Penile Mondor's disease (PMD) is the thrombophlebitis of the superficial dorsal vein of the penis. The patients usually feel the superficial vein of the penis like a hard rope and present with complaint of pain around this hardness. The physiopathology of this condition remains unknown; however, it is likely that vascular transection occurring after a surgical intervention or trauma caused by external compression may be triggering this condition.
Case reportA 36-year-old male presented with penile indurations that felt like a hard rope for the last one week that worsened with erection. The patient was diagnosed with PMD based on the findings from the physical examination, Colored Doppler Ultrasonography (Doppler USG) of the penis, and magnetic resonance imaging (MRI). The patient was diagnosed with subacute PMD. The patient was placed on a therapy involving oral anti-aggregants, topical anti-inflammatory agents, and heparinoid creams. The patient was recommended to abstain from sex.
ConclusionThe patients with penile Mondor's disease may experience anxiety and sexual dysfunction. The early recognition of the condition on the basis of clinical and radiological evidence increases the effectiveness of medical therapy and avoids surgery. In this regard, cooperation between the radiologist and the urologist is an essential component.
La enfermedad de Mondor con afectación peniana (PMD) es la tromboflebitis de la vena dorsal superficial del pene. El paciente suele sentir la vena superficial peniana como una cuerda dura y manifiesta dolor alrededor de esta dureza. Si bien todavía se desconoce la fisiopatología de esta dolencia, cabe la posibilidad de que el desencadenante pueda ser una transección vascular postquirúrgica o un traumatismo provocado por compresión externa.
Informe del casoVarón de 36 años con induración peniana y sensación de cuerda dura durante la semana previa que empeora con la erección. El paciente fue diagnosticado PMD conforme a los hallazgos de la exploración física, una ecografía doppler color del pene y una resonancia magnética (RMN). La PMD es de tipo subagudo. Se pautó un tratamiento con antiagregantes orales, agentes antiinflamatorios de uso tópico y cremas heparinoides. Se aconsejó al paciente que mantuviera abstinencia sexual.
ConclusiónLos pacientes con enfermedad de Mondor con afectación peniana pueden experimentar ansiedad y disfunción sexual. Un diagnóstico temprano de la dolencia ayudándose de las pruebas clínicas y radiológicas aumenta la eficacia del tratamiento médico y evita la cirugía. Por ello la colaboración entre el equipo de radiólogos y urólogos es fundamental en estos casos.
Mondor's disease is the thrombophlebitis of the superficial veins, and the condition was first described in the superficial veins of the chest by Henri Mondor in 1939.1 Isolated thrombosis in the dorsal veins of the penis was first reported by Helm and Hodge in 1958, and the authors defined this condition as penile Mondor's disease.2 PMD is a rare and under-recognized vascular benign disease of the penis occurring in sexually active young males. The true incidence of the disease is assumed to be higher than the reported incidence rates. There are only 53 reported cases in the literature.3 The present case ranks 54th in the literature, and is the second case that was diagnosed by MRI. Penile Mondor's disease affects sexually active males at all ages. The age of the patient's ranges between 18 and 70 years.3 The patients often present with the feeling of a hard rope on the dorsal penis. The patients report episodic or continuous aching and throbbing. Edema and redness may be apparent on the penile skin. Some patients report tension at the site of thrombosis. The patients also typically report increasing pain during erection. In some instances, patients may exhibit irritative urinary symptoms.4 The diagnosis can be easily established by physical examination. However, Doppler USG of the penis and MRI may help in the differential diagnosis. Penile Mondor's disease is clinically divided into three stages: acute, subacute-chronic, and recanalization period. In most cases, the flow in the vessel is re-established within nine weeks without any treatment, and the condition recovers in four to six weeks.5 The treatment of this condition involves medical measures and surgery. Surgical therapy involves thrombectomy and the resection of the superficial vein of the penis. The symptomatic cases exhibiting no flow on Doppler examination after Week 6 were considered to be resistant to medical therapy. These cases must be offered surgical therapy.
Case reportClinical featuresA 36-year-old male patient presented with penile induration that felt like a thin, ropy cord occurring after prolonged sexual intercourse. The patient reported pain for the last one week that increased with erection. The physical examination revealed superficial vein thrombosis that measured 8cm from the dorsal penis to the left inguinal area and was painful on palpation (Fig. 1). The other superficial veins were not palpable. There was no penile edema or hyperemia. The patient had an active sexual life. The patient did not have a remarkable history for sexually transmitted diseases. The patient was a smoker and he had type II diabetes mellitus in his past medical history. The patient did not report any problems with tendency to thrombosis. All laboratory results including blood glucose level and HbA1c were within normal ranges.
