Patent ductus arteriosus is treated according to its indications conservatively with medications or by surgical closure; the latter was traditionally performed by an open technique, then later, the percutaneous approach was developed for selected cases and finally, in recent years, it has been done by thoracoscopic surgery with success challenging percutaneous results. However, at our hospital, this had not been tried before. We present the case of a female patient who met the ideal criteria for this procedure to be performed and in whom it was successfully accomplished without complications; hence our report, motivated by the historical importance and as a baseline for future cases.
La persistencia de conducto arterioso es tratada de acuerdo a sus indicaciones de forma conservadora con medicamentos o por cirugía; originalmente esta se realizaba de forma abierta, posteriormente surgió la oclusión del conducto por vía percutánea en pacientes seleccionados y por último en años recientes por cirugía toracoscópica con resultados satisfactorios que compiten con los resultados percutáneos, sin embargo en nuestro Hospital, este último no se había realizado antes. Presentamos el caso publicado de paciente femenino, la cual era candidata ideal para este método, habiéndolo realizado con éxito en nuestra institución por primera vez, el motivo de presentación del caso recae en la importancia histórica del mismo, así como base para la modificación de la técnica en nuestros futuros casos.
Patent ductus arteriosus (PDA) is a cardiovascular abnormality wherein the duct, which is part of the normal foetal circulation that normally closes spontaneously within the first 24–36h after birth, remains patent. The consequence is a shunt from left to right between the aorta and pulmonary artery which has haemodynamic repercussions and if not addressed, can be fatal. In Mexico, PDA is the most common congenital heart defect.1 Traditionally, this abnormality was corrected with open surgery, suturing the duct where, in some groups, this is transected. In 1971, Porstmann et al. reported the first percutaneous occlusion, changing the direction of management of these patients in the last three decades.2 In 1993, Laborde et al. performed the first thoracoscopic closure with high success rates,3 and this opened up a debate as to whether the percutaneous technique was better than the thoracoscopic as there was no significant benefit in overall success, complications or blood transfusions when compared with minimally invasive surgery.4 In our country, Arellano-Ostoa et al. analysed 105 cases where successful occlusion was reported in 100% of patients with a postoperative complication rate of 3.8%.5 Alvarez-Tostado et al. reported the first two successful cases in 1994, followed by another report of their experience in 62 patients with 100% successful occlusion and 4.8% complications.6,7 This presentation is motivated by the importance of the advantages offered by minimally invasive surgery over open techniques, as well as the large number of patients with PDA treated at our hospital, making it essential that we seek to introduce this technique.
PresentationThis was an 11-year-old female patient, 132cm tall and weighing 32kg, referred to the Paediatric Cardiology Department from another hospital. She had a history of a grade III/IV continuous murmur in the left 2nd intercostal space with femoral pulses with increasing amplitude and associated dyspnoea on moderate exertion. Previous investigations included transthoracic echocardiogram which reported patent ductus arteriosus as the only morphological abnormality, with a diameter of 8mm at the pulmonary and aortic sides, with a length of 17mm, with a pulmonary artery pressure of 31mmHg and Qp/Qs of 1.1:1, preoperative blood studies within normal ranges; thoracoscopic surgical closure was decided after consensus with the medical-surgical group.
