A 3-month-old female patient is presented, with ileo-ileal intussusception secondary to Meckel's diverticulum. The patient underwent emergency surgery due to a diagnosis of intestinal obstruction secondary to intussusception.
Se reporta caso de paciente femenino de 3 meses de edad, con una intususcepción intestinal íleo-ileal secundario a divertículo de Meckel, intervenida quirúrgicamente de urgencia por diagnóstico de obstrucción intestinal secundario a una invaginación intestinal.
Intussusception is when one part of the intestine folds or invaginates into another. It is one of the most common causes of intestinal obstruction in infants and children and the second most common cause of acute abdominal pain in infants and toddlers. Intussusceptum is the proximal part and intussuscipiens the distal part.1
Its incidence worldwide is 1–4 out of every 2000 infants and children. It is most commonly reported in boys at a ratio of 2:1 or 3:2. 75% of cases occur before the age of 2, and more than 40% from 3 to 9 months of age.1
Intussusception in neonates (0.3%) caused by other conditions. Other conditions increase its incidence to 44% at 5 years and 60% from 5 to 14 years.1
The most common conditions involved are: Meckel's diverticulum, intestinal polyps and intestinal duplication. Rarer causes include: periappendicitis, stump appendicitis, invaginating appendectomy, appendiceal mucocele, local suture line, lymphoid hyperplasia, ectopic pancreas, abdominal trauma, benign tumours (adenoma, leiomyoma, carcinoid, neurofibroma, haemangioma) and malignant tumours (lymphoma, sarcoma, leukaemia).1
In infants, most cases are idiopathic.2 In only 2–8% of patients are there anatomical abnormalities that cause intussusception,3 the most common of which is Meckel's diverticulum, especially in children over 2 years of age and adults.2
Anatomical type: ileocolic (85%), ileoileocolic (10%), appendicocolic, cecocolic, colocolic (2.5%), jejunojejunal, ileoileal (2.5%).1
This paper reports the clinical characteristics of a case of ileoileal intussusception secondary to Meckel's diverticulum in a 3-month-old baby girl treated at the Paediatric Surgery Department of Hospital Pediátrico de Tacubaya. This is an uncommon condition in small infants.
Case report3-month-old female patient, the first child of an 18-year old mother with no significant prenatal history. She was brought to the paediatric emergency room after 8h of vomiting on 15 occasions, intense diffuse abdominal pain with periods of calm and bloody pasty bowel movements. The mother administered oral ampicillin, paracetamol and butyl hyoscine with no improvement. We were called when she arrived at the paediatric ER and found a lethargic patient with pale skin and mucous membranes, poor hydration, crying without tears and salivating, cardiopulmonary system normal, soft, compressible abdomen, with no organ enlargements, tympanic, with pain upon profound palpation in right half of abdomen. Mass in right iliac fossa, with signs of peritoneal irritation.
The patient was admitted and administered intravenous saline and Hartman solution (10ml/kg). The blood test showed leukocytes 8130, neutrophils 40%, lymphocytes 49%, platelets 127,000, haemoglobin 10.63g/dl, haematocrit 31.59%, sodium 137mE1/L, potassium 5mEq/L, chlorine 105mEq/L, PT 14.1s, PTT 36.4s, INR 1.16, activity 80%.