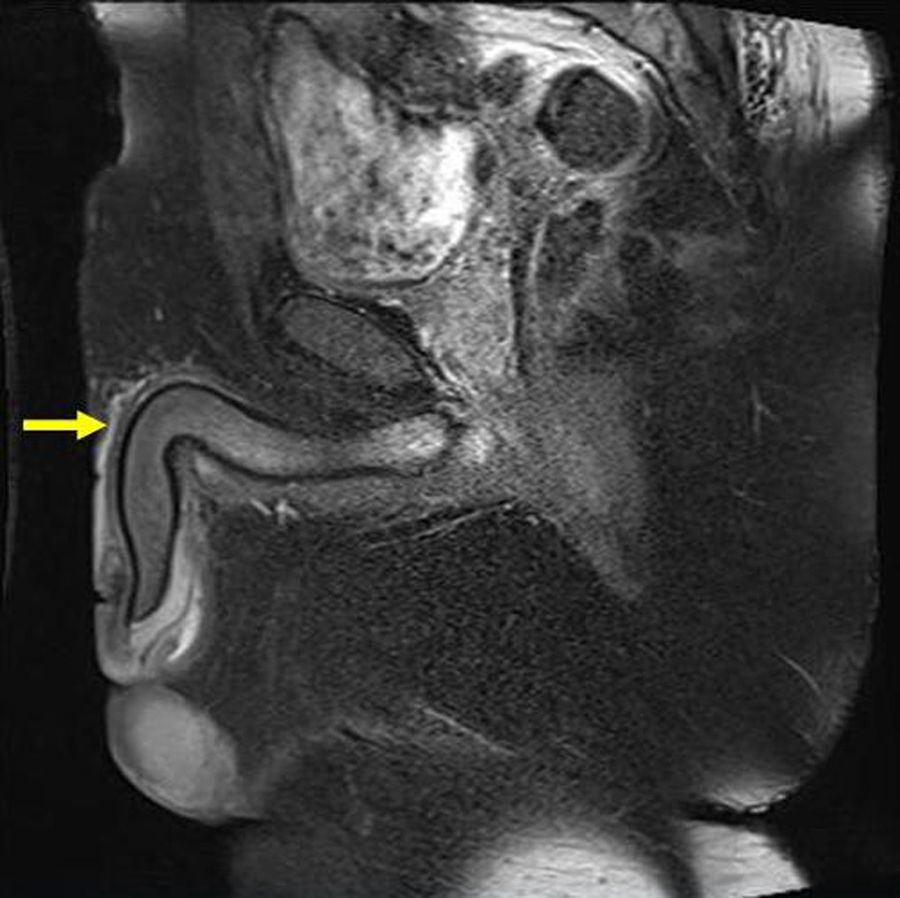
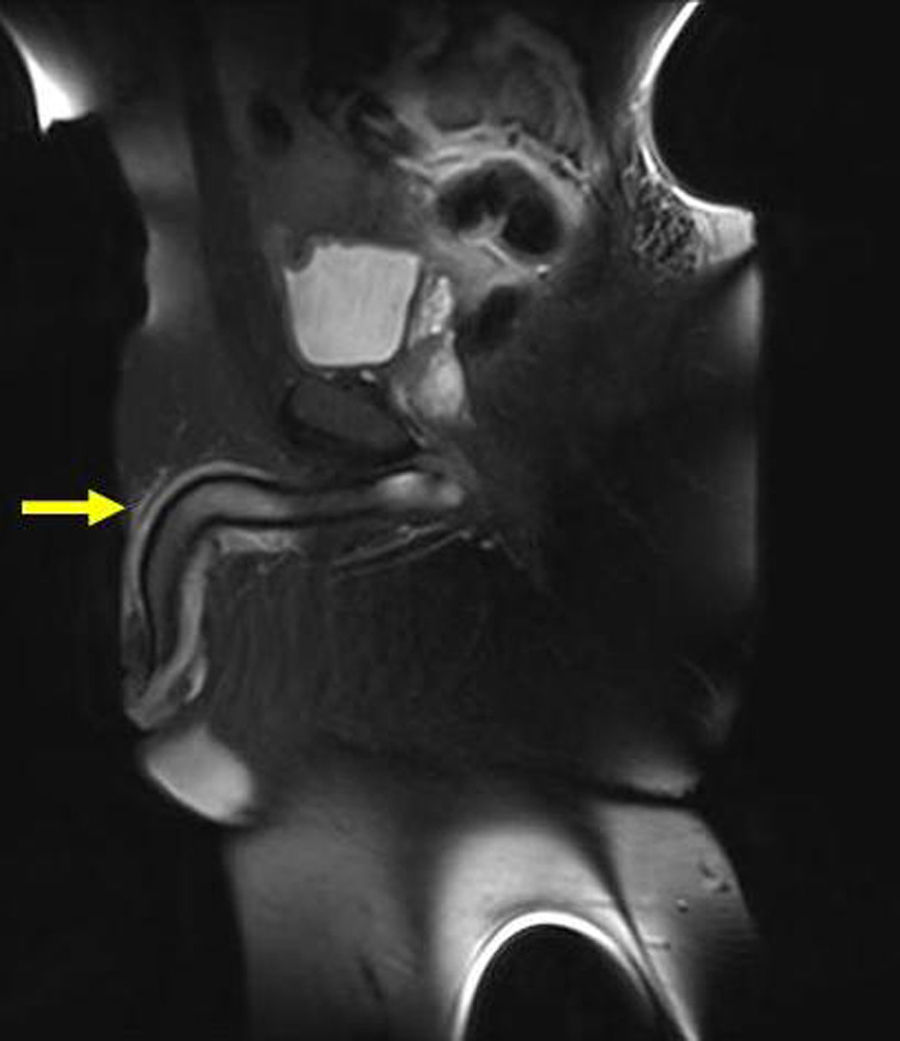
MRI findingsSagittal MRI sequences of the penis revealed a thrombosis in the superficial vein of the penis under the skin on the dorsal penis (Figs. 2 and 3). Doppler USG of the penis supported the diagnosis with the lack of flow in the superficial vein of the penis due to thrombosis. The Doppler USG also showed low velocity and highly resistant flow in the cavernous arteries.
The patient was placed on therapy involving anti-aggregant (ASA: 100mg/day) and topical heparinoid creams with the diagnosis of PMD. The patient was recommended to abstain from sex.
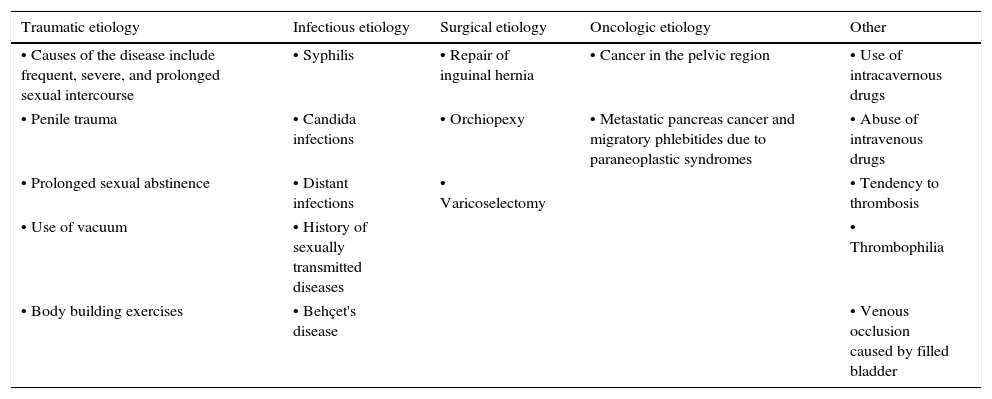
DiscussionPenile venous system; venous drainage of the penis begins at the base of the glans; a series of venous canals merge to form the dorsal vein of the penis, which in turn runs along a groove between the corpora and drains into the preprosthatic venous plexus. The circumflex veins orginate in the corpus spongiosa and extend around the corpus cavernosum on either side to merge with the deep dorsal vein perpendicularly. They are only present in the two distal thirds of the penis and total between 3 and 10 in number. Intermediate venules of the venous sinuses in turn form and drain into a capillary plexus beneath the tunica. This plexus system gives rise to emitting veins that generally extend obliquely between the layers of the tunica and drain into the circumflex vein at the dorsolateral level. The emitting veins in the proximal third of the penis merge over the dorsomedial surface of the corpus cavernosum bilaterally to form between 2 and 5 cavernous veins. In the hilum of the penis, these vessels pass between the pillars and the bulbar region receiving branches from each of them and joining with the internal pudendal veins.6 Apart from the erectile structures, vessels of the penile skin also originate from the external pudendal branch of the femoral artery. These vessels enter the penis at radix of penis. They run longitudinally in the Dartos layer and make frequent anastomoses between each other.7 This widespread venous network may be affected by trauma and inflammatory or infectious processes in the genital region under certain conditions. Many factors may result in the development of thrombosis in the dorsal vein of the penis. The thrombosis develops as a result of intravascular coagulation occurring after vessel wall damage, stasis, and tendency to hypercoagulation, known as Virchow's triad.8 However, trauma associated with sexual intercourse has been implicated as the major factor in the etiology of the disease.9 The reports in the literature have suggested various factors are involved in the development of Penile Mondor's disease. These factors were classified as trauma, infections, surgery, oncological, and others (Table 1).10
Causes of penile Mondor's disease.
