Korean acupuncture comes from the far-eastern tradition and has unique approaches to acupuncture point selection.
ObjectivesThere are several types of acupuncture methods. Among these, Tae-Geuk acupuncture and Saam acupuncture adopt five phase characteristics, using five vital points. Cho-sun acupuncture regulates Qi using acupunctures and meridians according to the flow of Qi. In this project, the effects of Korean Tae-Geuk acupuncture on chronic tension-type headache (TTH) were examined.
MethodsThis study is a randomized controlled study involving sham acupuncture (placebo acupuncture), and everything is clear except for the data processing phase. The purpose of the study; was to measure the safety and efficacy of Korean Tae-Geuk acupuncture in patients with chronic TTH. Groups used; acupunture + traditional pharmacological therapy, traditional pharmacological therapy only and placebo korean acupuncture + traditional pharmacological therapy groups. Seven treatment sessions were applied over a four-week period. Changes in pain and quality of life and side effects were examined during treatment and within 3 months after the completion of treatment. Results were evaluated by using the visual analog scale for pain and pain log records.
ResultsKorean Tae-Geuk acupuncture is a more effective treatment than placebo and traditional pharmacological treatment in chronic TTH. Korea Tae-Geuk acupuncture showed significant improvement in clinically chronic TTH during treatment and in 3 months follow-up after treatment.
ConclusionTae-Geuk acupuncture is a treatment branch of Sasang Constitution Medicine. Acupuncture points do not change according to acupuncture practitioner or disease.
la acupuntura coreana proviene de la tradición del Lejano Oriente y tiene enfoques únicos para la selección de puntos de acupuntura.
ObjetivosExisten varios tipos de métodos de acupuntura. Entre estos, la acupuntura Tae-Geuk y la acupuntura Saam adoptan características de cinco fases, utilizando cinco puntos vitales. La acupuntura Cho-sun regula el Qi utilizando acupunturas y meridianos de acuerdo con el flujo de Qi. En este proyecto, se examinaron los efectos de la acupuntura coreana Tae-Geuk sobre la cefalea tensional crónica (TTH).
MétodosEste estudio es un estudio controlado aleatorio que involucra acupuntura simulada (acupuntura placebo), y todo está claro excepto por la fase de procesamiento de datos. El propósito del estudio; Fue medir la seguridad y eficacia de la acupuntura coreana Tae-Geuk en pacientes con CT crónica. Grupos utilizados; Acupuntura + terapia farmacológica tradicional, solo terapia farmacológica tradicional y grupos placebo de acupuntura coreana + terapia farmacológica tradicional. Se aplicaron siete sesiones de tratamiento durante un período de cuatro semanas. Se examinaron los cambios en el dolor y la calidad de vida y los efectos secundarios durante el tratamiento y dentro de los tres meses posteriores a la finalización del tratamiento. Los resultados se evaluaron mediante el uso de la escala analógica visual para los registros de dolor y los registros de dolor.
ResultadosLa acupuntura coreana Tae-Geuk es un tratamiento más eficaz que el placebo y el tratamiento tradicional en la CT crónica. La acupuntura Tae-Geuk de Corea mostró una mejora significativa en la CT clínicamente crónica durante el tratamiento y en el seguimiento de 3 meses después del tratamiento.
Conclusiónla acupuntura Tae-Geuk es una rama de tratamiento de la Medicina de la Constitución de Sasang. Los puntos de acupuntura no cambian según el médico o la enfermedad de acupuntura.
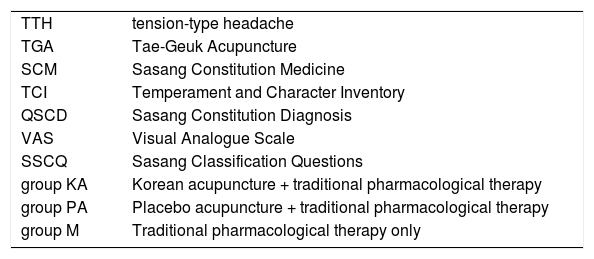
| TTH | tension-type headache |
| TGA | Tae-Geuk Acupuncture |
| SCM | Sasang Constitution Medicine |
| TCI | Temperament and Character Inventory |
| QSCD | Sasang Constitution Diagnosis |
| VAS | Visual Analogue Scale |
| SSCQ | Sasang Classification Questions |
| group KA | Korean acupuncture + traditional pharmacological therapy |
| group PA | Placebo acupuncture + traditional pharmacological therapy |
| group M | Traditional pharmacological therapy only |
Spanish summary
IntroductionThe most common type of primary headaches is tension-type headaches (TTH). The lifetime prevalence of TTH varies between 30 and 78% in studies. It is more common in women than in men.1 Although it is such a common medical condition, an effective and adequate treatment approach based on evidence has not been developed to date. This can be explained by the fact that the pain is mild in nature and patients find self-treating methods. However, when the pain returns into migraine or chronic daily headache, a more serious treatment need arises. 4% of the general population suffers from chronic headaches. In the classification made by the International Headache Society, the diagnostic criteria determined by the ICHD 2013 beta version are presented below.
Episodic tension-type headache diagnostic criteria (IHS 2013 beta version)A. There are at least 10 pain attacks that complement the features in A, B and D, and the sum of painful days is more than 1 or in a month, but less than 15 days, or more 15 or more but less than 180 days in a year.