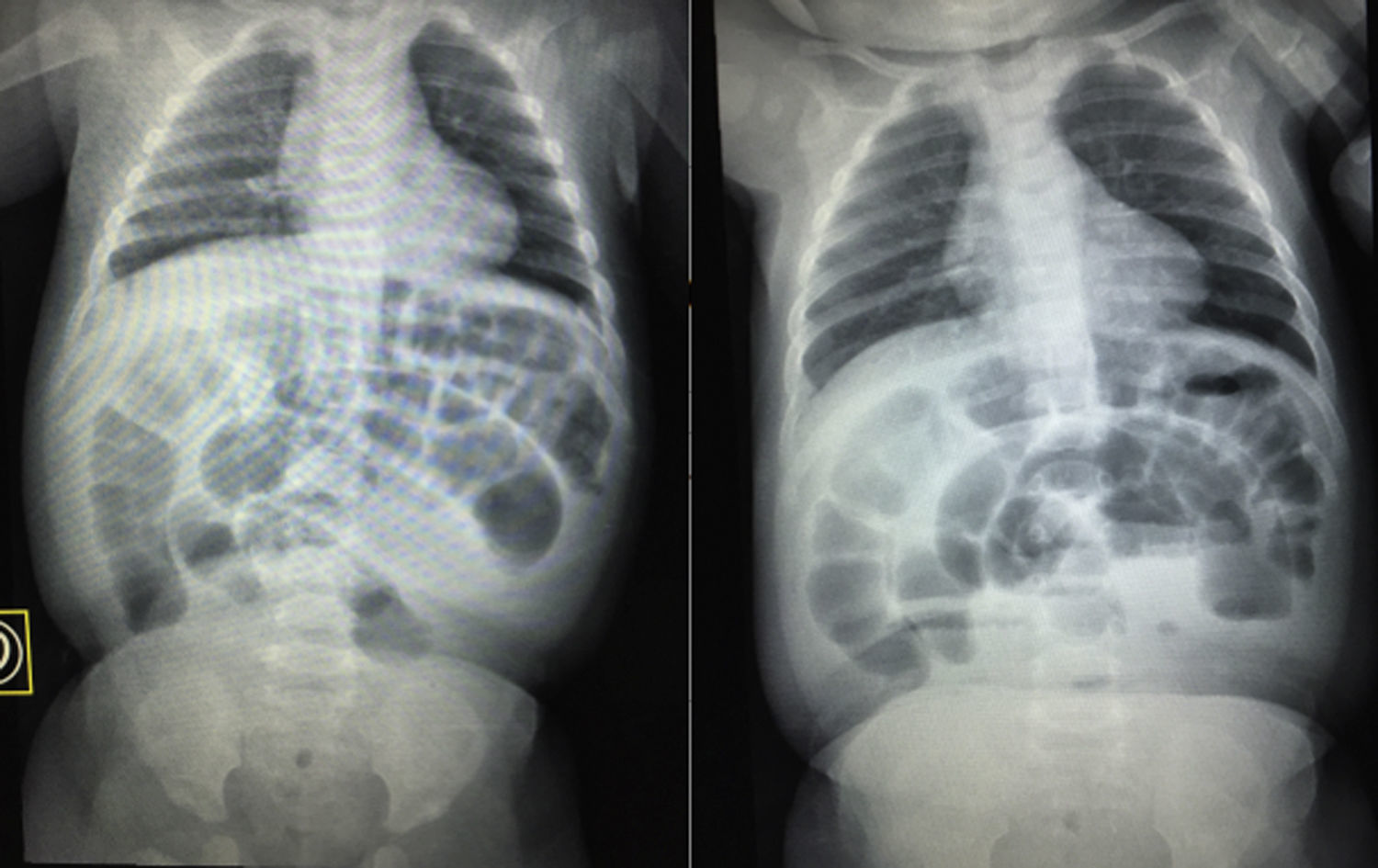
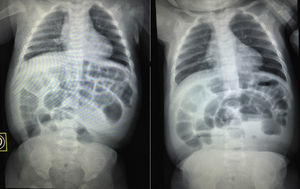
A simple X-ray of the abdomen while standing and lying down showed poor distribution of air, distension of the small intestine and colon, absence of air in pelvic gap, fluid and gas levels (Fig. 1).
Abdominal ultrasound was not available in the hospital at that time.
