standard error of the mean.
Normality was tested through the Shapiro–Wilk in all analysis. In the intragroup analysis, data from the 1st and 10th sessions were compared in each group. When the data presented a normal distribution, the paired T-test was used. When given a non-normal distribution the before and after was compared through the Wilcoxon test. The daily variation in pain intensity at rest and in movement of the 10 sessions was analyzed using the Friedman test. This same test was used when comparing the seconds in TS and the moments in the CPM of each group.
In the intergroup analysis, independent T (if parametric) or Mann–Whitney (if not parametric) tests were used.
The chi-square test was used for the categorical variables (sex, occupation, physical activity, smokes, alcoholic drinking).
An intention-to-treat analysis was performed only in dynamometry, where there was loss of segment. For the accomplishment of the analysis, the average of the outcome was considered at each moment of the measurement. This analysis was performed in an attempt to avoid compromising the research results. Data with p-value <0.05 were considered statistically significant.
ResultsAs for the characterization of the sample, 18 patients were allocated to each group, and in the end, 18 remained in the RA group and 17 in the PA group, as shown in Fig. 1. In the personal and demographic characteristics, no significant differences were found between the groups.
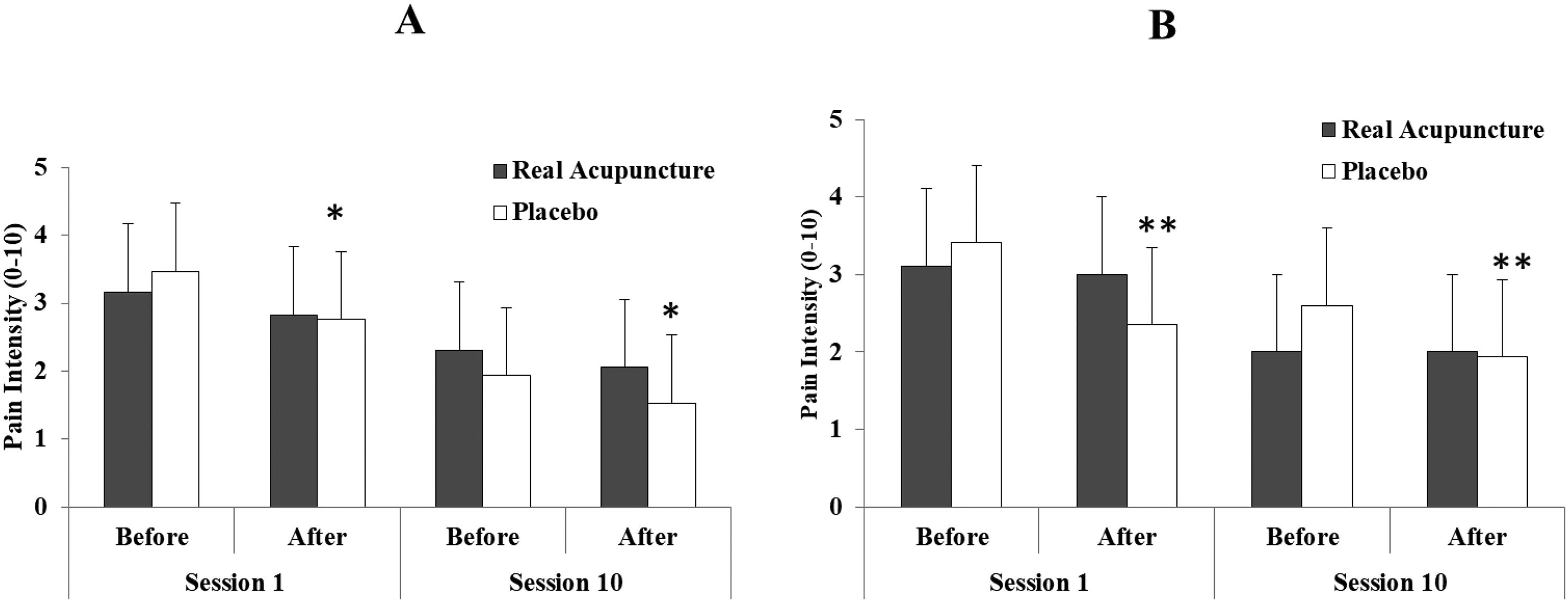
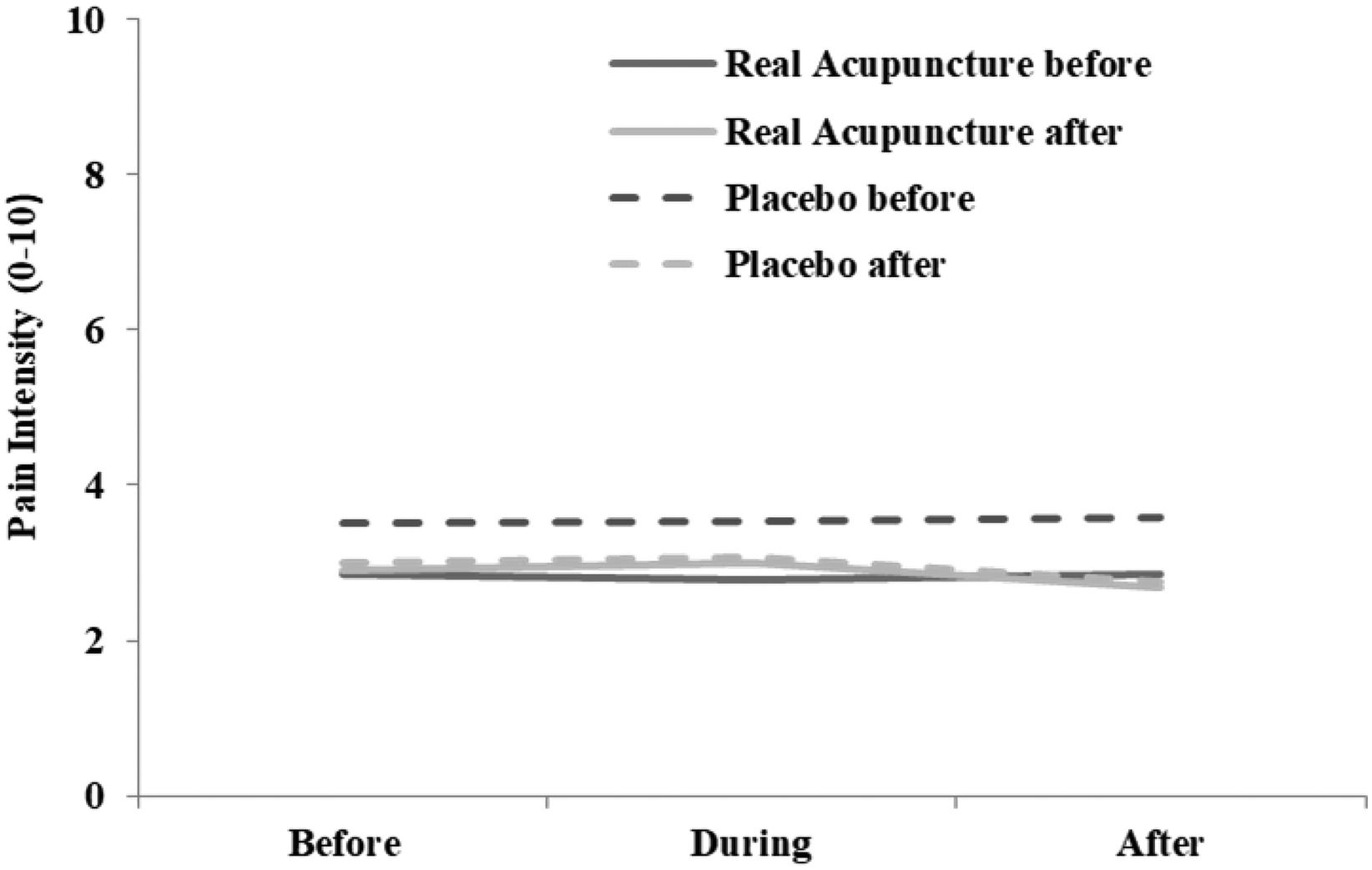
After each of the 10 sessions, pain intensity was significantly lower at rest (p < 0.028) and during movement (p < 0.035) in the RA group. In the PA group, pain intensity was also significantly lower at rest (p < 0.028) and movement (p < 0.017) after each session (Table 1). When comparing the 1st and 10th in the PA group, pain intensity at rest (p = 0.008) and movement (p = 0.038) were significantly lower after 10 sessions (Fig. 2).