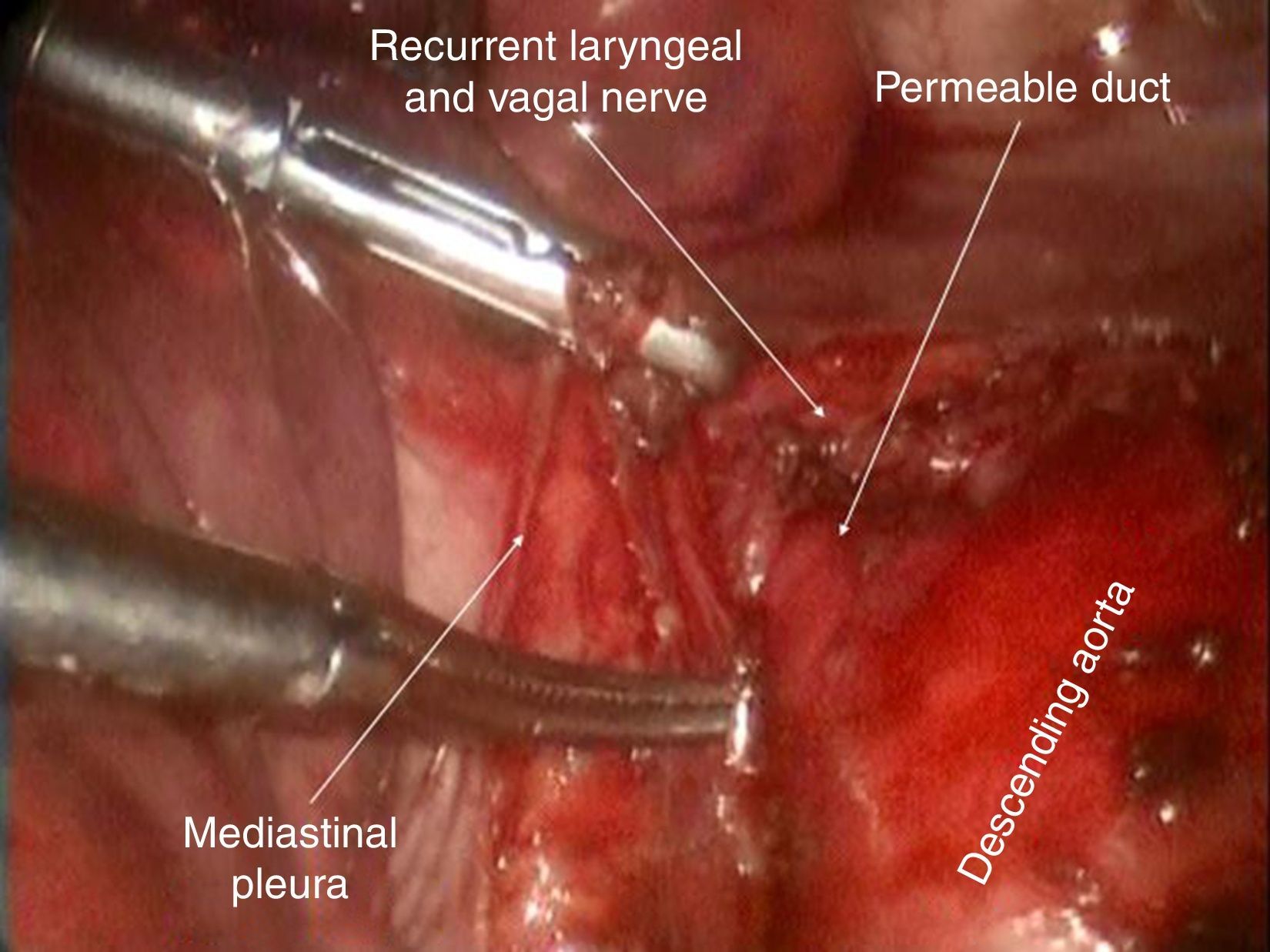
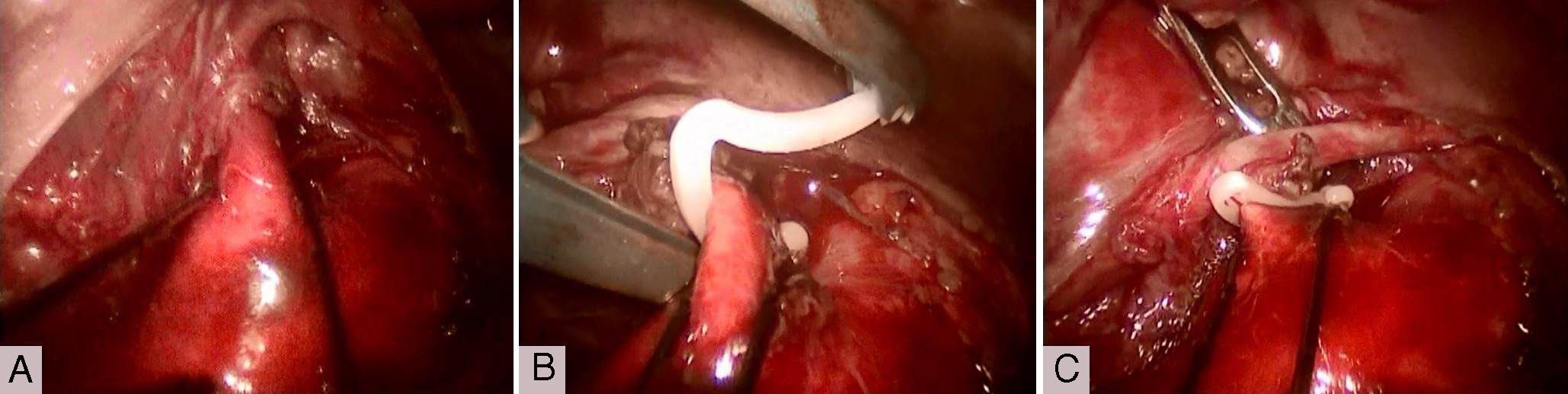
Once in the operating theatre, selective intubation of right lung was performed and an oesophageal stethoscope was placed to ensure the absence of murmur once the duct was closed (Fig. 1), with the patient in right lateral decubitus position and flexion at the point between the last costal arch and the iliac crest in order to lower the hip, allowing greater manoeuvrability of the instruments during surgery (Fig. 2). A 5mm incision was made in the 3rd intercostal 1cm medial to the scapula where a 30° thoracoscope or working tools could be introduced, another immediately caudal to the scapula in the 4th intercostal space as a working port, and a third in the 3rd intercostal space, anterior axillary line, for curved Foerster forceps for lung retraction. During the procedure, aortic mediastinal pleura was incised longitudinally, retracting it medially in order to dissect the path of the duct with Maryland forceps supported by angled forceps (Fig. 3). Once the duct was referred with a silk suture, a long Hem-o-lok® haemostatic clip was placed without complications (Fig. 4), absence of murmur was confirmed with the oesophageal stethoscope and patient left the operating room with a chest drainage and without mechanical ventilation. Once in the Coronary Care Unit, the drain was removed at 12h after collecting 20cc of blood-stained serous fluid; at 20h post-intervention, the patient was discharged home without complications (Fig. 5). Post-intervention echocardiogram reported 100% occlusion of the duct and the patient's progress continues to be satisfactory after one month of follow-up.
Surgical closure of PDA corrects haemodynamic damage caused by the vascular shunt that is sometimes responsible for congestive heart failure. In older patients, it may be indicated to improve patient life expectancy by preventing infectious endarteritis, pulmonary hypertension, heart failure, and aneurysm and/or pulmonary/systemic embolism formation.8 The first report of thoracoscopic closure in our country dates back to 1994. There are few groups reporting use of this procedure with their patients.6 These authors have laid the groundwork to continue the trend towards a more widespread use of this technique which provides frank benefits. Two authors with the highest number of reported cases, are Villa et al., with 743 patients (mean age 1.6 years, mean weight 9kg, 0% mortality, mean surgical time 20min, mean hospital