Situational anejaculation means that a man can ejaculate in some situations but not in others. Intercourse type of anejaculation means existence of ejaculation by masturbation, but not during sexual intercourse. In some cases, men may be able to ejaculate and attain orgasm with one partner but not with another. Performance anxiety, hostility toward the partner, dysfunctional psychosexual development, and unconscious desire to avoid pregnancy are the possible underlying conditions. We herein reported a case of wife-specific intercourse anejaculation succesfully treated with sexual therapy. According to our best knowledge, this is an important case study in literature about intercourse type of situational anejaculation specific to the patient's wife that was treated with psychosexual counseling. The authors conclude that this clinical course of situational intercourse anejaculation suggests a psychological problem in these patients and sexual therapy is effective.
La aneyaculación situacional significa que un varón puede eyacular en algunas situaciones, pero en otras no. El tipo de aneyaculación sexual implica la existencia de eyaculación mediante la masturbación, pero no durante las relaciones sexuales. En algunos casos, los varones pueden ser capaces de eyacular y alcanzar el orgasmo con un compañero, pero no con otro. La ansiedad subyacente, la hostilidad hacia la pareja, el desarrollo psicosexual disfuncional y el deseo inconsciente de evitar el embarazo son las posibles situaciones de fondo. En este documento, informamos de un caso de aneyaculación sexual específica de la esposa tratada con éxito con terapia sexual. Según nuestro mejor conocimiento, este es el primer estudio de caso en la bibliografía sobre el tipo de relación sexual de la aneyaculación situacional específica de la esposa del paciente que fue tratado con asesoramiento psicosexual. Los autores concluyen que este curso clínico de aneyaculación del coito situacional sugiere un problema psicológico en estos pacientes y la terapia sexual es efectiva.
Anejaculation is defined as the inability to ejaculate semen despite sexual stimulation by intercourse or masturbation. It may result from organic causes such as prostatitis, surgery to the prostate, conditions affecting the nervous system (Multiple Sclerosis, Parkinson's disease, spinal cord injuries, diabetes mellitus, etc.), or drugs.1 Anejaculation can be classified as orgasmic (organic) anejaculation, anorgasmic (psychogenic/idiopathic) anejaculation, and situational anejaculation. Situational anejaculation means that a man can ejaculate in some situations but not in others. There are different types of situational anejaculation: clinic anejaculation (can collect semen at home, but has anejaculation in clinics, hospitals), periovulatory anejaculation (unable to ejaculate at ovulation, but can ejaculate on other days), unexpected anejaculation (first time failure of ejaculation on day of ovulation), masturbatory anejaculation (ejaculates during intercourse, but not by masturbation), and intercourse anejaculation (ejaculates by masturbation, but not during intercourse).2,3 Typically, intercourse anejaculation is stressed induced. The factors possibly contributing to this entity are performance anxiety, negative affect (fear and hostility in attitude) toward the partner, dysfunctional psychosexual development, lack of awareness of one's body, psychological inhibition due to guilt, inadequate sexual arousal, previous sexual trauma, oedipal fears of retaliation, fear of defiling partner with semen, and unconscious desire to avoid pregnancy. There is no sufficient evidence for these theories.1,4 Intercourse anejaculation or in other words inability to ejaculate into the vagina is a rare situational anejaculation type.2 A rarer case is that intercourse anejaculation is specific to a particular person. In this study, we reported a case of wife-specific intercourse anejaculation succesfully treated with sexual therapy. According to our best knowledge, this is one of the first case studies in literature about intercourse type of situational anejaculation specific to the patient's wife that was treated with psychosexual counseling.