Pain intensity after each of the 10 sessions at both rest and movement in the groups Real Acupuncture (n = 18) and Placebo Acupuncture (n = 17) in patients with chronic non-specific low back pain.
| Pain intensity | Real Acupuncture (RA) | Placebo Acupuncture (PA) | ||||
|---|---|---|---|---|---|---|
| Before | After | p | Before | After | p | |
| Rest | ||||||
| Session 1 | 3.16±0.47 | 1.76±0.40 | 0.003* | 3.47±0.65 | 1.64±0.53 | 0.003* |
| Session 2 | 3.05±0.63 | 2.22±0.59 | 0.006* | 2.88±0.60 | 2.23±0.55 | 0.066 |
| Session 3 | 2.94±0.67 | 1.94±0.52 | 0.004* | 3.17±0.52 | 2.11±0.42 | 0.017* |
| Session 4 | 2.76±0.52 | 1.41±0.42 | 0.002* | 2.17±0.57 | 1.58±0.52 | 0.028* |
| Session 5 | 1.94±0.45 | 1.52±0.40 | 0.071 | 2.29±0.54 | 1.29±0.40 | 0.017* |
| Session 6 | 2.82±0.53 | 1.82±0.59 | 0.002* | 2.11±0.43 | 1.23±0.33 | 0.010* |
| Session 7 | 2.76±0.59 | 1.94±0.52 | 0.007* | 2.47±0.52 | 1.52±0.44 | 0.004* |
| Session 8 | 2.68±0.53 | 1.75±0.46 | 0.028* | 2.23±0.57 | 1.58±0.47 | 0.009* |
| Session 9 | 3.00±0.65 | 2.00±0.56 | 0.002* | 1.82±0.65 | 1.35±0.56 | 0.066 |
| Session 10 | 1.70±0.49 | 1.23±0.37 | 0.026* | 1.93±0.60 | 1.33±0.49 | 0.017* |
| Movement | ||||||
| Session 1 | 3.94±0.67 | 2.94±0.60 | 0.035* | 4.52±0.70 | 2.41±0.71 | 0.002* |
| Session 2 | 3.88±0.71 | 2.94±0.69 | 0.003* | 3.88±0.70 | 3.29±0.67 | 0.088 |
| Session 3 | 3.29±0.55 | 2.35±0.51 | 0.002* | 3.76±0.58 | 2.64±0.50 | 0.016* |
| Session 4 | 3.64±0.58 | 1.94±0.51 | 0.001* | 2.94±0.55 | 1.94±0.53 | 0.006* |
| Session 5 | 2.22±0.48 | 1.66±0.43 | 0.020* | 3.29±0.61 | 2.05±0.42 | 0.007* |
| Session 6 | 3.05±0.61 | 2.00±0.57 | 0.002* | 3.35±0.56 | 2.35±0.58 | 0.004* |
| Session 7 | 3.23±0.61 | 2.52±0.60 | 0.011* | 3.00±0.54 | 2.35±0.49 | 0.013* |
| Session 8 | 3.12±0.54 | 2.18±0.52 | 0.031* | 3.23±0.55 | 2.29±0.58 | 0.004* |
| Session 9 | 3.47±0.65 | 2.35±0.62 | 0.031* | 2.82±0.66 | 2.05±0.60 | 0.017* |
| Session 10 | 2.35±0.55 | 1.82±0.46 | 0.016* | 2.80±0.64 | 1.93±0.57 | 0.007* |
Values in mean ± SEM (standard error of the mean). Tests Wilcoxon Matched Pairs.