B. Headache attacks last between half an hour and 7 days.
C. The presence of at least two of the following pain characteristics:
1. With bilateral localization.
2. It has a blunt (not throbbing) character in the form of pressure–compression–weight.
3. Mild or moderate severity.
4. Pain that does not increase with daily activities such as walking.
D. The presence of two of the following:
1. Pain is not accompanied by nausea and vomiting (may be anorexia).
2. No more than one of photophobia or phonophobia.
E. No underlying systemic or neurological disorders.
Chronic tension-type headache diagnostic criteria (IHS 2013 beta version)A. Pain that complements the features in B and D lasting for at least 15 days or more, and continues for 3 months or more (more than 180 days).
B. Headache attacks persist between hours and days or continue continuously.
C. The presence of at least two of the following pain characteristics:
1. With bilateral localization.
2. In a blunt (not throbbing) character in the form of pressure–compression–weight.
3. Mild or moderate severity
4. Pain that does not increase with daily activities such as walking.
D. The presence of two of the following:
1. Pain is not accompanied by nausea and vomiting (may be anorexia).
2. No more than one of photophobia or phonophobia.
E. No underlying systemic or neurological disorders.
The physiopathology of TTH is not fully known. While peripheral pain mechanisms are effective in common or rare TTH, central sensitization plays an important role in TTH.2 The data obtained indicate that there is increased sensitivity and inadequacy/weakness in the extensor neck and shoulder muscles in TTH, and also increased sensitivity is associated with the frequency and severity of headache.3
TTH treatments can be divided into pharmacologically and non-pharmacologically. Pharmacological treatments are applied as acute-symptomatic and chronic-prophylactic. If episodic tension type headache is in question and the pains are rare/mild, only treatment for pain should be arranged. If chronic tension type headache is in question or if the number of painful days is frequent, then preventive–prophylactic treatment should be initiated in addition to treatment for pain. Chronic GTBA; is often accompanied by stress, depression or anxiety disorders. Medication treatments include amitriptyline, gabapentin, onabotulinumtoxin A, propranolol, topiramate, mirtazapine and venlafaxine. The drug treatments used have both a large cost and side-effect profile. Recurrence rates are also high at the end of treatment.4,5 Non-drug approaches used in TTH are summarized below.
Non-drug approaches- •
Information about the disease,
- •
Regulation of lifestyle,
- •
Regular sleep and nutrition,
- •
Exercise,
- •
Relaxation techniques,
- •
Rearrangement of posture,
- •
Awareness and avoidance of triggers,
- •
Biofeedback,
- •
Cognitive-behavioral treatments,
- •
Psychological support, anxiety relief,
- •
Physiotherapy,
- •
Acupuncture,
- •
Homeopathy,
- •
Ozone therapy.
Many studies have shown the short-term effects of acupuncture in various physiological variables related to analgesia.6,7,8 However, it is unclear how relevant these observations in experimental settings are to the long-term effects reported by doctors. Spinal, supraspinal mechanisms and cortical, psychological or placebo mechanisms, which are a variable combination of peripheral effects, are assumed to have an impact on clinical effects in routine treatment.9 As a result of stimulation with acupuncture treatment; various neurotransmitters (endorphins, monoamines and cortisone) have been shown to be secreted in the brain.10,11 Acupuncture creates analgesia by stimulating neural structures, activating the spinal cord stimulation pathways and many centers in the brain (spinal cord, midbrain and hypothalamus–pituitary axis).12 Again, some randomized controlled studied show that this treatment may be as effective as and more effective than medication in headache, especially migraine.13
Sasang Constitution Medicine (SCM) was developed by Korean physician Lee Jema (1837–1900).14 According to Sasang structural medicine, people are divided into four groups according to their congenital pathophysiological predisposition and treated according to these groups. These groups are divided according to temperament structure, behavior patterns, physical properties and bio-psychological characteristics.15–19
The feature of these groups
- 1-
Taeyang (Sadnes: Strong Lung/ Weak Liver) Creative, positive, progressive, impressive, brave, hasty mind.
- 2-
Soyang (Anger: Strong Spleen / Weak Kidney) Indecisive, boring quickly with compromising, truthful, warm-tempered.
- 3-
Taeeum (Joy: Strong Liver / Weak Lung) A kind, professional, durable, humorous, coward, frightened mind
- 4-
Soeum (Pleasure: Strong Kidney / Weak Spleen) Elegant and moderate, negative, selfish, smart, organized and jealous.
SSM uses herbal and acupuncture treatment in the treatment of these four groups. One of the acupuncture treatments used is Korean Tae-Geuk Acupuncture (TGA). Korea TGA Acupuncture is a treatment option and applied firstly by Dr. in 1974 by Byunhaeng Lee. TGA uses acupuncture points specific to four groups.
The determination of the groups in the SSM is performed with some psychosocial tests. The most frequently used ones are Temperament and Character Inventory (TCI) are Questions for Sasang Constitution Diagnosis (QSCD), and Sasang Classification Questions (SSCQ).