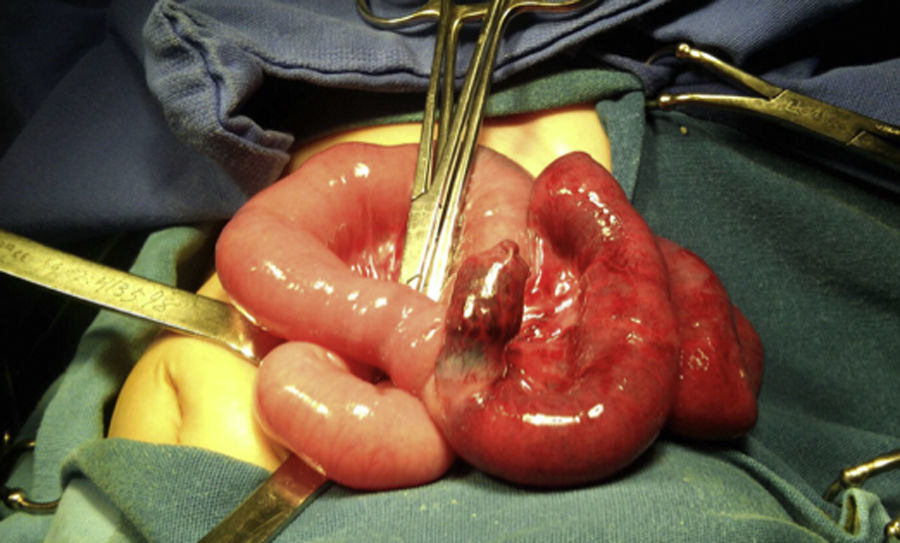
Surgery was performed under balanced general anaesthetic, installing a central line in the right subclavian area. Then an exploratory laparotomy was performed with right transverse infraumbilical incision, finding ileo-ileal intussusception, treated and resolved with taxis. The cause was a Meckel's diverticulum 1cm in diameter 50cm from the ileocaecal valve, with violet colour in the terminal ileum due to poor perfusion. Warm saline solution was applied to improve perfusion in the distal ileum (Fig. 2), with moderate improvement in colour. Intestinal resection and termino-terminal anastomosis on two planes with 4–0 suture. Resection margin 5cm distal and 5cm proximal to Meckel's diverticulum, with 5–0 chromic gut sutures in the mesenterium. An incidental appendectomy (Halsted) was also conducted, leaving Penrose 5/16 drain directed towards the anastomosis (Fig. 3).
Post-surgical management with gastric tube and fasting for 4 days, intravenous cefotaxime and amikacin for 7 days. Tube removed on 4th day and lactose-free diet on the 5th day after surgery. Oral diet was poorly tolerated and she presented 2cm distension of abdominal perimeter. X-ray showed no free air in cavity or intestinal occlusion. Metoclopramide was added to the treatment, with clear improvement, tolerating oral diet, with normal bowel movements, normal urination, vital signs within normal limits for her age. Penrose drain removed on 6th day after surgery due to reduced output of clear serous fluid. The sutures were removed 10 days after surgery.
The patient was seen as an outpatient 10 days after discharge and then after 4 months. She presented normal growth and development.
DiscussionIntussusception is one of the most common causes of intestinal obstruction in infants and children. Its incidence worldwide is 1–4 out of every 2000 infants and children. It is more common in boys at a ratio of 2:1 or 3:2. 75% of cases occur in the first 2 years of life.1
Intussusception caused by other conditions is 0.3% in neonates, increasing to 44% at 5 years and 60% at 5–14 years.
In infants, most cases are idiopathic. In only 2–8% of patients are there anatomical abnormalities that cause intussusception,3 the most common of which is Meckel's diverticulum, especially in children over 2 years of age and adults.2
2.5% of cases are ileo-ileal.1
Our case concerned a 3-month-old baby girl with ileo-ileal intussusception secondary to Meckel's diverticulum. This condition is very uncommon in female infants with an incidence of less than 2%.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo sponsorship of any kind was received for this paper.
Conflict of interestsThe authors declare that they have no conflicts of interest.