Pain intensity at rest (A) and movement (B) of patients with non-specific chronic low back pain before and after the 1st session and before and after the 10th treatment. Wilcoxon Matched Pairs test. * p = 0.008 pain intensity at rest session 1 x session 10. ** p = 0.038 intensity of pain in motion session 1 x session 10.
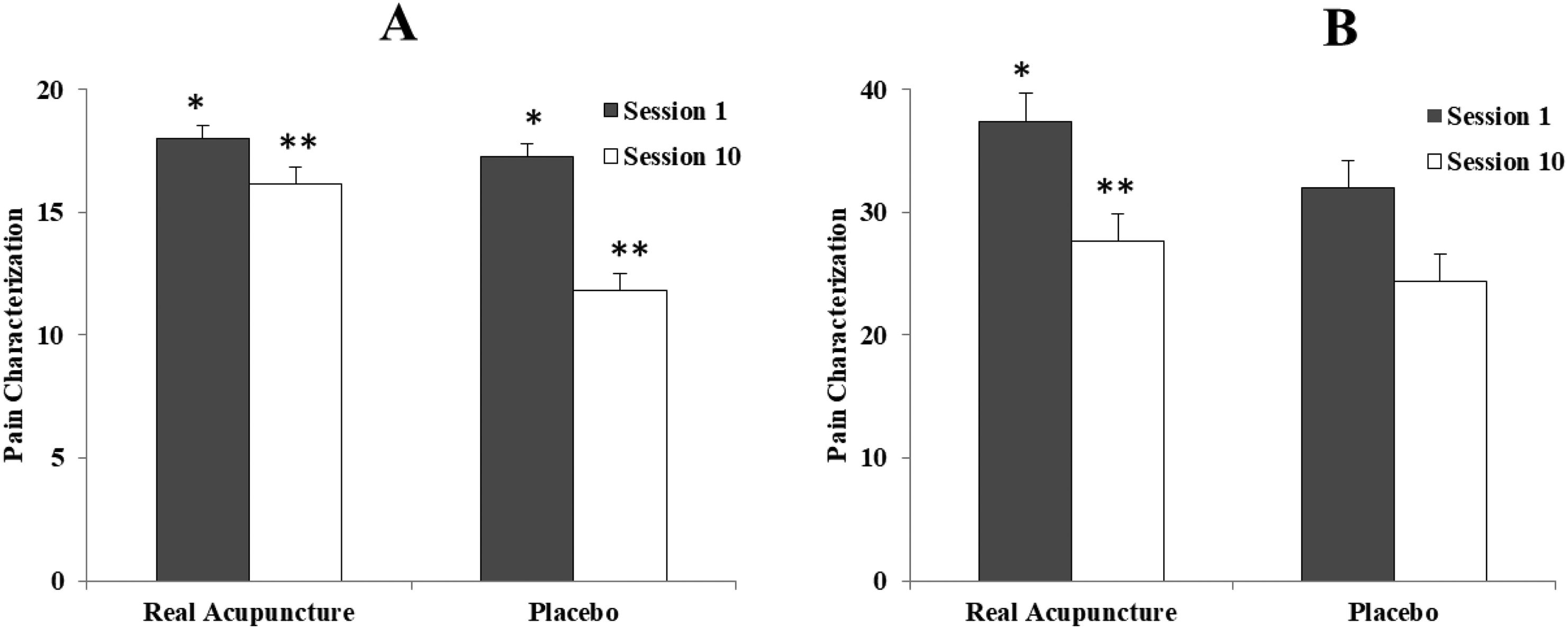
There was a significant reduction in the number of words chosen (NWC; Br-MPQ) in the RA group when comparing sessions 1 (18.00 ± 0.53 of 20) and 10 (16.15 ± 0.60 of 20) (p = 0.004 *). Similarly, there was a significant decrease in NWC between the 1st (17.25 ± 0.67) and the 10th (11.84 ± 1.76) session in the PA group (p = 0.017 *). Concerning the pain classification index (PCI), there was a significant reduction (p = 0.001 *) when comparing the 1st (37.40 ± 2.29 of 78) with the 10th session (27.65 ± 1.67 of 78) in the RA group. In the PA group, there was no significant difference (p = 0.051) in the comparison between the 1st (31.95 ± 2.22 of 78) and the 10th (24.41 ± 3.92 of 78) sessions (Fig. 3).
