The aim of the present exploratory work was to investigate if acupuncture objectively improves xerostomia and if results are sufficiently relevant to perform further studies.
Material and methodsA preliminary clinical study, randomized, non-blinded and controlled with a waiting list was designed. The initial sample of the study consisted of 33 patients with malignant neoplasia in the head and neck area, submitted to RT treatment between October 2014 and May 2015 in the Radiotherapy Service of Centro Hospitalar do Porto at Oporto (Portugal). After applying inclusion/exclusion criteria the final patient's sample consisted of 18 patients randomized in two groups (experimental and control groups). The experimental group (EG) was submitted to 8 acupuncture sessions. The control group (CG) consisted of patients of the “waiting list”. All patients were subjected to the sialometry and modified Schimer tests. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, Core Module (QLQ-C30) and Head and Neck Module (QLQ-H&N35) were also used.
ResultsThere was a statistically significant increase in the amount of saliva (p < 0.001) and an increase in salivary flow, without stimulation (p = 0.001) and with stimulation (p = 0.011), when comparing experimental and control group. There was also an improvement in the “dry mouth sensation” in EG (p = 0.03) and a tendency to improve symptoms associated with xerostomia in the EG.
ConclusionsDespite the methodological limitations, our study suggests that the acupuncture treatment used can objectively increase salivary production (flow and quantity) and improve the quality of life of the patients. There were not detected side effects associated with acupuncture. These results are sufficiently relevant to perform further studies.
El objetivo de este estudio exploratorio fue investigar si la acupuntura mejora objetivamente la xerostomía, y si los resultados son suficientemente relevantes para realizar estudios futuros.
Material y MétodosSe diseñó un estudio clínico preliminar, aleatorizado, no ciego y controlado con lista de espera. La muestra del estudio inicial incluyó 33 pacientes con neoplasia maligna en el área de cabeza y cuello, sometido a tratamiento de RT entre octubre de 2014 y mayo de 2015 en el Servicio de Radioterapia del Centro Hospitalar do Porto de Oporto (Portugal). Tras aplicar los criterios de inclusión/exclusión la muestra final de pacientes incluyó 18 pacientes aleatorizados en dos grupos (experimental y control). El grupo experimental (GE) fue sometido a 8 sesiones de acupuntura. El grupo control (GC) incluyó pacientes de la “lista de espera”. A todos los pacientes se les realizaron pruebas de sialometría y de Schimer modificada. También se utilizaron los cuestionarios Core Module de QLQ-C30 de la European Organization for Research and Treatment of Cancer Quality of Life Questionnaire y QLQ-H&N35 (Head and Neck Module).
Resultadosse produjo un incremento estadísticamente significativo de la cantidad de saliva (p < 0,001) y un aumento del flujo salivar, sin estimulación (p = 0,001) y con estimulación (p = 0,011), al comparar los grupos experimental y control. También se produjo una mejora de la “sensación de boca seca” en el GE (p = 0,03) y una tendencia a mejorar los síntomas asociados a la xerostomía en el GE.
ConclusionesA pesar de las limitaciones metodológicas, nuestro estudio sugiere que el tratamiento de acupuntura utilizado puede incrementar objetivamente la producción salivar (flujo y cantidad) y mejorar la calidad de vida de los pacientes. No se detectaron efectos secundarios asociados a la acupuntura. Estos resultados son suficientemente relevantes para realizar estudios adicionales.
Head and neck malignant neoplasia represents a group of diseases with epidemiological, anatomical, and pathological features that require a multidisciplinary therapeutic approach. Surgery and radiotherapy (RT) are the standard practices, sometimes combined with chemotherapy regimens.1 With respect to radiotherapy, the effect of ionizing radiation results in a salivary flow reduction (salivary hypofunction) and, consequently, acute or chronic xerostomia.2 The functional changes of the parotid, and the impact on oral structures depend on the radiation dose and irradiated volume, with a rapid decrease in salivary flow rate observed during the first RT week.3 Brosky (2007) acquiesced that bilateral RT may result in reductions up to 80%, while unilateral RT results in a reduction of 50%–60%.4
Saliva is fundamental for oral health and general homeostasis with an important role in the digestive function and taste, moistures the oral mucosa, contributes to dental health, lubricates the mouth and provides oral protection.5,6 The antibacterial, antifungal and antiviral properties of saliva control the composition of the oral microflora, so, a reduced saliva secretion and the resulting xerostomia causes a significant morbidity in patients with head and neck cancer treated with RT, negatively interfering with the patients' quality of life and comfort.5
Current therapies for xerostomia consist of oral hygiene with fluoride, pilocarpine (alkaloid, cholinergic agonist), cevimeline, amifostite (made hydrophilic), salivary substitutes (oral lubricants) or surgical transfer of the submandibular gland.7–9 Nevertheless, these palliative care products have several limitations: some can cause complications such as nausea and sweating, their effect is short and they do not have the protective effects of natural saliva.7 Due to the limitations of these therapies, complementary and alternative medicine (CAM) has become more popular among patients suffering from xerostomia.10,11 One of the most widely used CAM therapies is acupuncture. There are several hypotheses on how acupuncture works, namely sensory stimulation, causing local and distant release of neuropeptides, with involvement of the central and peripheral nervous system.12,13 Different studies suggest that acupuncture can be a cost-effective intervention in the management of a number of palliative symptoms in cancer patients.12,14 With respect to oral dryness, some studies of acupuncture found promising results.15–19
Therefore, the aim of the present exploratory work is to investigate if acupuncture objectively improves xerostomia and if results are sufficiently relevant to perform further studies.
Material and methodsSampleThe initial sample of the study consisted of 33 patients with malignant neoplasia in the head and neck area, submitted to RT treatment between October 2014 and May 2015 in the Radiotherapy Service of Centro Hospitalar do Porto at Oporto (Portugal). All the patients were individually invited to participate in the study. After a meeting with all the potential participants to a better explanation of the study, each participant signed the written informed consent. The enrollment and assignment were conducted by the research coordinator, with the support of the responsible of the Service.