Korean acupuncture is a form of treatment that has a certain treatment protocol compared to classical Chinese acupuncture and does not differ according to the acupuncture practitioner. This study is an original study designed to evaluate the effect of TGA, which is the Korean Acupuncture type, on pain, daily functions and quality of life in patients with chronic tension headache and to measure the level of reliability.
Materials and methodsStudy settingThe study was conducted in Istanbul Medipol Mega University Hospital and is a randomized controlled clinical trial. The effectiveness of TGA treatment was examined in patients with chronic tension headache. All examinations, statistical analyzes and patient appointment were carried out by impartial researchers.
Working Algorithm:
Stage 1: Determining the patients who meet the criteria from the patients who applied to the internal medicine, family medicine and neurology outpatient clinics.
Stage 2: Preliminary interview with the patients, informing about the study.
Stage 3: The patients who accepted the study were asked to read and sign the “consent form”.
Stage 4: Determining the groups of patients by the closed envelope method.
Stage 5: The treatment schedule of the patients selected for the acupuncture and sham acupuncture groups was determined.
Study populationA total of 129 patients with a tension headache were included in the study. Patients who had been diagnosed with chronic tension headache for at least 6 months among the patients who applied to Family Practice, Neurology and Internal Medicine Polyclinics in Medipol University Hospitals were included. A visit was arranged for all participants by the clinical research coordinator for preliminary evaluation. After the screening questions were completed, the participants filled in the informed patient consent form. The participants were divided into three groups.
- 1-
Korean Acupunture group (group KA); Korean acupuncture + traditional pharmacological therapy,
- 2-
Placebo Korean Acupuncture Group (group PA); Placebo acupuncture + traditional therapy,
- 3-
Traditional pharmacological treatment group (group M); Traditional pharmacological therapy only.
They were informed that they would be randomly directed to any of the three groups, and they were informed that they could leave at any stage of the treatment they voluntarily attend. Participants who met the following criteria were measured for tension-type headache by clinicians based on the ICHD 3 Beta (International classification of Headache Diseases) criteria. The eligible participants were divided into groups using the closed envelope method. After random grouping, the interviewer arranged the treatment sessions. All the procedures performed were recorded in the follow-up file.
Eligibility criteria1-18–65 years old,
2-Chronic tension type headache must be diagnosed definitively,
3-At least 6 months of illness,
4-Not being received acupuncture treatment before,
5-No comorbid disease that may cause headaches (hypertension, somatoform disorder, etc.),
6-There is no psychiatric illness or visual-hearing impairment that would hinder work.
Dismissal criteria1) Having a different pain problem that requires pain relief or anti-inflammatory,
2) Depression or any condition that prevents memory and critical analysis,
3) Acupuncture history or acupuncture point stimulation treatment in the last 3 months,
4) Any damage to the head or neck lately,
5) Failure to understand or reject the informed patient consent form,
6) Deformities that can prevent acupuncture in cervical vascular,
7) Hemorrhagic disorders or anticoagulant consumption,
8) Pregnancy,
9) Infection in acupuncture points,
10) Participation in any other clinical trial within one month of the screening date.
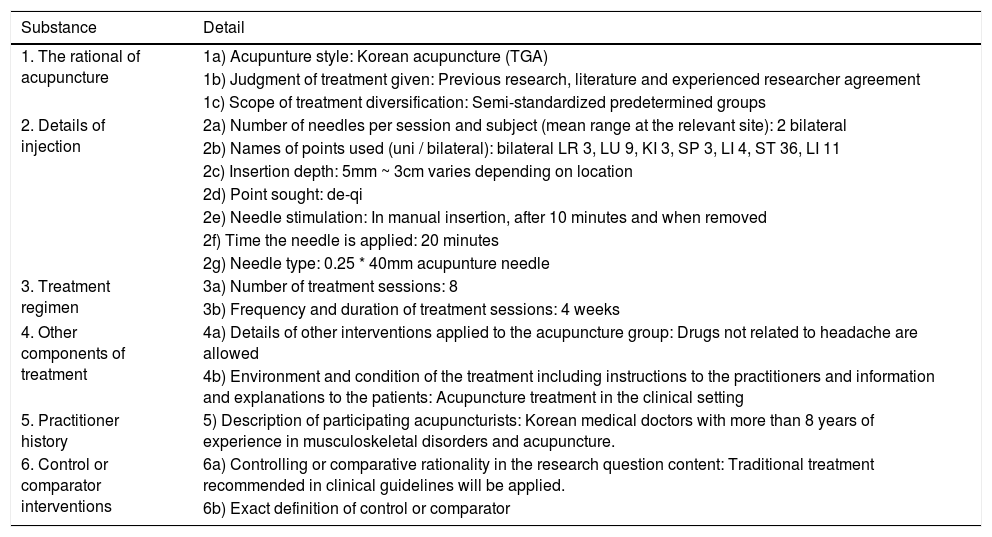
InterventionsThe group KA was treated according to a protocol of 8 sessions for 4 weeks, with Korean acupuncture and traditional pharmacological therapy. In the same way, 8 sessions for 4 weeks were applied to the group PA. During the trial period, all groups continued to be given traditional pharmacological therapy (antidepressant + analgesic therapy if needed (paracetamol, dexketoprofen trometamol ... etc)). Acupuncture treatment is detailed according to STRICTA (Intervention Reporting Standards in Acupuncture Clinical Trials) protocol in Table 1.