stay 2 days, 0% residual fistula in underweight patients, 0.3% in children and 4.7% in adolescents (p=0.001), 4.2% dysfunction of the recurrent laryngeal nerve in underweight patients, 0.3% in children and 0% in adolescents (p=0.012)), who concluded that thoracoscopic closure compares favourably with open surgery and, when compared to the percutaneous technique, presents an attractive option in relation to cost-effectiveness.9 The other group is Nezafati et al. who, at 2000, so far have the highest number of patients (mean age 5.2 years, mean weight 9.8kg, one death reported from chylothorax complication, one conversion to open surgery due to rupture of the vessel wall, 4 residual fistulas and 12 transient recurrent laryngeal nerve injuries, mean hospital stay 21h), on whom they performed closure using two titanium clips, confirming closure with an oesophageal stethoscope as in our case. They concluded and reaffirmed the safety and feasibility of this technique.10 In our patient we decided to use Hem-o-lok® clips; there are series in the literature reporting 0% residual fistula and it is the perception of the surgical team that better closure of the duct is obtained because these clips contain a mechanism that ensures closure at the distal end while the titanium clips do not.11
Since the first percutaneous closure was published, countless studies have demonstrated their superiority over open surgery to the extent that today, open surgery is reserved for complex cases. However it was not until recently that, due to the accumulating evidence of excellent results with thoracoscopic closure, Wang et al. carried out a meta-analysis comparing percutaneous to thoracoscopic closure and found seven studies that met their inclusion criteria, noting that the percutaneous technique did not increase closure success rate (RR: 0.92, 95% CI: 0.82–1.03, p=0.16), and nor did it reduce the number of post-procedure complications (RR: 0.74, 95% CI: 0.44–1.25, p=0.26) or blood transfusions (RR: 1.10, 95% CI: 0.16–7.67, p=0.93); catheterisation was 5.19 times more associated with a significant number of residual vascular shunts (95% IC: 1.41–19.20, p=0.01). This evidence is an excellent argument for thoracoscopic surgery over percutaneous closure. However it is a difficult habit to break among cardiologists.4 Meanwhile, in our hospital, we will continue to develop and refine this surgical procedure, which is of great benefit to the patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.