Characterization of pain of patients with non-specific chronic low back pain. A: number of words chosen and B: pain rating index. * p = 0.004 in the NPE comparison 1st and 10th session group AR; ** p = 0.017 in the NPE comparison 1st and 10th AP group session; * p = 0.001 in the 1st and 10th group ICD comparison AR group. Wilcoxon Matched Pairs test and Paired t-test respectively.
In the sensory tests comparing the RA and PA groups, the only significant difference was that the CST of the right lumbar was significantly lower in the RA group than in the PA group before the 1st session (p = 0.026). No difference was found between the groups in the left lumbar, right and left ATM (p > 0.05) before treatment. There was a statistically significant difference in CST, only in the RL region in the comparison after the 1st and 10th sessions (p = 0.028) in the PA group, and no significant difference was observed in the RA and PA groups before and after each daily treatment session (Table 2).
Cutaneous Sensory Threshold (CST) and Pressure Pain Threshold (PPT) before and after the 1st and 10th treatment sessions. Wilcoxon Matched Pairs test.
| Real Acupuncture | Placebo Acupuncture | |||||
|---|---|---|---|---|---|---|
| 1st | 10st | p | 1st | 10st | p | |
| CST | ||||||
| RL | 0.08±0.00a | 0.08±0.01 | 0.306 | 0.15±0.03 | 0.07±0.00 | 0.028* |
| LL | 0.14±0.04 | 0.13±0.05 | 0.888 | 0.11±0.02 | 0.10±0.02 | 0.876 |
| ATM R | 0.10±0.01 | 0.08±0.01 | 0.570 | 0.37±0.17 | 0.17±0.05 | 0.073 |
| ATM L | 0.10±0.02 | 0.13±0.03 | 0.474 | 0.40±0.17 | 0.20±0.05 | 0.722 |
| PPT | ||||||
| RL | 3.18±0.35 | 2.92±0.35 | 0.588 | 3.17±0.41 | 3.54±0.46 | 0.421 |
| LL | 3.02±0.38 | 2.92±0.35 | 0.837 | 3.00±0.43 | 3.83±0.52 | 0.068 |
| ATM R | 3.00±0.39 | 2.88±0.37 | 0.774 | 3.13±0.48 | 3.66±0.56 | 0.309 |
| ATM L | 3.02±0.37 | 2.82±0.38 | 0.856 | 3.16±0.46 | 3.46±0.44 | 0.943 |
Values expressed as mean ± SEM (standard error of the mean). Cutaneous sensory threshold (CST) in millinewton (mN) and pressure pain threshold (PPT) in kilograms-force (kgf) RL = Right Lumbar; LL = Left Lumbar; ATM R = Right Anterior Tibial Muscle; ATM L = Left Anterior Tibial Muscle. * p = 0.028 in the comparison after the 1st and 10th session in RL in the group Placebo Acupuncture. Wilcoxon Matched Pairs test. ap = 0.026 in the comparison between the groups. Mann–Whitney test.
PPT decreased at the end of treatment at all points in the RA group and increased at all points in the PA group, but this difference was not statistically significant. Similarly, no significant difference was observed in the RA and PA groups before and after each daily treatment session. When comparing the RA and AP groups, no significant difference was found (p > 0.05) (Table 2).
