Although many patients are being treated by radical prostatectomy (RP), there is still insufficient information about the changes in long-term erectile function after RP. Our aim is to examine long term, up to 5 year erectile function status of patients after Radical Perineal Prostatectomy (RPP).
Materials and methodsOne hundred and thirty-two patients, who underwent bilateral nerve-sparing Radical Perineal Prostatectomy (RPP) in between January 2012 and January 2017, with preoperative age≤70, prostate volume<80g, transrectal ultrasound (TRUS) guided biopsy Gleason score (GS)<7, prostate specific antigen (PSA) value<10ng/mL, and cT stage≤2 (N0, M0) were included into this study. Exclusion criteria were previous cardiovascular diseases, serious chronic renal and/or hepatic insufficiency, neurological diseases, uncontrolled diabetes mellitus, and severe lung diseases. Patients who received additional treatment (hormonal and/or radiotherapy) after RPP were also excluded from the study group. Erectile function was evaluated before surgery and at postoperative 3rd, 12th, and 60th months. Patients with an “International Index of Erectile Function (IIEF) – 5” score of ≥21 and patients whose IIEF-5 scores were between 16 and 20 but responded as “yes” to the “Sexual Encounter Profile (SEP) – 2” and “SEP-3” questions were accepted as having normal erectile function.
ResultsOut of the 132 patients, 96 (72.7%) of the patients were found to be potent in the first postoperative year. A total of 118 patients were evaluated at the end of 5 years. Eighty seven (73.7%) patients had normal erectile function according to our criteria.
DiscussionAccording to the results of our study, short term and long term erectile function outcomes of patients undergoing RPP were favorable and there was no statistically significant difference between short and long term results.
Aunque muchos pacientes son tratados mediante prostatectomía radical (PR), existe poca información acerca de los cambios de la función eréctil a largo plazo tras una PR. Nuestro objetivo fue examinar el estatus de la función eréctil a largo plazo, de hasta cinco años, de los pacientes tras una prostatectomía radical perineal (PRP).
Materiales y métodosIncluimos en el presente estudio a ciento treinta y dos pacientes sometidos a PRP bilateral con preservación de nervios entre enero de 2012 y enero de 2017, con edad preoperatoria ≤ 70, volumen prostático <80g, puntuación de Gleason (GS) de biopsia transrectal ecoguiada (TRUS) (GS)<7, valor de antígenos específicos prostáticos (PSA) <10 ng/ml, y estadio cT ≤ 2 (N0, M0). Los criterios de exclusión fueron enfermedades cardiovasculares previas, insuficiencia renal crónica y/o hepática graves, enfermedades neurológicas, diabetes mellitus incontrolada, y enfermedades pulmonares graves. También se excluyó del grupo de estudio a los pacientes que recibieron tratamiento adicional (hormonal y/o radioterapia) tras PRP. La función eréctil fue evaluada antes de la cirugía y a los 3, 12 y 60 meses postoperatorios. Los pacientes cuya puntuación IIEF-5 (International Index of Erectile Function) fue≥21 y los pacientes cuyas puntuaciones IIEF-5 se situaron entre 16 y 20 pero respondieron “sí” a las preguntas SEP-2 (Sexual Encounter Profile) y SEP-3 fueron aceptados como pacientes con función eréctil normal.
ResultadosDe los 132 pacientes, 96 (72,7%) de ellos reflejaron potencia durante el primer año postoperatorio. Se evaluó a un total de 118 pacientes al cabo de cinco años. Ochenta y siete (73,7%) pacientes tuvieron función eréctil normal con arreglo a nuestros criterios.
DiscusiónEn virtud de los resultados de nuestro estudio, los resultados de la función eréctil a corto y largo plazo de los pacientes sometidos a PRP fueron favorables, no existiendo diferencia estadísticamente significativa entre los resultados a corto y largo plazo.
