Giant cell tumours (GCT) are usually benign, locally aggressive tumours. They tend to occur in long bones and rarely in small bones, with an incidence rate is 1.2–2.4% in the bones of the foot. The objective is to present a unique case in the literature of a GCT that only affected the first cuneiform. We present the case of a 35-year-old male patient seen at Hospital General de México (HGM) with seven months history of pain and increased volume in the medial region of the right foot, with X-ray and MRI images consistent with GCT in first cuneiform of the right foot. The excisional biopsy confirmed GCT. The definitive treatment consisted of curettage, cryotherapy with nitrogen and heterologous bone graft placement. Evolution was satisfactory, with no pain, no volume increase, normal gait and radiographic bone graft integration. Follow-up was at 24 months.
El tumor de células gigantes (TCG) es un tumor generalmente benigno y localmente agresivo. Se presenta más en huesos largos y raramente en huesos pequeños, su incidencia es de 1.2 al 2.4% en los huesos del pie. El objetivo es la presentación de un caso único en la literatura, de un TCG que sólo lesiona la primera cuña. Masculino de 35 años de edad, visto en el Hospital General de México (HGM) con un padecimiento de 7 meses de evolución, caracterizado por dolor y aumento de volumen en la región medial del pie derecho, con imágenes radiológicas y de RMN compatibles con TCG en cuña del pie derecho, se le realizó biopsia excisional, la cual reportó TCG. El tratamiento definitivo consistió en curetaje, crioterapia con nitrógeno y colocación de injerto óseo heterólogo. Presentó una evolución satisfactoria, sin dolor, sin aumento de volumen, con marcha normal, y radiográficamente con integración de injerto óseo. Seguimiento de 24 meses.
GCT is an aggressive local tumour containing mononuclear stromal cells and multiple multinucleated giant cells.
It is the sixth most common primary bone cancer. It is predominant in women, with a ratio of 2:1, and presents from 20 to 40 years of age. 60% are found in long bones, primarily the distal femur, proximal tibia, distal radius and proximal humerus, and represents 20% of all primary bone tumours in the foot and ankle.1–6
They are not very common in the small bones of the hands, feet and ankles.5–7 Only 6% of GCTs occur in the ankle and foot, with the distal tibia being the most common location.3,6 Their incidence in small bones is 1.2–2.4%.2,4,7,8
Jae et al.8 reported a case affecting the first and second cuneiforms and the bases from the first to the third metatarsal,8 Wendi O’Connor et al.9 reported a case affecting the third cuneiform with extension towards the second9 and Roberto Biscaglia et al.7 reported 2 patients with involvement of the first cuneiform and adjacent bones and another patient with involvement of the third cuneiform and cuboid bones.7
We report the case of a patient with a single expansionary lesion only affecting the first cuneiform of the right foot.
Case reportCase report: 35-year-old male with onset in December 2012, characterised by increased volume in the medial face of the right foot, together with burning pain of 5/10 intensity on the Visual Analogue Scale (VAS), which increased to 8/10 when walking and upon palpation.
He underwent infiltration privately but the symptoms continued and the pain progressively increased to VAS 8/10, with further increased volume.
He came to HGM on 16/07/2013 with gait affected due to the right leg, with a hard, non-mobile tumour measuring 3cm×3.5cm×0.5cm in the first cuneiform, painful upon palpation.
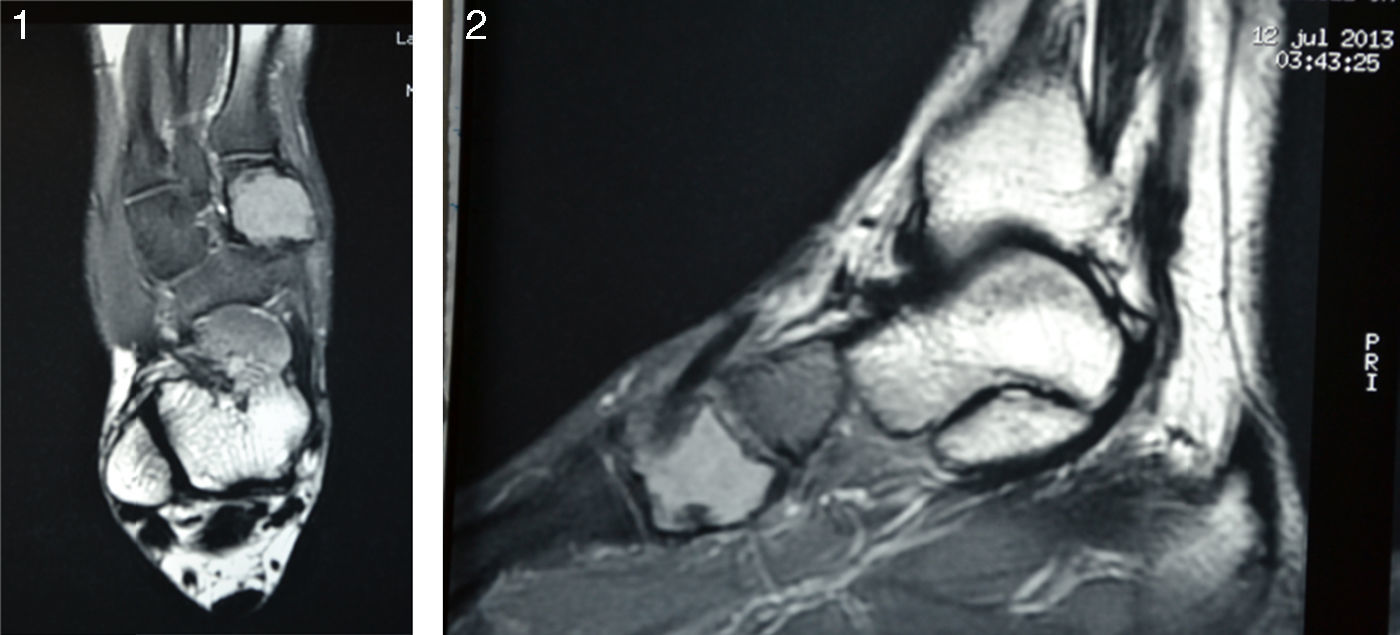
X-rays showed a 2.2cm×3.3cm lytic lesion in the first cuneiform with round, sclerous edges and no periosteal reaction. The MRI (Figs. 1 and 2) showed a multi-lobe 3.2cm×2.2cm×5.2cm lesion affecting the entire first cuneiform, with integral, sclerous edges and hyperintense areas in T2.
