Spinal anaesthesia is a commonly used anaesthetic technique for transurethral resection of the prostate for its efficiency, speed, minimal effects on mental state, protection against thromboembolic complications, early mobilisation after surgery, minor respiratory complications, continuous analgesia and shorter hospital stay.
ObjectiveTo determine whether administration of hyperbaric bupivacaine in spinal anaesthesia in sitting position causes minor changes in blood pressure and heart rate compared to the lateral decubitus position.
MethodologyProspective, longitudinal, comparative, randomised study. A total of 50 patients were included in two groups. Group A (n=23) patients were administered 12.5mg of hyperbaric bupivacaine in the sitting position and the position was maintained for 5min. Group B (n=27) patients were administered 12.5mg of hyperbaric bupivacaine in lateral decubitus position. Blood pressure, heart rate, and levels and latency of sensory and motor block were compared. Descriptive statistics were used and analysed by Student's “t” test to compare the means of the values found.
ResultsThere were no significant differences in heart rate and systolic blood pressure. Diastolic blood pressure was higher in group A, showing a significant difference from 5min after administration of the block, with a significant difference in mean arterial pressure from minute 10. The onset of sensory and motor blockade was faster, and the level of sensitive block achieved higher, in group B. The regression of the motor block was faster in group A.
ConclusionsThere were significant differences in mean and diastolic blood pressure as well as onset of sensory and motor block with the sitting position. This proves that applying spinal anaesthesia in a sitting position involves less haemodynamic variation (heart rate and blood pressure) for elderly patients undergoing transurethral resection of prostate.
La anestesia espinal es una técnica anestésica comúnmente usada para resección transuretral de próstata por su eficacia, rapidez, mínimos efectos en el estado mental, protección contra complicaciones tromboembólicas, movilización temprana postcirugía, menores complicaciones respiratorias, continuidad de analgesia y disminución en estancia hospitalaria.
ObjetivoDeterminar si la administración de bupivacaina hiperbárica en anestesia espinal en posición sedente produce menores cambios en presión arterial y frecuencia cardiaca comparada con la posición decúbito lateral.
MetodologíaEstudio Prospectivo, Longitudinal, Comparativo y Aleatorizado. Se incluyeron un total de 50 pacientes, en dos grupos. Grupo A (n: 23) se le administraron 12.5mg de bupivacaína hiperbárica en posición sedente y fue mantenida la posición por 5 minutos. Grupo B (n: 27) pacientes se le administraron 12.5mg de bupivacaína hiperbárica en posición de decúbito lateral. Se compararon las cifras de presión arterial y de frecuencia cardiaca, así como los niveles de bloqueo sensitivo y motor y la latencia del mismo. Se realizó estadística descriptiva y se analizó mediante “t” de Student para comparar las medias de los valores encontrados.
ResultadosLas cifras de frecuencia cardiaca y presión arterial sistólica no mostraron diferencias significativas. La presión arterial diastólica fue mayor en el grupo A, mostrando diferencia significativa a partir de los 5 minutos de instalado el bloqueo, la presión arterial media muestra diferencia significativa a partir del minuto 10. El inicio de bloqueo sensitivo y bloqueo motor fue más veloz en el grupo B, así como el nivel más alto de bloqueo sensitivo alcanzado. La regresión del bloqueo motor fue más rápido en el grupo A.
ConclusionesEl aplicar al paciente anestesia espinal en posición de sentado, presenta menos variaciones hemodinámicas (frecuencia cardiaca y presión arterial) para pacientes ancianos sometidos a resección transuretral de próstata.