Prostate cancer is the most common cancer in men over 50 years of age and is the second leading cause of death from cancer.1 Radical prostatectomy (RP) is one of the gold standard treatment options for localized prostate cancer.2 RP operation can be performed through Retropubic or Perineal (RPP) approach which both of them may be open, laparoscopic or robotic. Regardless of the method; providing urinary continence, erectile function and cancer control, after surgery are the main goals.3
Urinary incontinence (UI) and erectile dysfunction (ED) are the most important morbidities affecting the postoperative life standards of the patients.4 Besides, in a study of Penson and colleagues, the erectile problem was identified as the most important independent factor that disturbs quality of life, out of the disease.5 Adverse effects of RP on erectile function have been documented in studies conducted over 20 years.6 Despite long-term clinical research and studies, inconsistency regarding the frequency of ED still remains.6 In many studies, it has been reported that erectile function is restored in 1–2 years after RP.6 With the presentation of anatomic RP by Walsh at the beginning of the 1980s and better understanding of prostate neuroanatomy over the last 20 years, postoperative patient well-being, in terms of continuity of erectile function, has increased.7 However, although the rate of ED after RP was reported to be 90–95% even in cohort studies of experienced centers, this value appears to be 20–30% in randomized controlled trials supported by penile rehabilitation.8,9
Sexual dysfunction is one of the most controversial aspects associated with radical prostatectomy. Anatomic studies have demonstrated additional nerve fibers running on the lateral surface of the prostate, distinct from the classically described dorsolateral “neurovascular bundles (NVB),” with a significant role in neural stimulation to the cavernous tissue. This NVY is also named Veil of Aphrodite because it covers almost pelvic floor. In the latest open or robotic techniques, the Veil of Aphrodite nerve-sparing technique became popular. Lately other related terms have emerged in the literature e.g., “high anterior release, “curtain dissection,” or “incremental nerve sparing. RPP is theoretically superior to other techniques, because Veil of Aphrodite is preserved by nature of RPP approach.
We perform different types of radical prostatectomy (RP) surgeries in our tertiary teaching hospital including all open or laparoscopic RP methods. Since we are one of the leading clinics performing RPP in our region and world, we believe that sharing our patients’ long-term results after RPP on erectile function will add valuable contribution to literature. Therefore, the aim of this study is to compare the erectile function status of patients after radical perineal prostatectomy (RPP) at the 1st and 5th postoperative years.
Materials and methodsOne hundred and thirty-two patients who underwent RPP in between January 2012 and January 2017 with preoperative age≤70, prostate volume<80g, transrectal ultrasound (TRUS) guided biopsy Gleason score (GS)<7, prostate specific antigen (PSA) value<10 ng/mL, and cT stage≤2 (N0, M0) were included into this study. These features mean that all patients had localized and low risk prostate cancer and were suitable to RPP. All surgeries were performed by the same high-volume surgeon. All patients’ erectile function was normal, preoperatively. Exclusion criteria were cardiovascular diseases, serious chronic renal and/or hepatic insufficiency, neurological diseases, uncontrolled diabetes mellitus, and severe lung diseases. Patients who received additional treatments (e.g. hormone and/or radiotherapy) before or after RPP were excluded from the study.
Erectile function was evaluated just before surgery and at postoperative 3rd, 12th, and 60th months. In addition to the patients with an “International Index of Erectile Function (IIEF) – 5” score of ≥ 21, patients with an ‘IIEF-5’ score between 16–20; but responding to the “Sexual Encounter Profile (SEP) – 2” and “SEP-3” question as yes were accepted as potent. Patients diagnosed with ED at the 3rd month after RPP were referred to penile rehabilitation and treated with different types of PDE5 inhibitors. When PDE5 inhibitors were ineffective, intracavernosal injection was administered twice a week (Papaverine 30mg/cc and Phentolamine 1mg/cc, max. 0.7cc/session).
Data were analyzed with Statistical Package for the Social Sciences software version 19 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were written with mean, standard deviation, lowest and highest values (range) and ratios. The distribution of variables was determined using the Kolmogorov–Smirnov test. Significance of parameters between groups was determined by univariate (Chi-square or t-test) tests. Statistical significance threshold was accepted as p<0.05 in all analyses.