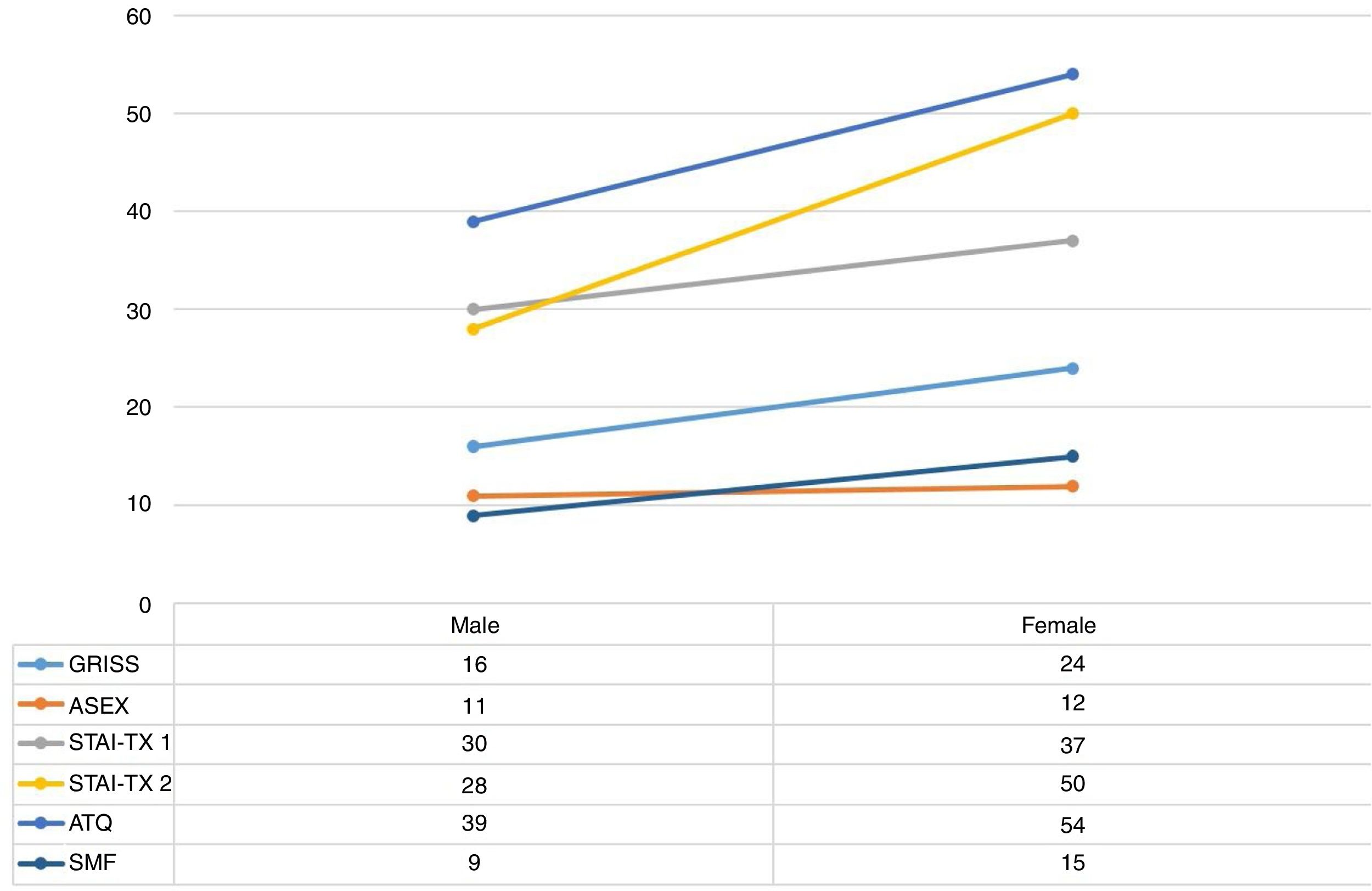
Case presentationA 32-year-old man (engineer) with a 27-year-old woman partner (patient's wife, teacher) who lives in a small city, Adiyaman (Region of Eastern Anatolia, Turkey), was admitted to Adiyaman University Training and Research Hospital alone because of inability to ejaculate intra-vaginally since he got married (one year). There was an experience of sexual intercourse before marriage without a problem of anejaculation and he preferred heterosexuality. He was masturbating twice a week and had wet dreams. Any anatomical problems were not reported related to his partner. Before marriage, the patient's partner had felt discomfort during a physician's pelvic exam. After marriage, they had no sexual intercourse. The gynecologist diagnosed it as vaginismus. They had not received any psychiatric support and the problem of vaginismus with Kegel exercise suggestion of the gynecologist was improved. After the vaginismus problem was solved, sexual intercourse started. He reported no orgasm during coitus, despite normal erections or libido. He had sexual intercourse three times a week. Although the sexual intercourse lasted 25–35min, he could not ejaculate during coitus. The patients’ partner was able to achieve multiple orgasms during sexual contact. The partner said that the patient did not want to continue sexual intercourse due to vaginal dryness, and the patient took his penis out of her vagina and had orgasm with masturbation within 3–4min. The patient had not an arranged marriage. There was no history of use of alcohol, cigarette, and cannabis before presentation. He had two brothers and one sister and family history did not indicate any findings of ejaculatory dysfunction. Physical examination revealed no pathology which could point to any reason for organic anejaculation. Neurological examination findings were normal. He was referred to the urology department, and no organic pathology was detected. (Total testosterone, free testosterone, luteinizing hormone, prolactin and estradiol revealed normal levels. Genital and rectal examination and transrectal ultrasound showed normal testicles, prostate, penis, and seminal vescicles.) Sexual therapy with his partner was suggested the patient. Therapy sessions with the couple were held weekly. Each session lasted about 40min to an hour. At first, the patient and his partner were seen separately. After these evaluation sessions, the information about their distress was given in a