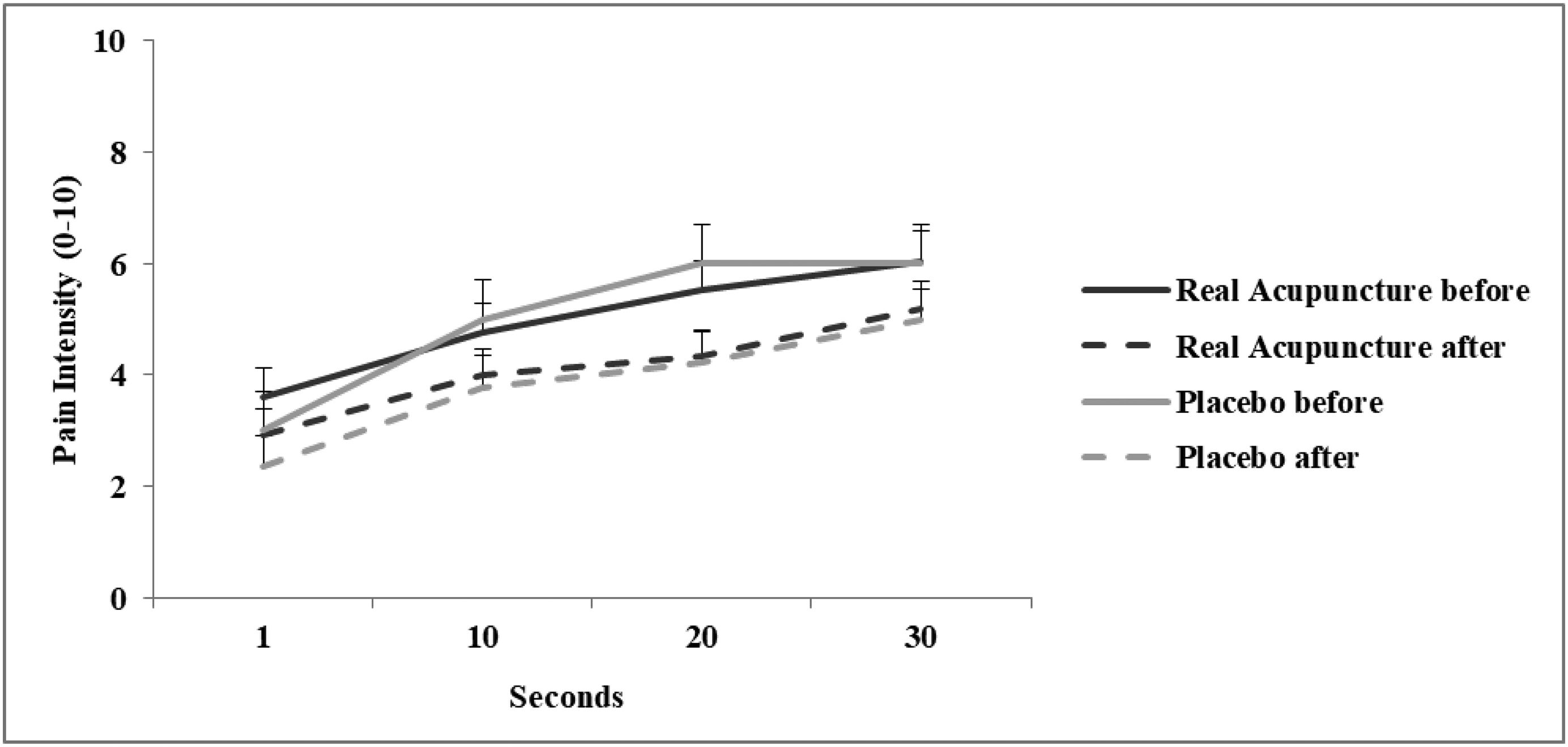
There was pain amplification (Fig. 4) over time during the temporal summation test in all groups before and after the proposed treatment (in the pre- and post-treatment RA group, p = 0.001, and p = 0.050, respectively; Pre-treatment AP, p = 0.001 and post-treatment, p = 0.001).