Inclusion and exclusion criteria were based in those of Meng et al. and Garcia et al.17,20 Inclusion criteria were: age > 18 years; carcinoma in the head and neck area (NPC) and anatomically intact parotid and submandibular glands. Patients were excluded if they had a history of xerostomia; had suspected or confirmed physical closure of salivary gland ducts on either side; had known bleeding disorders and were taking heparin or warfarin; had contraindications for the use of acupuncture at any acupoints; had history of cerebrovascular accident or spinal cord injury; or had taken any drug or herbal medicine in the past 30 days that could affect salivary function, were planning to, or ended up taking such a substance during the study. From the initial sample, fifteen patients were excluded: 10 did not fulfill the inclusion criteria, 4 did not performed the tests and 1 did not complete all the acupuncture sessions. Thus, the final sample was constituted by 18 patients (13 males and 5 females). The mean age for the sample was 61.5 (minimum 33 and maximum 83 years) (see Table 1).
Characterization of the sample.
| Characteristics | Experimental Group(n = 9) | Control Group(n = 9) | P value | |
|---|---|---|---|---|
| Age (years) | Mean | 60,7 ± 5,9 (51–68) | 62,4 ± 15,2 (33–83) | 0,657 |
| Gender | Male | 7 (78%) | 6 (67%) | 0,609 |
| Female | 2 (22%) | 3 (33%) | ||
| Radiotherapy Technique | IMRT | 3 (33,3%) | 0 (0%) | 0,065 |
| 3D-CRT | 6 (66,7%) | 9 (100%) | ||
| Prescribed dosage (Gy) | 50 Gy | 2 (22,2%) | 2 (22,2%) | 0,488 |
| 56 Gy | 0 (0%) | 1 (11,1) | ||
| 58 Gy | 0 (0%) | 1 (11,1) | ||
| 60 Gy | 3 (33,3) | 2 (22,2%) | ||
| 70 Gy | 4 (44,4%) | 3 (33,3%) | ||
| Mean dosage in the left parotids (Gy) | Mean | 32,3 ± 6,9 Gy | 26,4 ± 13,0 Gy | 0,250 |
| Interval | 25 Gy – 43 Gy | 10,0 Gy – 50,0 Gy | ||
| Mean dosage in the right parotids (Gy) | Mean | 26,3 ± 12,5 Gy | 26,0 ± 10,2 Gy | 0,825 |
| Interval | 9,0 Gy – 42,0 Gy | 5,0 Gy – 36,0 Gy | ||
A preliminary clinical, randomized, controlled with waiting list and non-blinded study was conducted.
The research protocol was approved by the Ethics Committee of Centro Hopitalar do Porto of Oporto, Portugal (CES_29–15). All the participants were informed about the aims and procedures of the study and all the participants signed a written informed consent before data collection. The participants could refuse to participate in the study at any moment according to the Declaration of Helsinki Ethical Principles for Medical Research. The study was conducted following the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA).21
The patients of the final sample were randomized into two groups, experimental group (EG) (n = 9) and control group (CG) (“waiting list”) (n = 9) by means of the coin-flip method.
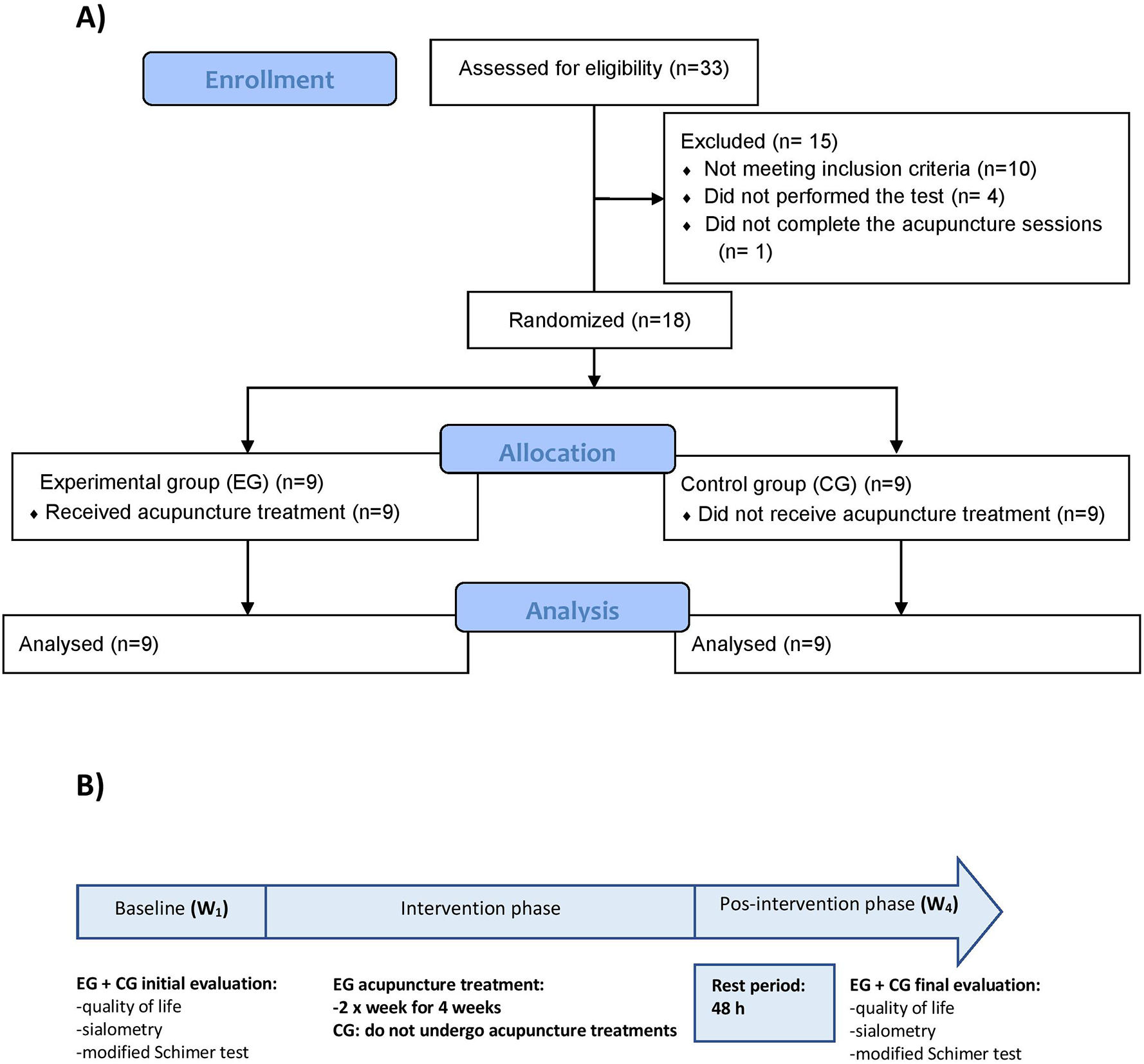
Fig. 1A shows the flow diagram for the selection of the sample and Fig. 1B shows the study design. At the baseline (W1), all the patients were evaluated with respect to quality-of-life parameters by means of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, Core Module (QLQ-C30) and Head and Neck Module (QLQ-H&N35). Also, sialometry and modified Schimer test were performed in order to obtain basal (pre-intervention) data to assess xerostomia. Thereafter, patients of the experimental group were submitted to 8 acupuncture sessions (2 times per week during 4 weeks). Control group consists of patients in a “waiting list”, so they do not undergo acupuncture treatments. After 4 weeks (W4), and after 48 h of the last treatment of patients of the EG, quality of life questionnaires, sialometry and modified Schimer test were performed again for both the experimental and the control group.