combined session. Therapeutic purposes were clarified. Information about the sexual therapy process was given. In order to better manage the treatment process, some scales were given and requested separately. At the next interview, information about sexual anatomy and physiology of women and men was clarified. A ban on any form of sexual activity was suggested. It was given the task of recognizing her sexual organs and examining her pleasure points. We talked about foreplay and gave some information on some techniques. The psychometric scales were taken and evaluated (Fig. 1). In the subscales of the male version of Golombok Rust Inventory of Sexual Satisfaction (GRISS)5; Impotence: 1, Premature Ejaculation: 6, Infrequency: 2, Male Avoidance: 0, Male Non-sensuality: 0, Male Dissatisfaction: 4, Non-communication: 2. In the subscales of the female version of GRISS; Anorgasmia: 3, Vaginismus: 6, Infrequency: 2, Female Avoidance: 1, Female Non-sensuality: 1, Female Dissatisfaction: 4, Non-communication: 4. According to the Symptom Checklist-90-Revised (SCL-90-R)6 of man, the subscales of Somatization (0.75), Obsessive-Compulsive (0.90), Depression (0.92), Interpersonal Sensitivity (0.88), Paranoid Ideation (1.33), and Global Severity Index (0.73) have higher scores. In SCL-90-R for woman, Obsessive-Compulsive (0.80), Depression (0.92), Interpersonal Sensitivity (1.00), Paranoid Ideation (1.50), Hostility (0.83), and Global Severity Index (0.73) have higher scores. The long form (63 items, 12 subscales) of the Rosenberg Self-Esteem Scale (RSES)7 indicated similar results for man and woman. (For man; D1: 0.50, D2: 3, D3: 1, D4: 1, D5: 0, D6: 0, D7: 0, D8: 2, D9: 1, D10: 1, D11: 1, D12: 0. For woman: D1: 0.25, D2: 3, D3: 1, D4: 3, D5: 1, D6: 0, D7: 0, D8: 2, D9: 0, D10: 0, D11: 3, D12: 0.) On the next visit, it was learned that they did not comply with the ban of coitus. They said they had sexual intercourse that lasted 15min with an ejaculation. In later sessions, it was learned that the problem had completely disappeared. They were informed to improve their communication skills and ensure that they have a better quality of life. He has been able to ejaculate satisfactorily during a majority of the couple's sexual interactions. The duration of the sexual intercourse with an ejaculation fell from an average of 15min to an average of 5min. After 10 sessions the sexual therapy was terminated. Written informed consent was taken from the patients in order to publish their data.