Treatment definition according to STRICTA protocol: Korean Acupuncture for tension-type headache.
| Substance | Detail |
|---|---|
| 1. The rational of acupuncture | 1a) Acupunture style: Korean acupuncture (TGA) |
| 1b) Judgment of treatment given: Previous research, literature and experienced researcher agreement | |
| 1c) Scope of treatment diversification: Semi-standardized predetermined groups | |
| 2. Details of injection | 2a) Number of needles per session and subject (mean range at the relevant site): 2 bilateral |
| 2b) Names of points used (uni / bilateral): bilateral LR 3, LU 9, KI 3, SP 3, LI 4, ST 36, LI 11 | |
| 2c) Insertion depth: 5mm ~ 3cm varies depending on location | |
| 2d) Point sought: de-qi | |
| 2e) Needle stimulation: In manual insertion, after 10 minutes and when removed | |
| 2f) Time the needle is applied: 20 minutes | |
| 2g) Needle type: 0.25 * 40mm acupunture needle | |
| 3. Treatment regimen | 3a) Number of treatment sessions: 8 |
| 3b) Frequency and duration of treatment sessions: 4 weeks | |
| 4. Other components of treatment | 4a) Details of other interventions applied to the acupuncture group: Drugs not related to headache are allowed |
| 4b) Environment and condition of the treatment including instructions to the practitioners and information and explanations to the patients: Acupuncture treatment in the clinical setting | |
| 5. Practitioner history | 5) Description of participating acupuncturists: Korean medical doctors with more than 8 years of experience in musculoskeletal disorders and acupuncture. |
| 6. Control or comparator interventions | 6a) Controlling or comparative rationality in the research question content: Traditional treatment recommended in clinical guidelines will be applied. |
| 6b) Exact definition of control or comparator |
Treatment was arranged according to TGA. The patients were divided into four groups according to their structure. Determination of the groups were made based on the Temperament and Character Inventory (TCI) form20 and the patients were filled in the TCI form. According to the results, the patients were divided into four structural groups: Taeyang, Taeeum, Soyang and Soeum. Disposable filiform acupuncture needles (0.25 * 40 mm) were used for acupuncture treatments.
The differences between the sets are at the distal acupuncture points. All patients were administered predetermined specific acupunctures such as at the bilateral midpoint (Set 1: Tae-Yang type) LR-3 (+), LU-9 (-); bilateral midpoint (Set 2: Tae-Eum type) LU-9 (+), LR-3 (-); bilateral midpoint (Set 3: So-Yang type) KI-3 (+), SP-3 (-); or t the bilateral midpoint (Set 4: So-Eum type) SP-3 (+), LI-4 (-).
All acupuncture treatments were performed in the Acupuncture treatment room at Medipol MEGA University Hospital Traditional and Complementary Medicine Research Center. Acupuncture treatment was performed after sterilization of the skin and in supine positions. The insertion depth varies according to the local anatomy and aims to reach de-qi. The sessions were held as 2 sessions each week and, if permitted, 3 sessions a week. It was planned to be at least 2 days between sessions in order not to cause planning problems in patients. Each session was determined as 20 minutes in duration. Manual stimulation was given 10 min after insertion and removal.
The traditional pharmacological treatments (antidepressant + if necessary analgesic treatment (paracetamol, dexketoprofen trometamol ... etc)) continued to be given to the patients during their treatment.
Placebo acupuncture groupIn this group, ear pin was applied to a parallel point 2 cm from the Korean acupuncture points determined according to the TCI survey. Patients will be convinced that korean acupuncture has been applied, the TCI Form has been filled in and sessions have been set as 2 sessions per week as in the Korean acupuncture group. The traditional pharmacological treatments (antidepressant + if necessary analgesic treatment (paracetamol, dexketoprofen trometamol ... etc)) the patients took continued to be given them.
Non-intrusive control groupIn this trial period, only traditional pharmacological medical treatment (antidepressant + analgesic treatment if necessary (paracetamol, dexketoprofen trometamol ... etc) was given during the trial period.
Patients were asked not to turn to treatments such as physiotherapy or massage for headaches outside the treatment protocol.
Permission of simultaneous treatment of patientsDuring the research period, all interventions, medications and treatments, except for the protocol, were prohibited. The use of normal medicines that were not intended to affect dysfunctions related to headaches was allowed. At each visit, all kinds of changes in simultaneous treatment were recorded. Results; Evaluated with VAS and Pain Log Records.
Visual analogue scale (VAS)Pain intensity and dysfunction severity of chronic tension-type headache was measured with 10 cm VAS, which is a reliable and accurate scale known for such purposes.1 Participants were asked to complete the VAS before the first session, in the 3rd, 5th and 7th sessions, at their visit 1 week after the end of treatment and 3 months after the end of treatment. The patients were asked to give information by evaluating them on a continuous scale from 0 to 10 (0, no pain or dysfunction; 10, worst pain or dysfunction imaginable).
Headache logPain diary record is a proven measurement tool used for measuring pain and daily functions in migraine and tension-type headaches. It is practical and provides a more detailed view of the real functions of the patient, as opposed to measuring only the pain of the patient. Pain diary records were evaluated at each visit of the patient.