Pain intensity in sequential times (1, 10, 20 and 30 s) for temporal summation measurement in the groups Real Acupuncture and Placebo Acupuncture in patients with non-specific chronic low back pain over time before (RA: p = 0.001; AP: 0.001) and after (AR: p = 0.050; AP: 0.001) treatment. After 10 sessions RA and PA (p > 0.05). RA x PA (p > 0.05). Paired t-test and t-test for independent samples.
In the Conditioned Pain Modulation test (Fig. 5), there was a significant increase in pressure pain threshold (PPT) in the AR group only after the 10th session during ischemic compression (p = 0.047). In the AP group, the difference was also only after the end of the treatment, but PPT significantly reduced 5 min after the removal of compression (p = 0.047).
Pressure Pain Threshold in sequential times (before, during and after) for the measurement of conditioned pain modulation in patients with non-specific chronic low back pain. * p = 0.047 Before x During in Real Acupuncture group. ** p = 0.047 Before x After in Placebo Acupuncture group. Paired t-test and t-test for independent samples.
In the functional aspects, muscle strength of the RA group did not change significantly. There was a significant difference in the impact of pain on functionality in the PA group before (12.18 ± 1.35) and after (9.84 ± 1.07) therapy, with significant difference (p = 0.015 *) (Fig. 6). However, functional disability was not significantly different in the RA group before (9.5 ± 1.28) and after (8.00 ± 1.21) (p = 0.053), and in the PA group before (9.56 ± 1.38) and after (8.07 ± 1.20) (p = 0.243) 10 sessions.
In the psychoemotional aspects, pain catastrophizing and kinesiophobia did not present statistically significant alterations after the 10 sessions neither in the RA group nor in the PA. And in the FABQ for physical activities and work, there was no significant difference in both groups after the end of the treatment. Regarding quality of life before the 1st and after the 10th treatment session, it was not significant difference in both the AR group and the AP group (p = 0.256).
DiscussionPain intensity decreased after each session, corroborating other study, that both acupuncture and placebo promote pain relief.21 And the PA group after the 10th treatment session improved the intensity of pain, perhaps this happened because the placebo effect is already part of the overall therapeutic effect22,23 suggesting, a strong influence of the placebo effect.24,25
The group treated with Real Acupuncture did not present a decrease in pain intensity even after 10 treatment sessions, perhaps this happened because it was only 10 sessions and acupuncture performs a therapy through expulsion of pain, where pain reduction occurs throughout treatment sessions, not in one session alone,26 this makes more therapy sessions necessary, especially when considering chronic pain. This may also have happened because acupuncture is not usually the only method of treatment for chronic pain; it serves as complementary therapy, acting in conjunction with medications or other techniques, such as exercise, manual therapy, among others.1 However, in the study by Haake et al. (2007),1 it was observed that only 25% of patients who received conventional therapy (physical therapy and medication) responded to treatment and those who received acupuncture showed superiority in pain reduction and decrease in drug intake.
This does not mean that acupuncture is not effective for the treatment of low back pain, but it may not be sufficient when applied alone for this type of pain, because it is a pain with mechanical characteristics, such as, compensation in joint, fascia and muscle tissue, and local peripheral alteration in the structures of the lumbar region, not only neurophysiological characteristics. So, it is necessary to add other therapies that mobilize and strengthen the entire region to obtain positive results in the symptomatic treatment of this disease.1,27
NPE decreased after 10 sessions in both the RA group and the PA group, since the DCI decreased only in the RA group between the 1st and 10th sessions, this means that the patients improved their perception of how to classify their pain. This may be related to the fact that the questionnaire presents several words to characterize pain, causing the patient to decrease his or her limitation to describe the pain sensation in the best possible way, classifying it more accurately.28
The CST found in the acupuncture points are lower when compared to regions outside the points, however, studies show that after application of acupuncture, it is possible to increase the CST at the stimulated point, thus indicating that there is greater tolerance to pain in the region of the acupuncture points.27 This result is divergent from the present study, since no change in cutaneous sensitivity was identified in any of the treated groups.