The social and economic importance of old age is related to the degree of dependence associated with being elderly.1 One of the factors that explains the rise in the population demographically is the increase in life expectancy; in 1970 this was 79.8 years for women and 79.1 years for men, by 2010 it had gone up to 83.3 for woman and 81.5 for men, and by 2050 it is expected to be 84.6 for women and 82.9 for men.2
Approximately one third of patients who undergo surgery are over 65 and one of the most common interventions is transurethral resection of the prostate.3 The ageing process is accompanied by a change in body mass, with a reduction in muscle and increase in adipose tissue. This is associated with a loss of lean body mass and a decrease in total body water, which can make it difficult to calculate the correct dosage for drugs. Increased adipose tissue increases the deposit of liposoluble medications, prolonging clearance and extending duration of action of drugs like benzodiazepines, volatile agents, opioids and hypnotics. In addition to this, many patients have malnutrition and therefore have low albumin levels, which leads to an increase in levels of free drug for those that are highly albumin-bound.4
Changes in the anatomy and physiology of a number of different organs also affect the use of medicines. In the kidneys, the renal parenchyma loses about 10% of its thickness per decade of life after the age of 40. Between the ages of 20 and 90, a decrease of 50% in renal blood flow contributes to a 30–50% reduction in the glomerular filtration rate. From the age of 50 onwards, there is a constant decrease in liver mass (20–40%), so by the age of 90, it only represents 11.6% of body weight. Hepatic blood flow slowly decreases (0.3–1.5% per year), reducing by up to 40% between the ages of 25 and 65. These changes affect the excretion of a large number of analgesics, sedatives and anaesthetics.5
Changes in autonomic function occur as a result of an increase in plasma catecholamine concentrations, the manifestation of which is, paradoxically, decreased heart rate. There is also a decrease in inotropism and chronotropism secondary to a reduction in vascular adrenergic receptors capable of responding to a stimulus; it becomes evident in the case of cardiovascular decompression under stress, causing a decrease in cardiac output. This tells us that elderly patients are more sensitive to changes in preload and fluid kinetics, due to the less effective response in the baroreceptors decreasing the capacity for response to haemodynamic changes.6
Both the central and peripheral nervous systems degenerate as we get older. These changes can have an impact on the characteristics of a central block and the pharmacology of local anaesthetics. A reduction in the number of neurons within the spinal cord, deterioration of the myelin sheaths and connective tissue barriers, changes in the anatomical configuration of the thoracic and lumbar spine, any reduction in the volume of cerebrospinal fluid and a decrease in conduction velocity in the peripheral nerves, especially motor nerves, can all alter the characteristics of the nerve block (dose/response ratio) after epidural or subarachnoid administration of local anaesthetics.7
In spinal anaesthesia, the extent of the block depends on the baricity of the solution. The effect of age on the maximum height of spinal analgesia with isobaric solution is marginal. Anaesthesia is more predictable with hyperbaric solutions, with spread in the direction of gravity and less interindividual variability, a higher level of sensory block (3–4 segments) and a more rapid onset of motor block.7
Studies with stable isotopes have shown that systemic absorption of local anaesthetics after epidural or subarachnoid administration is biphasic; a rapid initial phase followed by a much slower phase. In spinal anaesthesia, the initial absorption of local anaesthetics from the subarachnoid space is much slower than with epidural administration because of poor perfusion of the subarachnoid space and a lower drug gradient. It has been shown that systemic absorption of bupivacaine after spinal anaesthesia is faster in elderly patients due to a faster final absorption rate, with no reduction in the duration and compared to other ages.7
The increase in body fat can result in a larger volume of distribution of local anaesthetics. Toxicity is less predictable in elderly patients. The most important plasma protein to which local anaesthetics bind is alpha-1-acid glycoprotein (α1 GPA). The free fraction of lidocaine and bupivacaine is inversely proportional to the plasma concentration of α1 GPA. In the absence of disease, age causes modest effects on the concentration of α1 GPA.7
A reduction in plasma clearance of lidocaine and bupivacaine of up to 35% has been demonstrated in elderly patients, mainly in men >65, due to the fact that clearance of amide-type local anaesthetics is mainly undertaken by the microsomal hepatic metabolism. We must therefore exercise caution when administering local anaesthetics in large or repeated doses or in continuous infusion.7
Clinically, the elderly are more sensitive to the effect of local anaesthetics. A higher level of sensory block is observed after administration of spinal or epidural anaesthesia, suggesting that these changes are due to pharmacodynamic changes in intrinsic neuronal sensitivity. The incidence of hypotension is increased due to decreased cardiac reserve, changes in the arterioles and changes in the autonomic nervous system, as well as increased neuronal sensitivity and a greater degree of spread of the local anaesthetic. The mean absorption time for subarachnoid hyperbaric bupivacaine is shorter in elderly patients due to its second phase of rapid absorption.7
Complications include allergic or anaphylactic reactions, post-puncture headache, paraesthesia, paresis or dysaesthesia, accidental total spinal block, paraplegia, paralysis, neuropathy, arachnoiditis, hypotension, bradycardia, cardiac arrest, respiratory depression, nausea, vomiting, back pain, muscle weakness, urinary retention and urinary incontinence.7
Most patients having transurethral prostatic resection are elderly men who have heart, lung or some other type of comorbidity. To reduce the adverse haemodynamic effects associated with spinal block in these patients, reducing the dose of local anaesthetic has been recommended.8 Differences have also been found when the anaesthetic is administered in a sitting position compared to the lateral decubitus position, because the drug settles at a lower level, but without compromising the quality of the blockade.