DiscussionAnejaculation may be primary or secondary, total, selective, or occasional. Patients having primary selective anejaculation can masturbate but cannot ejaculate intravaginally and this situation is called by some authors as intercourse anejaculation. Sometimes, intercourse anejaculation may be seen in specific conditions. A man may be able to ejaculate and attain orgasm with one partner but not with another. In our patient this problem was related to the wife. This disorder stems from unconscious conflicts or abnormal beliefs about intravaginal ejaculation.1,3 The reported cases of intercourse anejaculation in the literature have certain common characteristics: growing up in rural areas, strict upbringing, arranged marriage, no experience of sexual intercourse premarital. The cases related to anejaculation reported from Israel are frequent. It is stated that Jewish orthodox population is at risk because of strict religious regulations.8,9 More rarely, there are cases reported from other communities and religious groups. Gopalakrishnan et al.,10 from a psychiatry clinic, reported a case who had been brought up in a family that followed orthodox Hindu traditions. There was a pressure on couple to have a child. They suggested that resolving relationship issues, reducing anxiety by cognitive behavioral therapy, and altering masturbatory techniques, and increasing the level of information about the sex can help the patient overcome his ejaculatory dysfunction. In another study11 in a Muslim society (Egypt), two situational psychogenic anejaculation cases were reported. These patients were from urban population and one of them was the sole boy in the family. However, in our case we had the opposite features. The patient believed that sexual therapy would be beneficial. Hence, it was thought that there might be problems in some areas with the information obtained from scales and individual interviews. In the vast majority of cases reported, the main application cause was childlessness and therefore, a big number of the cases were reported by the urology departments. Psychosexual counseling was not welcomed and even rejected by patients with situational anejaculation according to literature. The main concern of these patients or couples were to conceive as soon as possible, but the counseling may take a long time. Also, in rural societies, psychological consultation means they were mentally unsound. This is another reason why treatment is delayed.1,11–13 Our study is important in this regard. Our patient adapted to sexual counseling and tried to follow instructions. Without the need to go to the urology department, the problem was solved with therapy. So, our subjective thoughts on this case are related to interpersonal, family, and couple relationships, that is, psychological. Arizona Sexual Experiences Scale (ASEX)14 indicated a marked sexual problem in both man and woman. In the scales applied, the patient's partner generally had higher scores, the problem level seemed higher. The paranoid ideation and interpersonal sensitivity scores were high in patient and his partner. The woman had more anxiety. The male version of the GRISS indicated a premature ejaculation and the female version revealed a problem of vaginismus. There was a dissatisfaction problem in man and woman. We have formulated this problem as follows: due to the vaginismus problem and anxiety in female, a poor start was made in terms of the sexual intercourse, so, the level of anxiety in male had increased, an intercourse anejaculation occurred, sexual therapy increased the level of sexual knowledge of female and male and reduced the level of anxiety, the problem was solved.
If we look at the literature, a detailed anamnesis and sexual history should be taken from patients who have complaint of anejaculation. They should be asked to come in pairs. The quality of the three phases of the sexual response cycle, including desire, arousal and ejaculation, should be assessed. The subjects other than the psychological conditions that may lead to problems related to this topic should be examined in detail by being directed to the departments such as urology and gynecology. Various therapeutic regimens have been advocated for the management of anejaculation.15 While Masters and Johnson9 advise sex therapy aiming at the production of ejaculation by the partner, Geboes et al.1 use sexual education, hormones, psychotherapy, and the electrovibrator. Some studies indicate that situational anejaculation is treated with counseling services, while others say it is not effective.10 Our study shows that sexual therapy can be successful.
ConclusionPrevious reports have indicated limitedly the instructions about heterosexual vaginal intercourse anejaculation.3 But we believe this is an important case study in literature about intercourse type of situational anejaculation specific to the patient's wife that was treated with psychosexual counseling.16 Further psychiatric research should be conducted with respect to situational intercourse anejaculation to provide a greater understanding of prevalence, etiology, course, and treatment.
Conflict of interestsThe authors declare no conflict of interests.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.