People with chronic low back pain have lower PPT in the lumbar region and in the ATM.28 The decrease in PPT in both the primary and secondary pain area in individuals with low back pain has been shown in the literature,29 suggesting the existence of secondary hyperalgesia in people with chronic low back pain. There are already studies that point to altered central processing in people with chronic low back pain, but this still needs to be better clarified,18 this fact was not observed in the present study in which there was no change in PPT in any of the treated groups.
TS and CPM did not change in this study, perhaps this happened because 10 acupuncture sessions were not sufficient to centrally desensitize the patient with low back pain. In the study by Corrêa (2015),26 PPT and CPM were investigated in chronic pain and there are already involved neurological factors affected, regardless of the intensity of pain, CNS excitability is an important phenomenon that is observed.
After a careful search in the literature, regarding studies investigating the effects of acupuncture on chronic non-specific low back pain, no reports related to primary and secondary hyperalgesia were found. However, due to the chronicity of the disease, it is necessary to investigate primary and secondary hyperalgesia, since they refer to the phenomena of peripheral and central sensitization, respectively.
No studies were found showing that acupuncture has a primary effect on movement, but study showed improved movement as a side effect.4 For this reason, perhaps if in the present study the pain was reduced when comparing session 1 with session 10 in the treated group, the function would probably improve as a secondary outcome, again showing the need for multimodal therapies that work the mechanical characteristic of pain.
The stimulation of acupuncture points acts directly on the neurophysiological processes that improve pain, producing the release of peptides, substance P, bradykinins and proteolytic enzymes that increase local blood supply, causing analgesia, and consequently optimizing function, as verified in the study of Cherkin et al. (2009),20 showing an improvement of 60% in the real and simulated acupuncture groups compared to usual care in eight weeks of treatment through the Rolland Morris scale differently from the findings of the present study. This emphasizes that clinical trials need greater methodological rigor,4 because it does not in fact justify the patient improving his function through acupuncture treatment alone.
Another study has shown that the light touch of the skin can stimulate mechanoreceptors that induce release of substances such as serotonin, which in turn relieve pain.29 Therefore, Real Acupuncture may not be superior to Placebo Acupuncture for pain relief, a fact that raises questions about the likelihood of sham treatments actually serving as inactive controls and on the mechanism of action of acupuncture.20
Maciel et al. (2016)10 analyzed 321 healthy subjects divided into seven groups of different Placebo Acupuncture methods and noted that all methods proposed in this study were equally effective and none of the placebo methods presented benefits in comparison to the other. Thus, it is noted that further study on the application of the placebo method may be necessary, because in the current study, the placebo used may also have stimulated mechanoreceptors at the time of puncture, thus relieving pain.
The quality of life also did not change in both groups, this is also reported in the Whynes study (2013)30 who observed through EQ-5D in patients with low back pain treated with epidural steroid injection who had less response than specific pain measurement instruments, and the difference with other tools arises from the lack of rigor of graduating severity and variation to use the tool.
A multimodal approach may be necessary, since chronic non-specific low back pain has several dimensions, because it is a chronic pain, so it is not possible to credit to a single treatment the competence or ability from a neurobiological technical point of view to modify all these parameters, all these variables.
In the present study, acupuncture in the treatment of non-specific chronic low back pain in the RA group decreased pain intensity after each session, NWC and PCI in pain measurement. However, there was no evidence of improvement in sensory tests, other functional aspects, psychoemotional aspects and quality of life. In the PA group, pain intensity decreased after each session, before the 1st and after the 10th session at both rest and during movement and also decreased NWC, and in the functional aspects there was a decrease in the impact of the pain in functionality.
FundingThis clinical trial received a grant from the National Council for Technological and Scientific Development (CNPQ): Chamada MCTI/CNPq/MS - SCTIE - Decit N° 07/2013 - Política Nacional de Práticas Integrativas e Complementares (PICS) no Sistema Único de Saúde.
We would like to thank the National Council for Technological and Scientific Development (CNPQ) and the Foundation to support research and technological innovation in the state of Sergipe (FAPITEC) for supporting the authors.
*The complete protocol of our study and its data can be accessed through the website: www.ensaiosclinicos.com.br.