Peyronie's disease produces penile curvature that leads, in certain cases, to difficulties in having satisfactory sexual relations.
The objective of this study is to evaluate the functional and cost-effectiveness results obtained in the surgical treatment of penile curvature due to Peyronie's disease under local anesthesia, comparing them with those performed under a general–spinal anesthesia regimen.
Material and methodsTwo groups of patients undergoing corporoplasty are compared according to the type of anesthesia used. Group 1 consists of 32 patients who underwent major outpatient surgery and under local anesthesia from June 2016 to June 2019. Their data are collected prospectively. Group 2 consists of 30 patients who underwent surgery under general/spinal anesthesia with hospital admission, from January 2013 to December 2015, with their data collected retrospectively.
Anesthetic and surgical procedure, postoperative functional results, degree of satisfaction and hospital costs between both groups are analyzed, considering p≤0.05 as statistical significance and analyzing the results with the SPSS 20.0 program.
ResultsOf the 32 patients included in group 1, none required admission for intra or postoperative complications. In both groups, an improvement of the PDQ-test was observed without statistically significant differences, with the degree of global satisfaction above 95% in both groups. There were also no differences in the appearance of complications secondary to the anesthetic procedure or the hospital regime. We observed differences in hospital costs, being 44% lower for the group performed with local anesthesia.
ConclusionsSurgical treatment of penile curvature under local anesthesia improves the cost-effectiveness ratio with the same quality of care, degree of satisfaction and postoperative functional results, maintaining a similar rate of intra/postoperative complications. For this reason, we consider that corporoplasty can be successfully performed under local anesthesia.
La enfermedad de Peyronie produce una curvatura del pene que conduce, en ciertos casos, a dificultades para tener relaciones sexuales satisfactorias. El objetivo de este estudio es evaluar los resultados funcionales y de coste-efectividad obtenidos en el tratamiento quirúrgico de la curvatura peneana por enfermedad de Peyronie bajo anestesia local, comparándolos con los conseguidos bajo un régimen de anestesia general-raquídea.
Material y métodosSe comparan 2 grupos de pacientes sometidos a corporoplastia según el tipo de anestesia utilizada. El grupo 1 está formado por 32 pacientes que se sometieron a cirugía mayor ambulatoria y bajo anestesia local desde junio de 2016 a junio de 2019. Sus datos se recogen de forma prospectiva. El grupo 2 está formado por 30 pacientes intervenidos bajo anestesia general/raquídea con ingreso hospitalario, desde enero de 2013 hasta diciembre de 2015, con sus datos recogidos de forma retrospectiva. Se analiza el procedimiento anestésico y quirúrgico, los resultados funcionales postoperatorios, el grado de satisfacción y los costos hospitalarios entre ambos grupos, considerando p≤0,05 como significación estadística y analizando los resultados con el programa SPSS® 20.0.
ResultadosDe los 32 pacientes incluidos en el grupo 1, ninguno requirió ingreso por complicaciones intra o postoperatorias. En ambos grupos se observó una mejora en el test PDQ sin diferencias estadísticamente significativas, con un grado de satisfacción global superior al 95% en ambos grupos. Tampoco hubo diferencias en la aparición de complicaciones secundarias al procedimiento anestésico o al régimen hospitalario. Observamos diferencias en los costos hospitalarios, siendo un 44% menor para el grupo en el que se utilizó anestesia local.
ConclusionesEl tratamiento quirúrgico de la curvatura del pene bajo anestesia local mejora la relación coste-efectividad con la misma calidad asistencial, grado de satisfacción y resultados funcionales postoperatorios, manteniendo una tasa similar de complicaciones intra/postoperatorias. Por este motivo, consideramos que la corporoplastia se puede realizar con éxito bajo anestesia local.
Surgical treatment under local anesthesia is widely used in multiple surgical and medical–surgical specialties such as thoracic surgery, gynecology, or urology. Jointly the evidence has allowed the development of “Fast-Track” protocols for these specialties with the aim of improving postoperative recovery.1–5 These protocols combine pre, intra, and postoperative procedures that reduce surgical stress and improve postoperative results.6,7 Furthermore, these procedures generally present an advantage and improvement at a cost- effective level, reducing not only healthcare expenses but also minimizing the social and labor impact of surgery on patients.