All three groups were asked about possible side effects during and after treatment, and the answers were recorded in their files.
ResultsWhen we look at the general characteristics of the groups; KA Group (n: 40); From 22 female, 18 male patients. His age is 22, the sickest is 33, the youngest is 18. PA Group (n:41); It was taken from 23 female and 18 male patients. Age is 23, the patient is 32, the youngest is 18. Group M (n: 48); It was taken from 26 female and 22 male patients. Age is 25, the sickest is 34, the youngest is 18. In the KA Group, 2 patients had screening and 1 patient had fibromyalgia diagnoses. In the PA Group, one patient had chronicle and one patient was diagnosed with it. In Group M, 2 patients were diagnosed with psoriasis in one patient and fibromyalgia in one patient. There were no differences in age and chronicity between the groups.
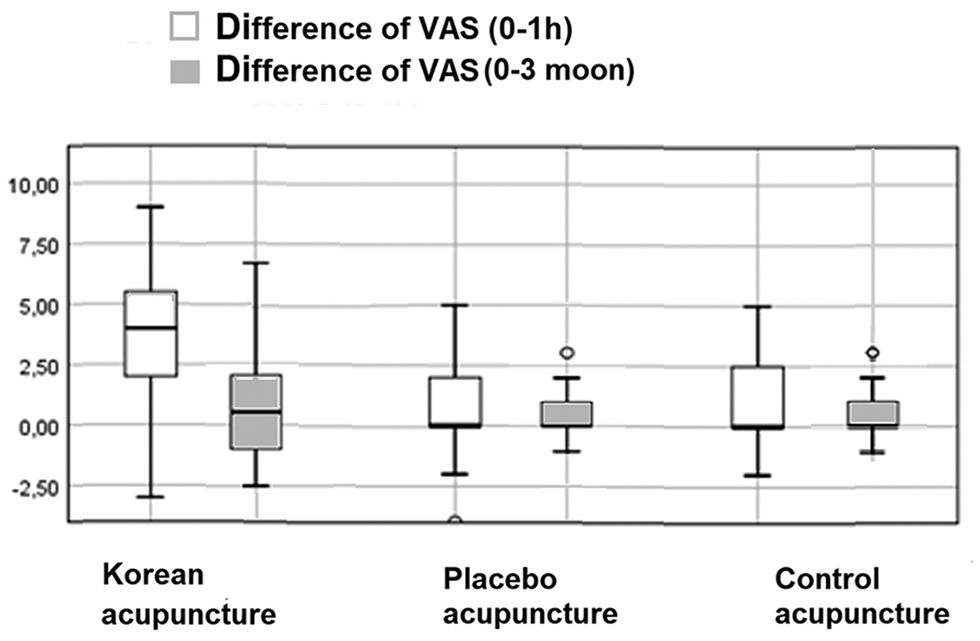
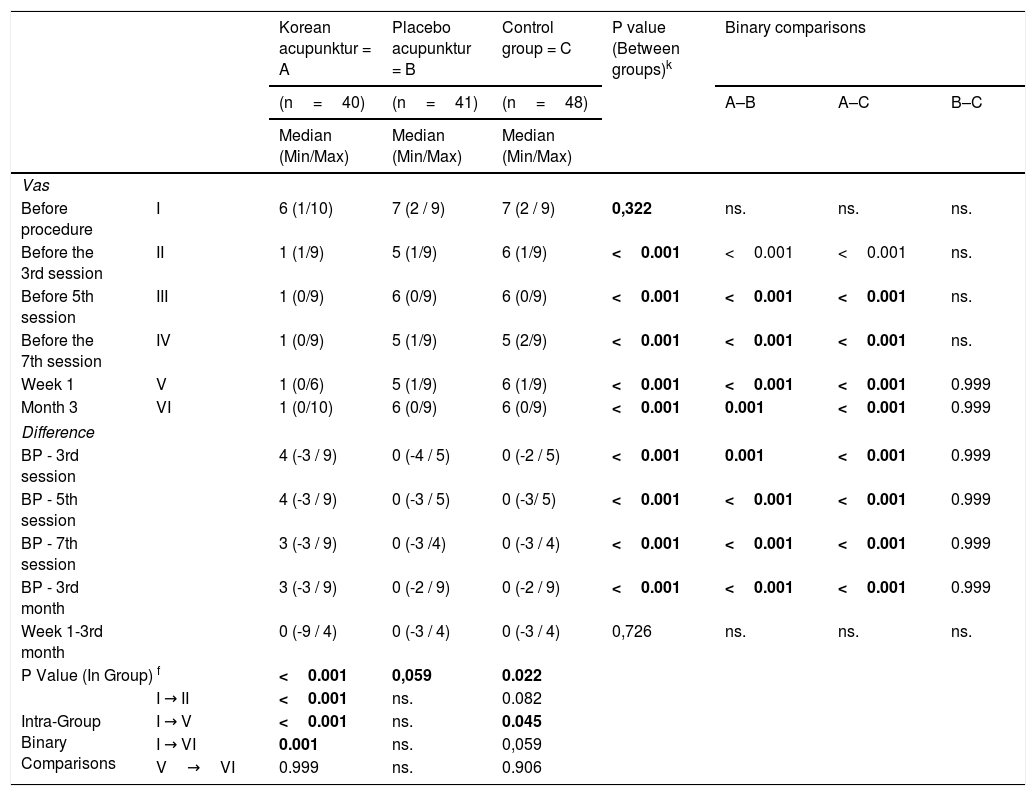
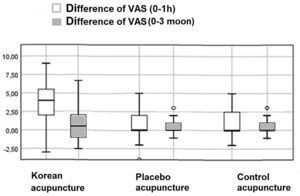
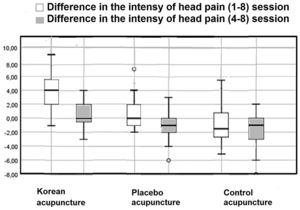
In this study, when we look at the effect of TGA on headache, there was no significant difference regarding VAS and Pain Intensity between the groups before the first session. In the KA group, Vas values decreased significantly before sessions 3, 5 and 7, 1 week after the end of treatment and 3 months after treatment compared to the other two groups (Table 2, Figs. 1, 2).