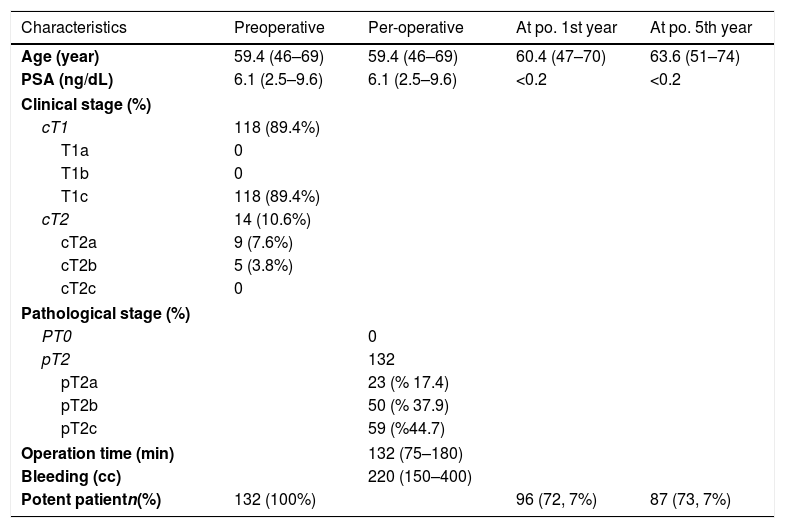
ResultsThe mean age of the patients undergone RPP was 59.4 years (46–69 years). Characteristics of the patients were summarized in Table 1. The mean preoperative PSA value was 6.1ng/dL.2,5,6–9 The mean prostate volume was 44cc (18–80).
Characteristics of the patients were summarized.
| Characteristics | Preoperative | Per-operative | At po. 1st year | At po. 5th year |
|---|---|---|---|---|
| Age (year) | 59.4 (46–69) | 59.4 (46–69) | 60.4 (47–70) | 63.6 (51–74) |
| PSA (ng/dL) | 6.1 (2.5–9.6) | 6.1 (2.5–9.6) | <0.2 | <0.2 |
| Clinical stage (%) | ||||
| cT1 | 118 (89.4%) | |||
| T1a | 0 | |||
| T1b | 0 | |||
| T1c | 118 (89.4%) | |||
| cT2 | 14 (10.6%) | |||
| cT2a | 9 (7.6%) | |||
| cT2b | 5 (3.8%) | |||
| cT2c | 0 | |||
| Pathological stage (%) | ||||
| PT0 | 0 | |||
| pT2 | 132 | |||
| pT2a | 23 (% 17.4) | |||
| pT2b | 50 (% 37.9) | |||
| pT2c | 59 (%44.7) | |||
| Operation time (min) | 132 (75–180) | |||
| Bleeding (cc) | 220 (150–400) | |||