Radiotherapy protocolAll patients in this study were subjected to RT treatment (using photon energies: 6Mv), with daily doses of 2Gy/fraction from Monday to Friday over a period of 5 to 7 weeks with a total of 25 to 35 sessions, resulting in a prescription dose from 50Gy to 70Gy. Treatment field includes the lesion and surrounding tissues, as well as the parotid with medium doses exceeding 20Gy at least on one of them.
Study participants underwent a treatment of RT linear accelerators Clinac 600C Varian brand or Primus from Siemens in the RT Service of São João Hospital of Oporto (HSJ) with 3D-CRT (83,3%) and IMRT (16,7%) techniques. Irradiation of the parotid glands was performed according to QUANTEC - unilateral average dose exceeding 20 Gy.
Acupuncture protocolAcupuncture treatments were administered only by one acupuncturist. For the study a standardized acupuncture protocol was developed, based on Heidelberg model of Traditional Chinese Medicine22 with the support of the Institute of Biomedical Sciences Abel Salazar (Oporto, Portugal). This model, developed by Prof. Greten, unifies the contemporary medical-scientific knowledge with the concepts of different classical schools of Chinese Medicine.22
Only patients of the experimental group (EG) received acupuncture treatment. Acupuncture sessions were done at the RT Service of São João Hospital, began after the first saliva collection (W1) and was performed twice a week for a 4 weeks period, with a total of 8 sessions. Each session lasted 20 min. The acupuncture protocol includes points based on WHO definitions, anatomically located in the lower extremities: the stomach 44-ST44 point (Neiting); in the upper extremities, the large intestinal 2-LI2 point (Erjian); at the head, the stomach 6-ST6 point (Jiache) and Controlling Vessel 24-CV24 point (Chengjiang).
Disposable acupuncture needles 0.22x13mm, stainless steel and coated with silicon (Tewa®) were used for this intervention. Puncture depth was approximately 5 mm and needles were stimulated until the appearance of “De Qi”.
Saliva measurementsTwo tests were used for assessment of xerostomy: the modified Schimer test and sialometry.
The modified Schimer test consists in measuring mouth moisture (ml) using a band of Schimer with a millimetric scale of 0–35 mm (Schimer-Plus ®). Patients elevate the tongue towards the hard palate (so the band does not touch the tongue) and a Schimer band is placed vertically on the left or right side of the frenulum for 5 min.23 Saliva absorption by the band is measured and recorded in the first, second, third, and fifth minute. The patient is requested not to swallow the saliva during the test.
Sialometry is the functional evaluation of the salivary glands.7 The sialometry test is based on total saliva collection without and with salivary induction.24 The sialometry test at rest was performed using the method of passive flow25: the patient is instructed to expel saliva accumulated in the mouth every minute into a glass over a period of 6 min without swallowing saliva. The stimulated sialometry test was performed using something sweet to stimulate the saliva production. Once again, patients were asked to emit saliva to a glass every minute over a period of 6 min.
Quality of life questionnairesTo self-report of dry mouth symptoms and quality of life, two questionnaires of The European Organization for Research and Treatment of Cancer (EORTC) were used: the EORTC QLQ-C30 and the EORTC QLQ-H&N35, validated for head and neck cancer patients.26 CG group was assessed by the questionnaires at the baseline (W1) and four weeks later (W4). EG patients filled in the questionnaires before the first acupuncture treatment (W1) and 48 h after the eighth treatment (W4) (Fig. 1A).
The scores were calculated according to the EORTC manual. The mean scores are processed on a scale of 0 to 100. The high values obtained in the functional scales and overall quality of life represent, respectively, a better functional ability and quality of life, while the high scores on a scale of symptoms represent a high level of symptomatology and problems.
Statistical analysisStatistical analysis was performed using SPSS program (Statistical Package for Social Sciences) version 22.0 for Windows ©. Kolmogorov–Smirnov test was carried out as a normality test. We used the t-test for independent samples or the t-test for paired samples for normal distribution variables. The Mann–Whitney test for independent samples or the Wilcoxon test for paired samples were used for not normal distributed variables. In all tests, the value set as the significance level limit was 0,05.
ResultsSample characterizationTable 1 shows the characterization of the 18 patients of the sample. With respect to the localization of the neoplasia, 39% of the patients have malignant neoplasia of the larynx, 17% malignant neoplasia of the palate, 17% malignant neoplasia in the nasopharynx, 11% malignant neoplasia of the tonsils, 11% malignant neoplasia of the tongue and 5% malignant neoplasia in the hypopharynx. Comparison between EG and CG group at baseline showed no significant differences among the variables age, gender or RT prescribed.