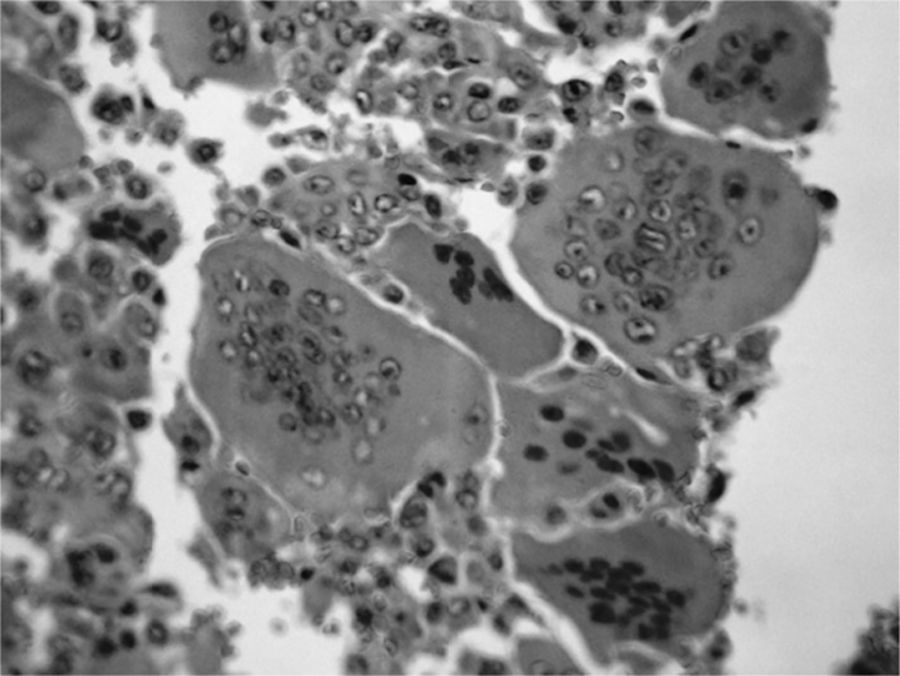
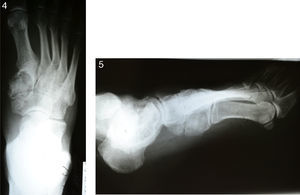
An excisional biopsy was performed on 29/07/13, showing GCT (Fig. 3). The definitive treatment consisted of curettage, cryotherapy and heterologous bone graft placement (Figs. 4 and 5).
Evolution was satisfactory, with no pain or volume increase, normal gait and radiographic graft integration. Follow-up was at 24 months.
DiscussionIn GCTs, pain is the predominant symptom, followed by increased volume due to tumour growth or oedema and, thirdly, fracture at the affected site, as reported by Dahlin, Osman and Biscaglia.2,3,7 According to Kwang-Son and Jae Hoon,5,8 diagnosis and treatment is delayed by more than 6 months. The patient presented burning pain and increased volume and was diagnosed after 7 months, consistent with the literature.
According to Green, Dahlin, Jae Hoon and O’Connor,1,2,8,9 it presents in most patients from the age of twenty to forty years. This is consistent with the case report.
It is rarely found in the small bones of the foot, with an incidence rate of 1.2–2.4%.2,4,7,8
Jae et al.8 reported a case where the first and second cuneiforms and the bases from the first to third metatarsal were affected; Wendi O’Connor et al.9 reported a case in which the third cuneiform, with extension towards the second, was affected; Roberto Biscaglia et al.7 reported 2 patients with involvement of the first cuneiform and adjacent bones, and another patient with involvement of the third cuneiform and cuboid bones. In the HGM orthopaedics department, the most common site for GCT affecting small bones is the ankle, followed by the heel bone. This is the first case affecting the first cuneiform, which is consistent with the literature, in that GCTs are rarely found on the small bones of the foot.2,4,7–9
The patient's X-rays showed an expansionary osteolytic lesion with defined sclerous edges and occasional stringiness, consistent with Green, Dahlin and Kwang,1,2,5 and this was confirmed by the MRI.8,10
Histologically, Green, Dahlin and Walid Osman1–3,10 refer to a double population of mononuclear stromal cells and giant cells uniformly distributed throughout the tumour, as reported in the patient's biopsy.
There are multiple forms of treatment: curettage, abrasion debridement, cryotherapy with different elements, use of phenol or phenol combinations and graft.1,2,5–8,10 The patient was treated with curettage plus cryotherapy and graft, with satisfactory evolution.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.