| Potent patientn(%) | 132 (100%) | 96 (72, 7%) | 87 (73, 7%) | |
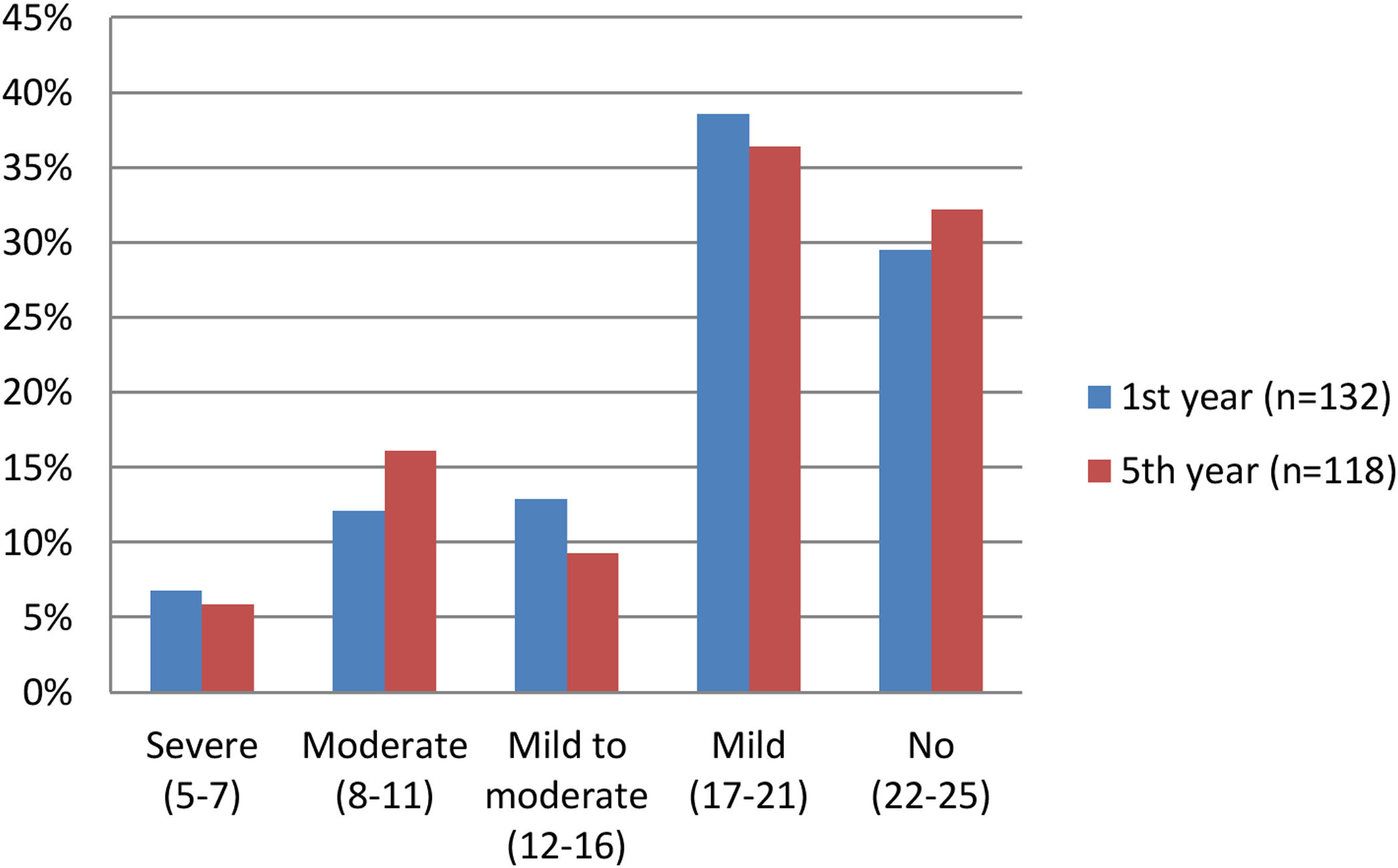
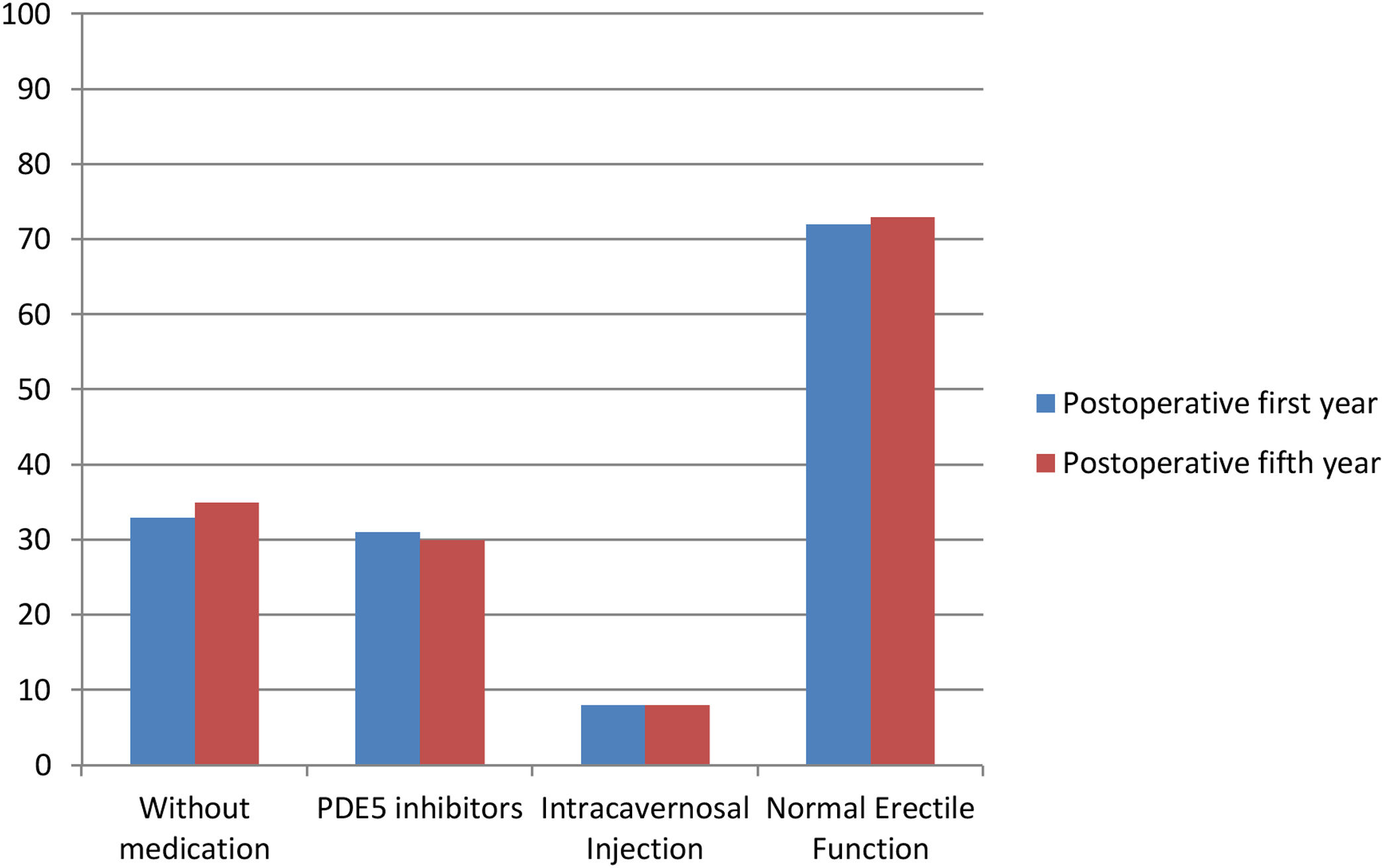
Of the 132 patients who underwent RPP, 96 (72.7%) were found to be potent at the end of first postoperative year (IIEF-5 scores and patient numbers at the end of the postoperative first year are shown in Fig. 1). Of the 96 patients, erection was achieved in 44 (33.3%) without any pharmacotherapy, in 41 (31.1%) using PDE 5 inhibitor and in 11 (8.3%) using intracavernosal injections. Erectile dysfunction was found in 36 (27.3%) patients at the end of postoperative 1st year. Of the 36 patients, 29 (22.0%) patients did not respond to penile rehabilitation and 7 (5.3%) of them refused to use additional treatment.
At the postoperative 5th year of our evaluation, a total of 14 patients were excluded from the study because of the fact that one patient received additional treatment for prostate cancer, four patients died, four patients could not be reached and five patients diagnosed new additional diseases (3 coronary artery diseases, 2 cerebrovascular diseases). Finally, a total of 118 patients evaluated at the end of 5th year (IIEF-5 scores and patient numbers at the end of the postoperative fifth year are shown in Fig. 2). Of the 118 patients, 87 (73.7%) were having good erectile function with and/or without medications. It was observed that of the 87 patients, 41 (34.7%) had erection without any pharmacotherapy, 36 (30.5%) had erection with PDE-5 inhibitors and 10 (8.5%) had erection with intracavernosal injection. There was no statistically significant difference between 1st and 5th year results in terms of erectile function status (p>0.05).
DiscussionIn our study, we found that 96 (72.7%) and 87 (73.7%) patients had good erectile function with and/or without medications at the 1st and 5th postoperative year, respectively. There was no statistically significant difference between 1st and 5th year results in terms of erectile function status (p>0.05).