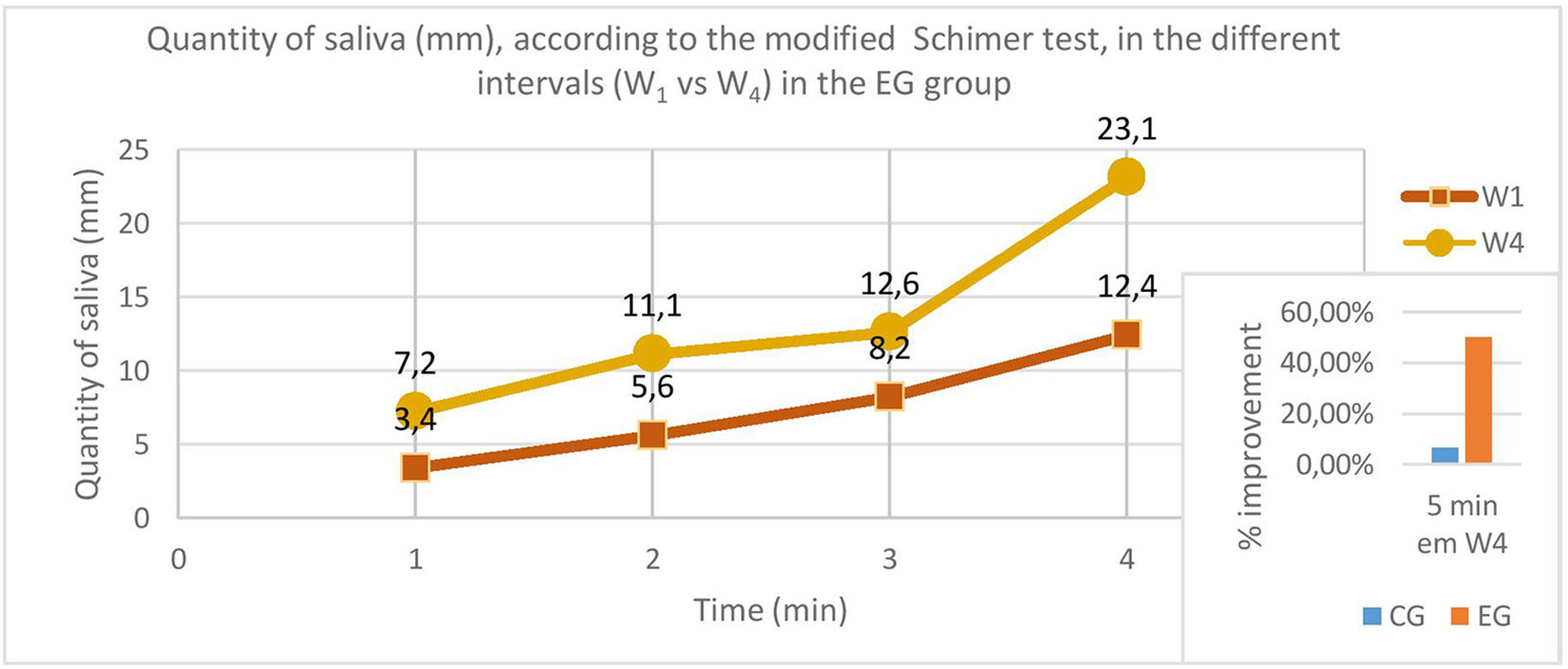
Analysis of the results obtained with objective measuresModified Schimer testWith respect to the modified Schimer test, at baseline (W1) there were no statistically significant differences comparing the CG and EG groups at first, second, third or fifth minute (p > 0,05 in all cases). However, statistically significant differences were found between CG and EG at W4, with a higher amount of saliva found in EG (average at 5 min of 23,1 ± 5,3 mm) compared with CG (mean of 11,6 ± 3,7 mm) (see Table 2). That is, patients receiving acupuncture produced 11,5 mm more saliva, what means an improvement of 49,8%.
Comparison of the quantity of saliva using a band of Schimer (mm), according to the modified Schimer test, between experimental and control groups at W1 and W4.
| Quantity of saliva (mm) | Experimental Group (n = 9) | Control Group (n = 9) | p-value | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| W1 | 1 min | 3,4 ± 1,0 | 2,8 ± 2,1 | 0,055 |
| 2 min | 5,6 ± 1,2 | 5,0 ± 2,4 | 0,079 | |
| 3 min | 8,2 ± 1,6 | 7,7 ± 3,4 | 0,658 | |
| 5 min | 12,4 ± 2,4 | 11,6 ± 3,8 | 0,562 | |
| W4 | 1 min | 7,2 ± 1,9 | 2,8 ± 1,7 | <0,001 |
| 2 min | 11,1 ± 3,3 | 5,1 ± 2,1 | <0,001 | |
| 3 min | 12,6/ ± 4,5 | 7,4 ± 3,1 | <0,001 | |
| 5 min | 23,1 ± 5,3 | 11,6 ± 3,7 | <0,001 | |
Similar results were found when we compared the intervals of assessment (Table 3 and Fig. 2). We observed a significant increase of the amount of saliva after 8 acupuncture sessions (W1 vs W4) in the EG group. The most relevant results were obtained at 5 min (12,4 mm vs 23,1 mm; p = 0,001) with an improvement of approximately 46,3%. Regarding the CG, there were no significant changes at the 5 min between W1 and W4 (11,6 ± 3,8 mm vs 11,6 ± 3,7; p = 1,0).