| Traumatic etiology | Infectious etiology | Surgical etiology | Oncologic etiology | Other |
|---|---|---|---|---|
| • Causes of the disease include frequent, severe, and prolonged sexual intercourse | • Syphilis | • Repair of inguinal hernia | • Cancer in the pelvic region | • Use of intracavernous drugs |
| • Penile trauma | • Candida infections | • Orchiopexy | • Metastatic pancreas cancer and migratory phlebitides due to paraneoplastic syndromes | • Abuse of intravenous drugs |
| • Prolonged sexual abstinence | • Distant infections | • Varicoselectomy | • Tendency to thrombosis | |
| • Use of vacuum | • History of sexually transmitted diseases | • Thrombophilia | ||
| • Body building exercises | • Behçet's disease | • Venous occlusion caused by filled bladder | ||
The patients often present with the feeling of a hard rope on the dorsal penis. The patients do not exhibit symptomatic diversity, although asymptomatic cases may occur. The patients report episodic or continuous aching and throbbing. The patients report redness and tension on the corresponding skin area. The patients also typically report increasing pain during erection.4 The patients often present with a painful lesion palpated as a thick cord on the dorsal aspect of the penis that occurred within 24–48h of extensive sexual intercourse. The lesion most often occurs in the dorsal aspect of the penis; however, it can also appear at the penile root or sulcus coronarious. The thrombosed vein measures 2–10cm.11 In rare cases, the thrombosis may develop in the superficial pudendal vein. This condition is regarded to be a variant of the original penile Mondor's disease.12 Although, in general, the typical location of the Mondor's disease is the dorsal of penile, the disease can be seen at the different anatomic localization of penis. In the literature, a case of Juxtafrenular venous thrombosis was reported in a study by Pérez Rodrígueza et al., and surgical treatment was needed in this case because of not responding to conservative treatment.13 The laboratory tests of the patients reveal normal findings. However, some conditions characterized by a hypercoagulable state should be separately evaluated. These include antithrombin III, and protein C and protein S deficiencies, and MTHFR gene defects. The disease is most often confused with sclerosing lymphangitis. The thrombosed vessel specimen removed by surgery can be examined by pathological and immunochemical methods. The examination can reveal swelling of the endothelial cells, increased connective tissue, thrombosis, perivascular infiltration by the lymphocytes, hystiocytes, and plasma cells. The specimens show positive staining with monoclonal antibodies CD31 and CD34. This test may, however, show negative findings during the sclerotic process. The diagnosis of the disease is based on radiological findings including colored Doppler USG and MR imaging. There is only one case report in the literature that was diagnosed by MRI angiography.14 The present patient is the second case in the literature that was diagnosed by MRI. Doppler USG in PMD reveals dorsal vein thrombosis and associated hemodynamic changes. Although typical findings of superficial dorsal vein thrombosis on Doppler USG with the lack of flow signals are suggested to be sufficient for the diagnosis of Mondor's disease, there are also studies in the literature asserting the contrary. The lack of filling pattern and flow spectrum within the lumen of the superficial vein, low velocity, and high resistance flow pattern in the cavernous arteries are findings that differentiate PMD from sclerosing lymphangitis. The above Doppler findings are considered typical of PMD.15
The diagnosis of PMD using MRI is a controversial subject. The improved image quality in MRI and the use of godalinum during the procedure as an angiographic agent allowed the evaluation of early arterial and late venous phases. However, this procedure can only be recommended for cases in which a diagnosis or differential diagnosis could not be established. Systemic fibrosis is the most important factor limiting the use of MRI-angiography. There is only one case report in the literature that was diagnosed using MRI-angiography. This procedure was reported to be helpful in the diagnostic process due to the coexistence of various diseases and symptoms.14 The currently reported case is valuable for the demonstration of the possibility of diagnosing the condition without using godalinum to avoid the risk of systemic fibrosis.
ConclusionThe early and accurate diagnosis of PMD increases the effectiveness of medical therapy and avoids surgery. From this perspective, thorough physical examination and the knowledge of the findings on colored Doppler USG and MR imaging would be helpful in early diagnosis and treatment. The patients with penile Mondor's disease may experience anxiety and sexual dysfunction. Therefore, a strong collaboration is required to be established between the radiologist and the urologist to prompt early diagnosis and determine appropriate means of therapy.
Conflicts of interestThe authors declared no conflict of interest.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.