VAS value between groups.
| Korean acupunktur = A | Placebo acupunktur = B | Control group = C | P value (Between groups)k | Binary comparisons | ||||
|---|---|---|---|---|---|---|---|---|
| (n=40) | (n=41) | (n=48) | A–B | A–C | B–C | |||
| Median (Min/Max) | Median (Min/Max) | Median (Min/Max) | ||||||
| Vas | ||||||||
| Before procedure | I | 6 (1/10) | 7 (2 / 9) | 7 (2 / 9) | 0,322 | ns. | ns. | ns. |
| Before the 3rd session | II | 1 (1/9) | 5 (1/9) | 6 (1/9) | <0.001 | <0.001 | <0.001 | ns. |
| Before 5th session | III | 1 (0/9) | 6 (0/9) | 6 (0/9) | <0.001 | <0.001 | <0.001 | ns. |
| Before the 7th session | IV | 1 (0/9) | 5 (1/9) | 5 (2/9) | <0.001 | <0.001 | <0.001 | ns. |
| Week 1 | V | 1 (0/6) | 5 (1/9) | 6 (1/9) | <0.001 | <0.001 | <0.001 | 0.999 |
| Month 3 | VI | 1 (0/10) | 6 (0/9) | 6 (0/9) | <0.001 | 0.001 | <0.001 | 0.999 |
| Difference | ||||||||
| BP - 3rd session | 4 (-3 / 9) | 0 (-4 / 5) | 0 (-2 / 5) | <0.001 | 0.001 | <0.001 | 0.999 | |
| BP - 5th session | 4 (-3 / 9) | 0 (-3 / 5) | 0 (-3/ 5) | <0.001 | <0.001 | <0.001 | 0.999 | |
| BP - 7th session | 3 (-3 / 9) | 0 (-3 /4) | 0 (-3 / 4) | <0.001 | <0.001 | <0.001 | 0.999 | |
| BP - 3rd month | 3 (-3 / 9) | 0 (-2 / 9) | 0 (-2 / 9) | <0.001 | <0.001 | <0.001 | 0.999 | |
| Week 1-3rd month | 0 (-9 / 4) | 0 (-3 / 4) | 0 (-3 / 4) | 0,726 | ns. | ns. | ns. | |
| P Value (In Group) f | <0.001 | 0,059 | 0.022 | |||||
| I → II | <0.001 | ns. | 0.082 | |||||
| Intra-Group Binary Comparisons | I → V | <0.001 | ns. | 0.045 | ||||
| I → VI | 0.001 | ns. | 0,059 | |||||
| V→VI | 0.999 | ns. | 0.906 | |||||
fFriedman Test (Monte Carlo), kKruskal Wallis Test (Monte Carlo), Post Hoc Test: Dunn's Test, ns.: not significant, Min.:Minimum, Max.:Maximum.
VAS values were similar in the group KA 1 week after the end of the session and 3 months later. This result shows that Korean Acupuncture continues its effect 3 months after the end of treatment (Table 2).