Comparison of the quantity of saliva, using a band of Schimer (mm), according to the modified Schimer test, between W1 and W4 in EG and CG groups.
| Quantity of saliva (mm) | Experimental Group (n = 9) | Control Group (n = 9) | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Min – Max (mm) | p-value | Mean ± SD | Min – Max (mm) | p-value | ||
| 1 min | W1 | 3,4 ± 1,0 | 2,0 – 5,0 | <0,001 | 2,8 ± 2,1 | 1.0–8,0 | 1000 |
| W4 | 7,2 ± 1,9 | 5,0–10,0 | 2,8 ± 1,7 | 1,0 – 7,0 | |||
| 2 min | W1 | 5,6 ± 1,2 | 3,0 – 7,0 | 0,002 | 5,0 ± 2,4 | 3,0–11,0 | 0,681 |
| W4 | 11,1 ± 3,3 | 7,0–15,0 | 5,1 ± 2,1 | 3,0–10,0 | |||
| 3 min | W1 | 8,2 ± 1,6 | 5,0–10,0 | 0,001 | 7,7 ± 3,4 | 5,0–16,0 | 0,169 |
| W4 | 12,6 ± 4,5 | 10,0–23,0 | 7,4 ± 3,1 | 5,0–15,0 | |||
| 5 min | W1 | 12,4 ± 2,4 | 8,0–16,0 | 0,001 | 11,6 ± 3.8 | 8,0–21,0 | 1000 |
| W4 | 23,1 ± 5,3 | 17,0–33,0 | 11,6 ± 3,7 | 8,0–20,0 | |||
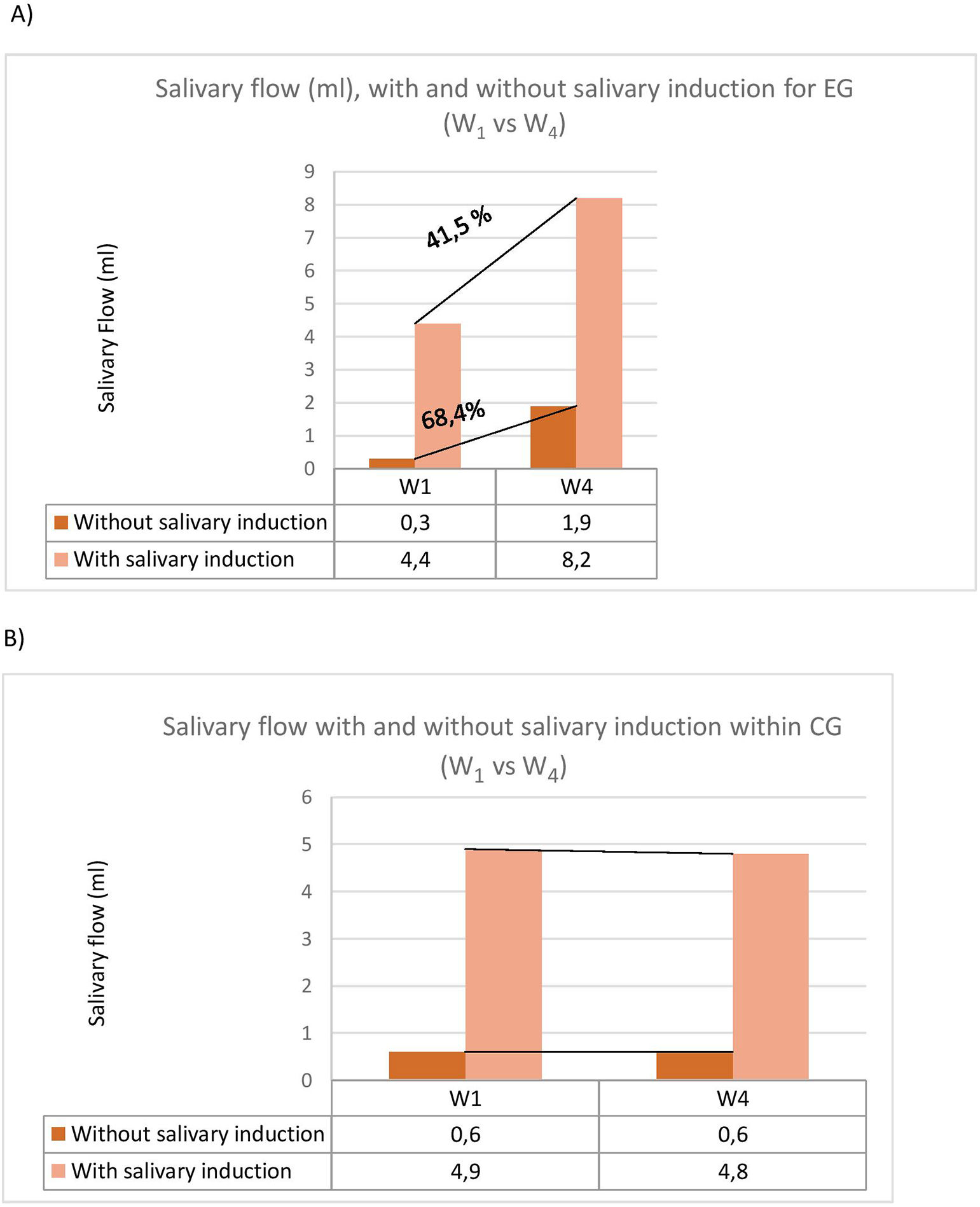
With respect to sialometry, we compared the results in salivary flow between W1 and W4, with and without stimulation, between groups and within each group. At W1, there were no statistically significant differences between the two groups, with or without stimulation (p = 0,3 and p = 0,642, respectively). Nevertheless, after 4 weeks assessment (W4), there was a statistically significant increase in saliva flow in EG compared to CG, both without salivary stimulation (1,9 ± 0,8 ml vs 0,6 ± 0,7 ml p = 0,001) and after salivary stimulation (8,2 ± 3,9 ml vs. 4,8 ± 1,1 ml, p = 0,011). (Table 4 and Fig. 3A and B).
Analysis of the salivary flow of the parotids (ml) – sialometry test between experimental and control groups at W1 and W4.
| Salivary flow of the parotids (ml) | Experimental Group (n = 9) | Control Group (n = 9) | p-value | |||
|---|---|---|---|---|---|---|
| Mean/ SD | Min – Max (ml) | Mean/ SD | Min – Max (ml) | |||
| W1 | Without stimulation | 0,3 ± 0,4 | 0,0 – 1,0 | 0,6 ± 0,7 | 0,0 – 2,2 | 0,352 |
| With stimulation | 4,4 ± 3,0 | 1,0–10,0 | 4,9 ± 1,6 | 2,8 – 7,0 | 0,642 | |
| W4 | Without stimulation | 1,9 ± 0,8 | 1,0 – 3,0 | 0,6 ± 0,7 | 0,0 – 2,0 | 0,001 |
| With stimulation | 8,2 ± 3,9 | 3,5 – 15,0 | 4,8 ± 1,1 | 3,0 – 6,0 | 0,011 | |
A) Salivary flow (ml), with and without salivary induction according to the sialometry test, at baseline and after 4 weeks within the experimental group. B) Salivary flow (ml), with and without salivary induction, according to the sialometry test, at baseline and after 4 weeks within the control group.