RP was firstly presented by Young in 1905 as a perineal approach.10 Later, with the development of oncologic outcomes in the treatment of prostate cancer, increasing the quality of life has been the main target over time. Therefore, nerve-sparing approaches have gained importance. Walsh et al., aiming to preserve cancer control, urinary continence and sexual potency, developed modern radical retropubic prostatectomy (RRP) technique by regenerating surgical anatomy with modern concept of the neurovascular bundle (NVB) based on the work of himself.7 Weldon and Tavel described the first nerve-protective RPP in 1988.11 The same authors reported a 70% potency rate at the 24th month of the surgery.11 Frazier et al. reported a 77% potency rate after nerve-sparing RPP.12 Although the pathophysiology of post-prostatectomy ED is not clear, it has been obviously known that NVB damage has very important crucial role in the development of impotence. During RP one or more factors may be connected to the NVB damage such as excessive traction, post thermal injury, or direct dissection.13 When RRP is applied in a retrograde fashion, to enter the posterior plan where the prostate is removed from the rectum, the prostate is lifted up resulting in traction on the NVB. However, such traction on the NVB is not possible with RPP technique. Because, in that technique, to prostate is approached from posterior aspect under the endopelvic fascia. Also, it mustn’t be forgotten that in addition to formed traction on NVB during surgery, the potency rates depend on many factors such as preoperative erectile function status, patient co-morbidity, whether nerve-sparing surgery is performed or not, patient age, and experience status of the surgeon.
Kiyoshima et al. showed that only 48% of the NVBs were localized in the posterolateral region of prostate, the other 52% was laterally distributed away from the band formation.14 In addition to this, Kiyoshima reported that the shape and localization of the NVB depends on the degree of fusion between the prostate capsule and the lateral pelvic fascia.14 The RPP technique is an intrafascial technique in terms of prostatic approach which the lateral endopelvic fascia can be manipulated without its integrity disturbed during the operation. In that condition, perhaps only this feature can explain why we found such a high potency rate of 72.7% at the first postoperative year.
Wiygul et al. prospectively investigated the effect of neuroprotective surgeries on functional outcomes of 88 patients who underwent RPP.15 The improvement in impotence was defined as, to some extent hardening of penis to provide vaginal penetration.15 While improvement in hardening was achieved in the nerve-sparing surgery group at an average of 23.8 months, no improvement was observed in the nerve unprotected group.15 When they performed multivariate logistic regression analysis, they found that nerve-sparing surgery and pre-surgical erectile dysfunction status were independent predictors of early recovery of impotence developed after operation.15 Different from that study, herein we are able to present the independent effect of nerve-protective technique on potency, since we included only patients who are completely potent before surgery into study group.
In another well-designed study, it was shown that erectile potency rate significantly diminished after RP.16 Overall, 1st, 2nd, and 3rd year erectile potency rates were 45%, 51%, and 53% respectively, but reached up to 65.7% in preoperatively potent patients with bilateral nerve sparing.16 At 3rd, 13% of patients noted problems in their partnership.16 On the other hand, at the same time point, 77% were pleased with their sexual intercourse. In the same study, authors stated that results of functional outcomes including erectile function status and quality of life aspects after surgery were better in a high-volume center compared with those obtained from population-based data.16 At that point, it should be emphasized that not being examined the quality of life of patients has been an important limitation of our study.
Despite these strengths, our study is not devoid of limitations. First, we did not perform penile Doppler USG before and after surgery. We preferred using their response to the questionnaires which are subjective criteria. Second, another important limitation of our study was that we did not examine the testosterone levels of patients.
ConclusionAccording to our study results, short term and long term erectile function outcomes of patients undergoing RPP were favorable. We did not observe clinically or statistically significant increasing in rates of erectile function as time progresses beyond one year. This might give an idea about timing to offer third step treatment for erectile dysfunction, in other words penile prosthesis implantation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Informed consentInformed consent was obtained from all individual participants included in the study.
FundingNo specific grant was received by this study from any commercial, not-for profit sectors, or public funding agency.
Conflict statementAuthors declare that there is no conflict of interest between all authors.