ObjectiveTo determine whether administration of hyperbaric bupivacaine in spinal anaesthesia in sitting position causes minor changes in blood pressure and heart rate compared to the lateral decubitus position.
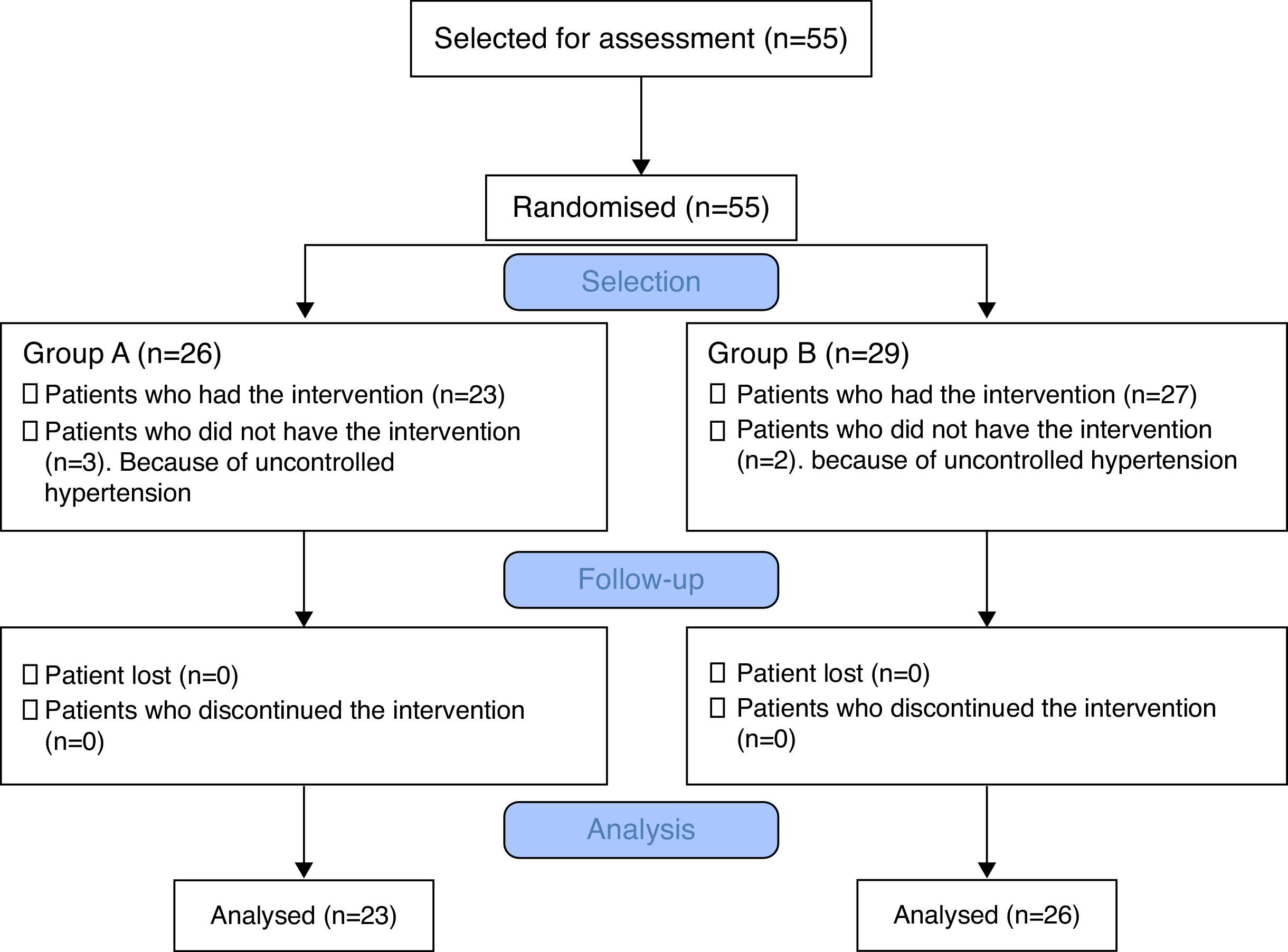
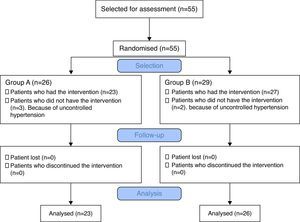
MethodsThe study was conducted as a clinical trial (prospective, longitudinal, comparative, randomised). After approval by the Hospital General de México (HGM) research ethics committee (authorisation code: DI/15/203/02/29), 50 patients scheduled for transurethral resection of prostate in the HGM Urology Pavilion, with risk classification for anaesthetic procedure ASA I–II and signed informed consent were included in the study and divided into 2 groups to receive spinal anaesthesia in a sitting position or lateral decubitus position. Patients found to have uncontrolled hypertension on arrival at the operating theatre were excluded.
The sample size was calculated using the statistical program Epi Info v7, with a difference in the means for independent groups; calculating both tails, taking as object of study a decrease in blood pressure of 20% out of 100%, for a confidence level of 95% and a test power of 80%, a sample size was estimated for each group of 23 patients. Adding a further 10%, the result was 26 patients per group. They were distributed into each group by simple randomisation performed with the Excel program.
On arriving in the operating department, the patient was assigned according to the simple randomisation table in accordance with the theatre in which the intervention was scheduled. The anaesthetic procedure and data collection were performed by the anaesthetist assigned to that theatre. The patient's heart rate, respiratory rate and non-invasive blood pressure, 5-lead electrocardiogram in lead II and V5, pulse oximetry and temperature were monitored. Patients in group A were then placed in a sitting position and patients in group B in lateral decubitus position. After application of antiseptic to the