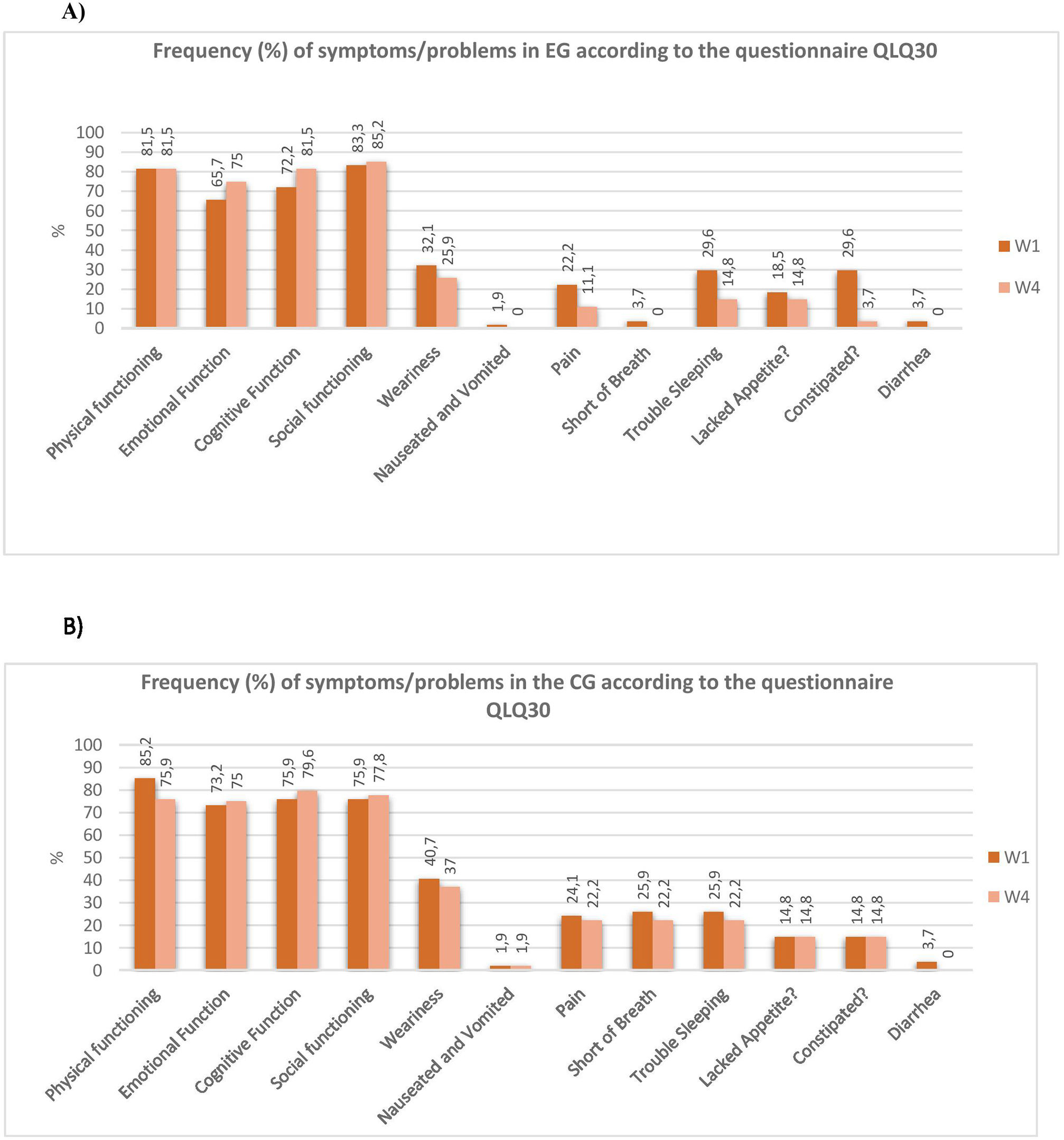
With respect to the QLQ-30 questionnaire, when we analyze the results of the EG group (W1 vs W4) we observed that there were no significant differences, although after 4 weeks of treatment it was observed improvements in the following items: “emotional function”, “cognitive function”, “social function”, “fatigue”, “nausea and vomiting”, “pain general”,”dyspnoea”, “loss of appetite”, “insomnia”, “constipation” and “diarrhea” (Fig. 4A). The results for the CG group did not show improvements for the analyzed items after four weeks (Fig. 4B).
When we compared the results between the experimental and control group in the evaluation of the questionnaire QLQ-30, at W4 there were significant differences between groups with respect to “dyspnea”, with EG experiencing less dyspnea than CG group (0,0 ± 0,0% vs 22,2 ± 28,9%). Although without statistically significant differences, we found improvements in the EG group for the following items: “cognitive function”, “social function”, “fatigue”, “nausea and vomiting”, “pain general “, “insomnia”, “constipation” and “diarrhea”.