Procedures under local anesthesia and under major outpatient surgery should coordinate concepts of patient education, new protocols for intra and postoperative analgesia, local anesthetic techniques and, of course, minimally invasive surgical techniques.8–13
The most effective surgical treatment for correction of penile curvature less than 60° is corporoplasty using plication techniques, which was initially described by Nesbit, and subsequently multiple variants emerged,14–16 which meet all the criteria to be considered a procedure to be performed through a major outpatient surgery program.8
Material and methodsComparative study of 62 patients divided into two groups: group 1 included the patients who underwent surgery between June 2016 and June 2019 using corporoplasty using plication techniques under local anesthesia and the major outpatient surgery regimen (n=32). Group 2 includes patients who underwent the same surgical technique, hospitalized and with general or spinal anesthesia (n=30) between January 2013 and December 2015. Data from the first group were collected prospectively, while the cases included in the second were retrospectively assessed.
Patients with penile curvature affected by Peyronie's Disease (PD) are included, ruling out those with penile curvature secondary to other causes such as congenital or the presence of hypospadias.
We analyze the type of corporoplasty technique used, the surgical-anesthetic risk (analyzed using the scale of the American Association of Anesthesiology), the degree and type of curvature using the method of self-photography in erection proposed by Kelami.17 The PDQ (Peyronie's Disease Questionnaire) test is also performed together with the visual analog scale (VAS), which is also taken into account to assess the overall satisfaction of the surgical procedure. Data collection is established in both groups using the medical history (anamnesis, physical examination and complementary tests such as the aforementioned questionnaires and digitized self-photographs, together with preoperative analytical studies, as well as prior anesthetic evaluation in the group of patients operated on by hospitalization-general or spinal anesthesia). In all cases, patients are informed of both the surgical and anesthetic procedures, signing the official informed consent for surgery and anesthesia. The pre-surgical preparation is performed at home by trimming the genital hair and taking anxiolytic with a moderate effect the night before (Bromacepan 3mg).
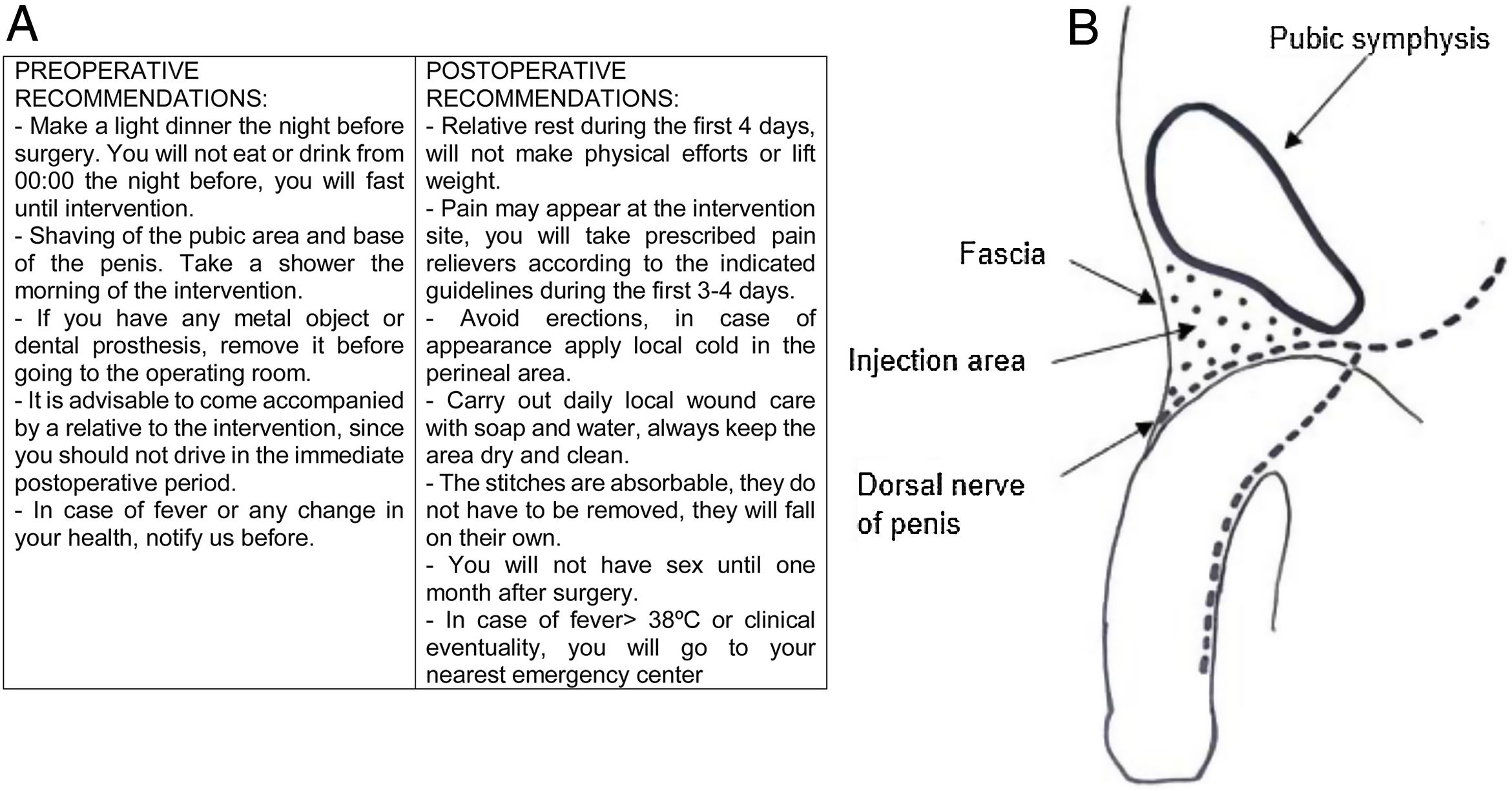
In addition, patients undergoing surgery on day-surgery regimen receive written information (Fig. 1A) on both preoperative and postoperative recommendations.