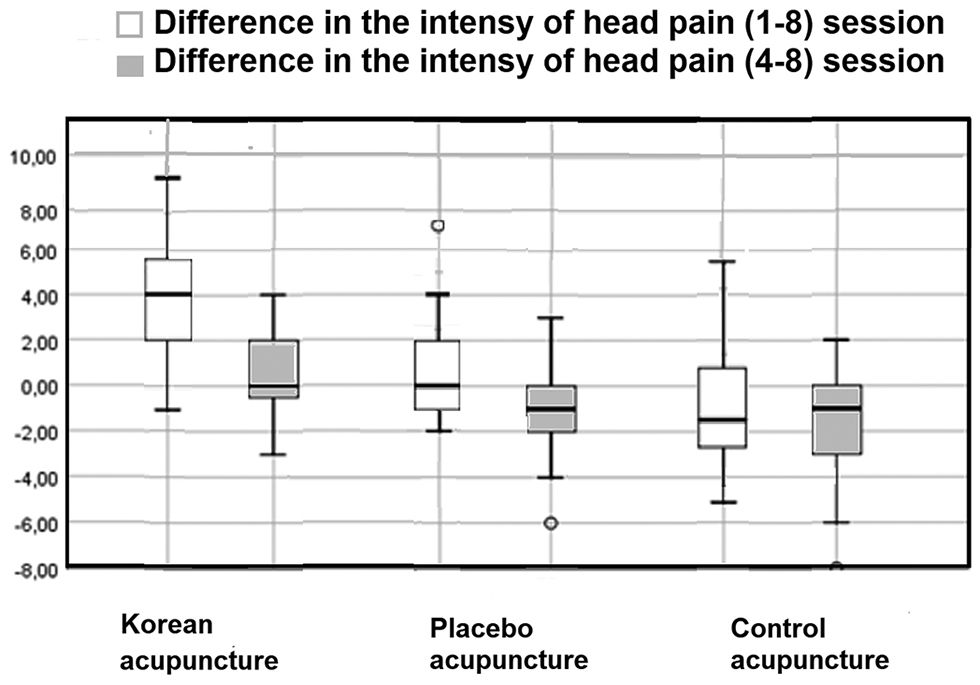
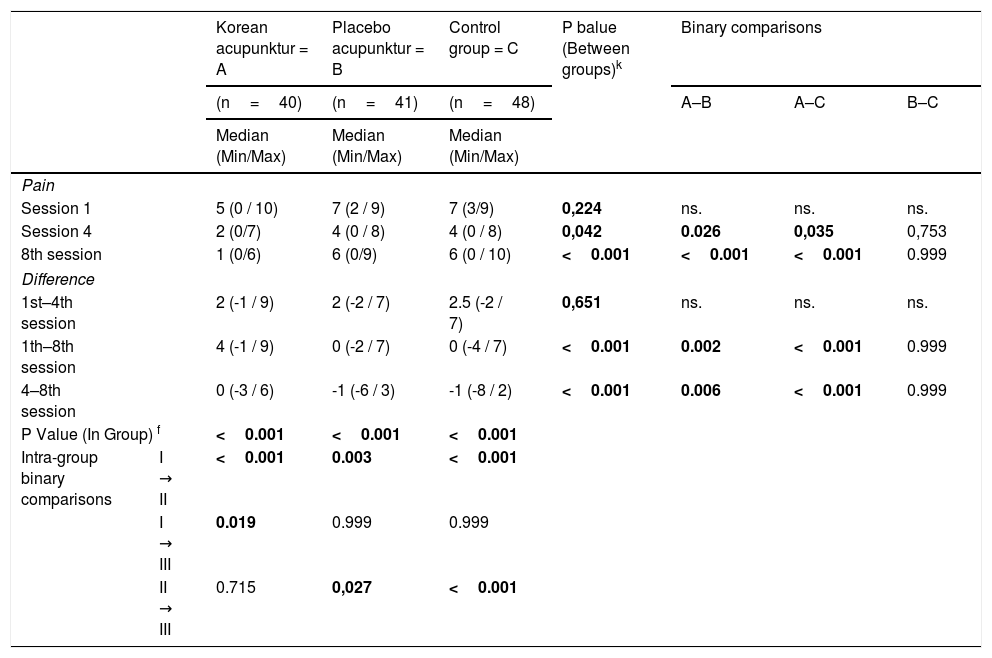
There was no significant difference between the groups regarding headache intensity before treatment, and there was a significant decrease in the group KA Headache Intensity Data, with respect to the headache intensity in the sesions 4 and 8 compared to the groups PA and M (Table 3, Fig. 2).
Headache Intensity value between groups.
| Korean acupunktur = A | Placebo acupunktur = B | Control group = C | P balue (Between groups)k | Binary comparisons | ||||
|---|---|---|---|---|---|---|---|---|
| (n=40) | (n=41) | (n=48) | A–B | A–C | B–C | |||
| Median (Min/Max) | Median (Min/Max) | Median (Min/Max) | ||||||
| Pain | ||||||||
| Session 1 | 5 (0 / 10) | 7 (2 / 9) | 7 (3/9) | 0,224 | ns. | ns. | ns. | |
| Session 4 | 2 (0/7) | 4 (0 / 8) | 4 (0 / 8) | 0,042 | 0.026 | 0,035 | 0,753 | |
| 8th session | 1 (0/6) | 6 (0/9) | 6 (0 / 10) | <0.001 | <0.001 | <0.001 | 0.999 | |
| Difference | ||||||||
| 1st–4th session | 2 (-1 / 9) | 2 (-2 / 7) | 2.5 (-2 / 7) | 0,651 | ns. | ns. | ns. | |
| 1th–8th session | 4 (-1 / 9) | 0 (-2 / 7) | 0 (-4 / 7) | <0.001 | 0.002 | <0.001 | 0.999 | |
| 4–8th session | 0 (-3 / 6) | -1 (-6 / 3) | -1 (-8 / 2) | <0.001 | 0.006 | <0.001 | 0.999 | |
| P Value (In Group) f | <0.001 | <0.001 | <0.001 | |||||
| Intra-group binary comparisons | I → II | <0.001 | 0.003 | <0.001 | ||||
| I → III | 0.019 | 0.999 | 0.999 | |||||
| II → III | 0.715 | 0,027 | <0.001 | |||||
f Friedman Test (Monte Carlo), k Kruskal Wallis Test (Monte Carlo), Post Hoc Test: Dunn's Test, ns.: not significant, Min.:Minimum, Max.:Maximum.