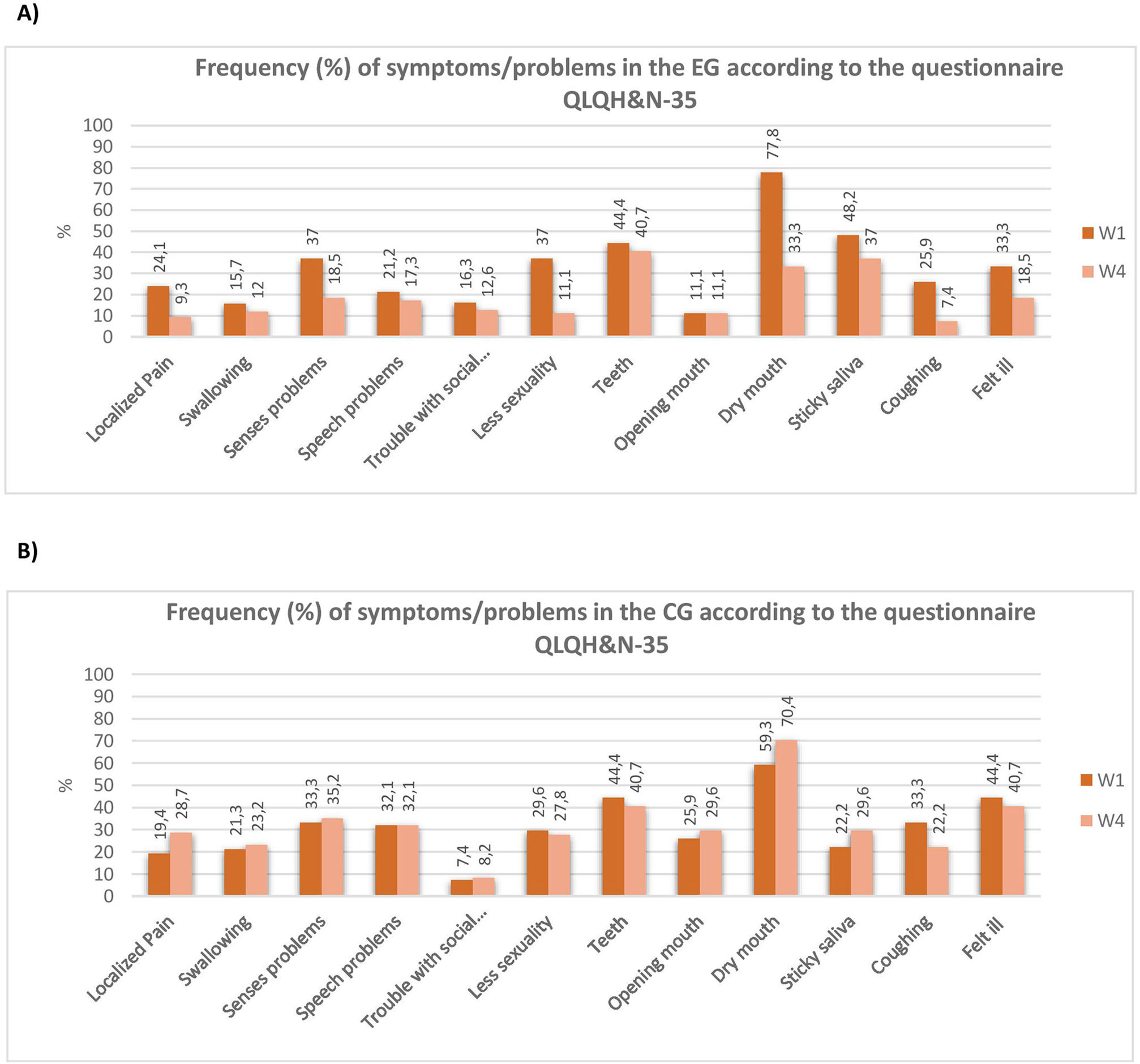
Questionnaire of quality of life of the patient with malignant neoplasia of the head and neck (EORTC – H&N35)Comparing W1 vs W4 for the EG, we observe a statistically significant improvement in the items: “dry mouth” (p = 0,002), “local pain” (p = 0,033) and “sexual activity” (p = 0,049) at W4. That means an improvement of 44,5% for the item “dry mouth” (77,8 ± 28,9 vs 33,3 ± 28,9), 14,8% for the item “local pain” (24,1 ± 21,0 vs 9,3 ± 11,4) and 25,9% for the item “sexual activity” (37,0 ± 28,6 vs 11,1 ± 23,6). The results also showed a trend in reducing symptoms, such as “swallowing”, “sensory problems”, “difficulty of speech”, “difficulty in establishing social contact”, “dental problems”, “sticky saliva”, “cough” (p = 0,059) and the “feeling of being sick” (Fig. 5A).
The CG showed no statistically significant differences after 4 weeks assessment (W1 vs W4), observing that some items even worsened: “local pain” (19,4 ± 21,3 vs 28,7 ± 31,5), “sensation of dry mouth” (59,3 ± 43,4 vs 70,4 ± 35,1) and “presence of sticky saliva” (22,2 ± 33,3 vs 29,6 ± 35,1) (Fig. 5B).
When we compared EG and CG, we found a statistically relevant improvement in the item “dry mouth” (33,3 ± 28,9% vs 70,4 ± 35,1%; p = 0,030), what means a 37,1% improvement of the xerostomia in the EG compared to CG. The remaining items showed no statistically significant difference. Nevertheless, an improvement of some symptoms such as “local pain”, the “ability to swallow”, the senses (taste and smell), “capacity to talk”, “sexual activity”, “difficulty opening the mouth”, “coughing” and “feeling sick”, was observed in EG. The CG showed no statistically significant differences after 4 weeks assessment (W4). We note that the item “problem in the teeth” maintained equal values for EG and CG (40,7 ± 22,2% vs 40,7 ± 43,4%, respectively).
DiscussionCholinergic signaling from parasympathetic nerves controls the secretion of saliva whilst the protein content of saliva is additionally depending on neuropeptides signaling and in parotid, submandibular and sublingual glands by sympathetic nerves and noradrenaline.27–29
Salivary glands are highly susceptible to radiation, with the parotid being the most sensitive.30 Radio-induced injuries modify the quantity, consistency and pH of saliva. These modifications represent an important impact on the quality of life of cancer patients. Some studies found that doses higher than 20Gy under the parotid can decrease salivary flow, and doses above 50Gy can lead to its dysfunction.30 Other studies also suggest that radiation induced damage in the acinar cells by lipid peroxidation, and hence the immediate lysis of the cells.31,32 In this sense, Konings et al. suggested two different mechanisms to explain the salivary gland dysfunction induced by radiation. The first mechanism was related with damage of selective membranes. The second mechanism explained the delayed effects by the cell death of progenitor cells and stem cells, thereby inhibiting cell renewal.33,34
Progress in RT techniques (3D CRT, IMRT) allow a better conformation of the target, avoiding the irradiation of a larger volume of surrounding tissue. In spite of these significant progress, to date, it is still not possible to prevent XIR in all patients submitted to RT.31,35 Vergeer et al.36 found that xerostomia (grade 2 -RTOG) was significantly lower after irradiation with IMRT compared with 3D - CRT. In our study, only 3 patients used the IMRT technique so it is not possible to consider the RT technique a variable to study.