Regional or truncal anesthetic blockade using 10ml of Lidocaine 2% together with 10ml of Levobupivacaine 5mg/ml. Infiltration is performed at the dorsal level of the base of the penis and bilateral to the suspensory ligament of the penis, as well as in the deep ventral and paraurethral part looking for the bulbospongieux ventral innervation.
Subcoronal incision associated with circumcision along with degloving and Buck's fascia exposure. Placement of tourniquet on the penile base and intra corpus cavernosum saline infusion with maximum inflection point marking and penile plication using the 16-dot technique (19 patients) or modified Nesbit plication.13 In both techniques, a unilateral/bilateral longitudinal opening of the Buck's fascia is performed, exposing the tunica albuginea to avoid ostoperative complications-sequelae.
A non-absorbable Ti-Cron 3.0 braided suture is used to perform the plication, for the closure of the Buck's fascia and circumcision suture, a short absorbable braided suture is used (Vicryl rapid 3.0).
Finally, a compression bandage is placed to be removed in 24h by the primary care nurse. In no case is intraoperative bladder catheterization performed.
Since the surgery is considered clean, antibiotic prophylaxis is not administered.
After surgery, observation is performed in the first hour of the postoperative course, being discharged with the prescriptive recommendations outlined in a written report: analgesics (paracetamol 1g every 6h) alternated with non-steroidal anti-inflammatory drugs (Dexketoprofen 25mg every 8h). In addition, the recommendations for cleaning and healing the surgical wound are presented, requiring a cure by a primary care nurse after 24h. Patients are also instructed to avoid sexual activity in the first 6–8 weeks, as well as taking diazepam 5mg at night in case of powerful and painful nighttime erections.
The postoperative follow-ups are carried out on an outpatient basis with visits scheduled for the first month, 4th month, and 10th month after the surgery.
Among the patients undergoing surgery under hospitalization and general or spinal anesthesia, the 16-point technique was used in 17 patients and modified Nesbit plication in the remaining 13. In 22 patients, corporoplasty was performed under spinal anesthesia, while 8 patients required general anesthesia. All of them remained hospitalized for more than 24h, requiring antibiotic prophylaxis during anesthetic induction (Cefuroxime 1.5g IV single dose) and bladder catheterization for 24h.
Statistical analysis of the results is performed using the SPSS 20.0 statistical package (SPSS Inc. Chicago, IL), using t-Student considering p<0.05 statistically significant. The qualitative aspects of the study were compared using a Chi-square test.
ResultsBoth groups share similar characteristics in terms of age, anesthetic risk and etiology of the curvature, considering themselves comparable.
The mean time used for surgery in the group of patients operated under local anesthesia was 50±10min (35–70). Among those undergoing general anesthesia, it was 85±15min (50–105) (p<0.0005).
In group 2, the average hospital stay was 1.8±0.8 days.1–4
No outpatient operated under local anesthetic required admission for intra or postoperative complications. Two patients were treated in the emergency department for discomfort related to the bandage and a mild bruise resolved without requiring invasive treatment or hospitalization.
In five cases in group 1 (4 patients, 16-point technique – 1 patient, modified Nesbit plication), close follow-up was required for glacial hyperesthesia with difficulty in sexual intercourse (3 patients), penile neuropathic pain (1 patient) and recurrence of curvature. (1 patient). Overall, the mean follow-up of the group, until the final discharge is 11.37 months (range 10–24).
In both groups, an improvement of the PDQ-test was observed without significant differences, with an overall degree of satisfaction of 95% in both groups.