Also, there was no significant difference between groups PA and M regarding VAS value and Headache Intensity values during treatment and follow-up (Tables 2, 3).
FindingsData analysisSPSS 25.0 (IBM Corparation, Armonk, New York, United States) program was used in the analysis of variables. In comparing Vas and Pain scores between groups, Kruskal–Wallis H Test was used with Monte Carlo Simulation results, while Dunn's Test was used for Post Hoc analysis. Friedman's two-way test was used with Monte Carlo simulation results for comparison of the six and three repeated measurements of the vas score and pain score respectively with each other in the group and Dunn's test was used for Post Hoc analysis. Quantitative variables were shown as median (Minimum / Maximum) in the tables. Variables were examined at 95% confidence level and p value was considered as less than 0.05.
When data analysis is performed, in the group KA the vas values decreased significantly before the session 3, 5 and 7, 1 week after the end of treatment and 3 months later, compared to the other two groups (Table 2, Fig. 1).
When data analysis is performed, Vas values decreased significantly in the sessions of 3, 5 and 7 of the treatment in the KA group compared to the other two groups 1 week and 3 months after the end of the treatment (Table 2, Fig. 1).
VAS values were similar in the group KA 1 week after the end of the session and 3 months later. This result shows that Korean Acupuncture continues its effect 3 months after the end of treatment (Table 2).
There was no significant difference between the groups regarding headache intensity before treatment, and there was a significant decrease in the group KA Headache Intensity Data, with respect to the headache intensity in the sesions 4 and 8 compared to the groups PA and M (Table 3, Fig. 2).
Also, there was no significant difference between groups PA and M regarding VAS value and Headache Intensity values (Tables 2, 3).
On the other hand, no side effects were observed during the treatment and follow-up period in all three groups. No side effects were observed during the three-month period they spent at home after the treatment.
DiscussionThere are many studies showing that classical acupuncture is effective in tension-type headache, a chronic disease.6,7,8 However, it is unclear how relevant these observations are to the long-term effects reported by doctors. Spinal, supraspinal mechanisms and cortical, psychological or placebo mechanisms, which are a variable combination of peripheral effects, are assumed to have an impact on clinical effects in routine treatment.9 As a result of stimulation with acupuncture treatment; various neurotransmitters (endorphins, monoamines and cortisone) have been shown to be secreted in the brain.10,11 Acupuncture creates analgesia by stimulating neural structures, activating the spinal cord stimulation pathways and many centers in the brain (spinal cord, midbrain and hypothalamus-pituitary axis).12 Again, some randomized controlled studied show that this treatment may be as effective as and more effective than medication in headache, especially migraine.13
However, different acupuncture points were used in each of these studies and different levels of results were obtained.21–26 Although the main reason for this condition is that acupuncture treatment is specific to individual rather than disease, it weakens the hand of acupuncture against modern medicine with standardization. In addition, the treatment of acupuncture by adopting specific points of the person, is not an easy to apply treatment by acupuncturists and to be able to apply the right treatment requires being an experienced acupuncturist. Incorrect determination of acupuncture points or improper sorting of acupuncture points during treatment sessions will negatively affect the outcome of the treatment. On the other hand, calling the PA and KA groups for treatment twice a week seems to have a positive effect on patient treatment. Because group M patients were not called to control as frequently as the other two groups. This situation seems to be a negative situation for the M group.
According to SCM, people are treated according to their congenital pathophysiological predispositions. In SCM, people are divided into 4 groups. These groups are Taeyang, Taeeum, Soyang and Soeum. The groups are divided according to their temperament structure, patterns of behavior, physical characteristics and bio-psychological characteristics. Tae-Geuk Acupuncture treats these four groups, which are separated on the basis of SCM, with their own acupuncture points. TGA applies acupuncture therapy to these four groups, which are based on the main energy conflicts between the main organs.17,19,27
A review published in Cochrane in 2009 revealed that acupuncture is much more effective in episodic or chronic tension-type headache than imitation acupuncture.28 Acupuncture is an intervention used frequently to reduce the frequency and intensity of headaches. For example, according to a survey in the USA, 9.9% of people who use acupuncture use acupuncture to treat migraine or other headaches.29 According to a study performed in Turkey in 2004, only 4.5% of patients who applied to clinics for headaches used acupuncture for their treatment.30
ConclusionsTGA is a treatment branch of SCM. TGA is an easily applicable form of treatment. Acupuncture points do not change according to acupuncture practitioner or disease. More comprehensive studies to be performed on SCM and TGA will increase the interest of acupuncture practitioners in this treatment.
AuthorshipResearch concept and design; Serhat Koran, Eun Sang jeon
Writing the article; Serhat Koran, Burcu Polat Özge, Burcu Polat Özge
Critical revision of the article; Serhat Koran, Aydın Sarıhan
FundingThe author(s) received no financial support for the research, authorship, and/or publication of this article.
Availability of data and materialsData sharing: no additional date available.
Ethics statementsAll of the authors pledge to abide by “The World Medical Association Declaration of Helsinki Ethical Principles Regarding Medical Research in Humans”.
Informed consentAll the patients who accepted the study were asked to read and sign the “consent form”.
The authors thank to Istanbul Medipol University and healthcare professionals.