With respect to palliative products to manage salivary gland hypofunction induced by radiation therapy, although significant advances, they still only offer partial protection, or potentially have significant adverse effects.7,37,38
Several studies suggested that acupuncture reliefs XIR.15–17,19,23,39–45 For example, a study by Simcock et al. comparing the use of acupuncture (6 sessions) vs oral hygiene education (2 sessions) found a significant improvement in reducing the sensation of dry mouth in the patient's perspective.42 Also, Mengh et al. verifies that manual acupuncture during RT treatment decreases XIR from week 3 for up to 6 months after the end of RT and also observes a significant increase in unstimulated salivary flow vs stimulated salivary flow at week 3, at week 7 and week 11 and at 6 months.17
The mechanisms underlying acupuncture are not clear. Bloom et al.46 suggested that tissue surrounding parotid glands experienced a significant increase in local blood flux after acupuncture. It was proposed that certain acupuncture points can directly stimulate the nerves that innervate the salivary glands.47 Deng et al. showed through functional magnetic resonance imaging (FMR), the activation of bilateral insula and adjacent operculum with the unilateral use of LI-2 acupuncture point in 20 volunteers with xerostomia. Although the meaning of this activation was not explained, it illustrates a biological effect of this point. Another possibility is that acupuncture acts inducing the increase in salivary flow through interaction of components of the neuronal salivation network, or increases Ca2+ cytosolic level.48,49 Another hypothesis is that the needle insertion into the skin may stimulate peptidergic parasympathetic fibers, which induce vasodilatation and stimulates fluid secretion.50,51 Also, we cannot rule out a possible placebo effect.
Although different clinical studies and systematic reviews suggested a possible positive effect of acupuncture treatment of patients with XIR, the results are still limited, with considerable heterogeneities in the acupuncture treatment protocols and results obtained.18,19,52 At present, more studies are needed to support the use of acupuncture as evidence-based treatment option to treat patients with symptoms of oral dryness.
With respect to the present study, our results point out a beneficial effect of acupuncture treatment in relief xerostomia, however, they should be interpreted with caution due to the inherent methodological limitations:
- -
Firstly, we observed that patients performing acupuncture (EG) showed an objectively decrease in XIR, measured by the amount of saliva present in the oral cavity and the production of salivary flow. In fact, in the EG we observed an increase of 49,8% of the amount of saliva in the mouth after 5 min, an increase of 68,4% of salivary flow without stimulation and 41,5% of salivary flow with stimulation. However, since the control group consisted of “waiting list”, the question is whether the effects of acupuncture are due to physiological effects or patient expectations. In this sense, from the perspective of patients (reviewed questionnaires), the feeling of dry mouth significantly decreases in the EG compared to CG and within EG between W1 vs W4, which appears to suggest a specific effect of acupuncture.
- -
Secondly, as far as quality of life is concerned, our study revealed statistically significant differences within the EG when compared W1 vs W4 in the items: dyspnea, local pain and sexual activity. Additionally, in the same group, we observe a trend to decrease (though not statistically significant) some relevant symptoms in the treatment of xerostomia such as swallowing, speech, pain, dental problems and sticky saliva, and also other relevant items related to quality of life as cough, fatigue, insomnia, constipation, diarrhea, nausea and vomiting as well as sensory problems (taste and smell). Probably the size of the sample is limiting conclusive results.
- -
Thirdly, there were no side effects related to the practice of manual acupuncture during the time of the study (four weeks). These preliminary results suggest that our acupuncture protocol is feasible and safe for patients with head and neck cancer undertaking RT treatments. Again, the size of the sample should be enlarged to have conclusive results in terms of security of the treatment.
- -
In our opinion, the obtained results suggest that the protocol of acupuncture used in our study can have a specific effect in terms of reduction of xerostomia induced by radiotherapy. Nevertheless, being a preliminary study, findings should be interpreted in light of its limitations:
- -
The sample size can be pointed out as an important limitation of the study. For further studies, sample should be enlarged and the sample size calculation analysis should be done.
- -
More restrictive inclusion criteria with respect to localization of tumor, treatment modality, type of radiotherapy and radiation dose could be used to assure a more uniform characterization of clinical variables.
- -
The present study was non-blinded. Results evaluation was carried out by the researcher, which may induce an evaluation bias. Blinding of the participants, practitioners and outcome assessors will be important in further studies.
- -
The control group consisted of “waiting list”, therefore it was not possible to compare real acupuncture with sham acupuncture. Nevertheless, placebo-controlled trials in acupuncture remain controversial as identifying an adequate sham treatment is difficult.
- -
Our study evaluated the effect of a four weeks acupuncture treatment but the long-term effects were not evaluated.
We can conclude that, as also suggested by other recent studies,19 the results seem to be promising for a therapeutic action of acupuncture in XIR. Thus, despite of caution in interpreting the results because of the limitations, the study suggests that the acupuncture treatment used can reduce XIR, improve quality of life of the patients and minimize some of the side effects caused by RT.
A study of larger dimensions, double-blind, with long term acupuncture treatment and controlled by sham acupuncture will be needed to clarify the effects of acupuncture on XIR in patients subjected to RT treatment. Also, further studies are needed to understand the physiological action of acupuncture in xerostomia. If the benefit of acupuncture is well established, then this treatment is likely to be included in the therapeutic offers in addressing XIR and promoting the quality of life in patients with neoplasia of the head and neck.
Study outlineFlow chart of the preliminary clinical, randomized, controlled with waiting list and non-blinded study, according to CONSORT statements.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Authors thank Prof. H J Greten, for the scientific support given to the study and the Centro Hospitalar do Porto and Abel Salazar Institute for Biomedical Sciences for hosting the study.