In relation to the surgical and hospital costs, the overall expense in the group of patients operated under local anesthesia and who did not require hospital admission was 67,904 Euros (2122 euros intervention of the patient under local anesthesia), while the group of patients operated with general anesthesia presents a global expense in relation to the surgical procedure and including hospitalization expenses (group III.1.1.341) of 179,517.3 Euros (5983.91 euros intervention–hospitalization of the patient under general anesthesia).18
DiscussionSurgical treatment of penile curvature caused by PD is indicated in patients with stable disease for 3 months and who have difficulties in maintaining satisfactory sexual relations due to curvature. The signs of disease stability are mainly the disappearance of pain and no increase in curvature. Some authors suggest waiting for surgical treatment for a period of 6–12 months after the disappearance of symptoms.19,20 Multiple corporoplasty procedures using plication techniques are performed on the healthy albuginea of the convex area of the penis. They are indicated when, in the absence of erectile dysfunction or significant penile deformity, the curvature is less than 60° in erection.21 Nesbit in 1965 initially described the excision of tunica albuginea ellipses on the opposite side to the curvature of congenital origin, and since 1979 it was used for the successful treatment of curvature secondary to PE.14,22 The Nesbit plication technique presents several variants with the intention of performing minimally invasive corporoplasties, outpatient surgical treatments, without major complications and presenting overall satisfactions similar to the Nesbit Plication technique in relation to penile correction, such as those used in our series of patients, described as a 16-point technique using non-absorbable sutures with minimal tension to reduce recurrence,23 and plication techniques without cleavage of the albuginea layer (modified Nesbit) in which the proximal and distal limits of the area to be applied, doing this by means of non- absorbable suture of three inverted points without needing to resect the albuginea.24 Both corporoplasty techniques are reproducible under local anesthesia in such a way that they reduce the morbidity derived from the general anesthetic act.
We prefer the use of Lidocaine and Levobupivacaine instead of other components given their low cardiotoxic effects (in case of accidental injection into the bloodstream). The dorsal truncal anesthetic block of the penis is a safe and effective procedure without being accompanied by motor block25 and that requires a series of essential items in our setting to carry it out:
- -
Acquire anatomical knowledge and references in relation to the area to be treated.
- -
Establish a peripheral venous catheter.
- -
Appropriate monitoring of the patient using blood pressure, electrocardiogram and pulse oximetry.
- -
Have anesthetic equipment for intubation and maintenance of the airway, as well as necessary medications for the management of any eventuality or complication.
- -
Preoperative medication
- -
Strict sterile technique.
The penis is innervated by the dorsal nerves that come from the genitocrural and minor abdominogenital nerve, emerging midway under the pubic symphysis and extending distally and laterally to the dorsal arteries of the penis along the internal aspect of Buck's fascia providing the sensory innervation of the glans and the distal two-thirds of the skin of the penis26,27 (Fig. 1B).
Regarding sutures used to perform the plication, in our case we used non-absorbable material in order to avoid recurrences (Ti-Cron 3.0), however; some articles suggest that there are no differences regarding the use of absorbable sutures in the plication, without visualizing an increase in complications or recurrences.28
The surgical techniques carried out for the correction of penile curvature due to PD have low morbidity. The most frequent complications are superficial hematomas (in some cases they may require surgical drainage), wound infections, and urinary retention (in the case of surgeries under general anesthesia). Other possible and less frequent are urethral perforation, urethral fistula and phimosis in patients who have had their foreskin preserved.
In our series, only a superficial penile hematoma was observed in one patient, which was resolved with conservative treatment and penile discomfort due to bandaging.
We do not consider post-surgical penile shortening as a complication, since it is inherent to the surgical technique, previously known and accepted by all the operated patients, regardless of the hospital regimen and the type of anesthesia used.
Therefore, we can conclude that there are no significant differences in the presence of postoperative complications in patients who underwent surgery under a major outpatient procedure and those who underwent general anesthesia.
The overall satisfaction obtained using the PDQ-test questionnaire was 95% in both study groups. After reviewing the series, overall satisfaction ranges from 76% to 100% overall, associated with penile rectification and improved sexual activity. We can say that both groups of studies show an overall satisfaction that is within the general values and that there are no significant differences in both groups.
ConclusionsCorrective and functional surgery continues to be the gold standard for the treatment of Peyronie's Disease. Plication techniques under local anesthesia in selected patients obtain a high degree of overall post-surgical satisfaction, with a lower rate of complications. In addition, compared to the hospital regimen, an improvement in the cost-effectiveness of the procedure is obtained.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been performed on humans or animals for this research.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors declare that they have no conflict of interest.