dorsolumbar region and placement of sterile fields, spinal block was performed (subarachnoid space) in interspace L2–L3, with Whitacre 22G needle, with 12.5mg (2.5ml) of hyperbaric bupivacaine at a rate of 0.2ml/s over about 10s. After injection of the local anaesthetic, the patients in group A (n=23) remained in a sitting position for 5min and were then placed in a supine position. With the patients in group B (n=27), the block was done in the lateral decubitus position and they were immediately placed in a supine position after the injection of local anaesthetic had been administered. Heart rate, non-invasive blood pressure, respiratory rate and oxygen saturations were measured at 3min intervals for the first 15min following administration of local anaesthetic, and then every 5min until completion of the surgical intervention. In the event of hypotension (systolic blood pressure <90mmHg or a decrease in systolic blood pressure, diastolic or mean >20% from baseline) 5mg intravenous ephedrine was administered, repeated every 5min if the blood pressure figures did not recover. Episodes of bradycardia (heart rate <50beats per minute) were treated with intravenous atropine 10mcg/kg body weight. Haemodynamic stability was considered when these values remained above 50bpm for heart rate and blood pressure did not decrease by >20% compared to baseline. The level of sensory block was determined with a blunt needle prick every 2min to establish the maximum level of block after 4 consecutive tests. The time to onset of sensory block, the maximum upper level of block, the time to reach the maximum upper level of block and duration of the blockade were recorded. In the recovery room regression of motor block was measured by modified Bromage scale every 20min until patient transfer.
The flow chart for the methodology is shown in Fig. 1.
Statistical methodsThe SPSS v. 22 statistical program was used for data analysis. Time (in minutes) from the application of the local anaesthetic to the maximum decrease in heart rate, systolic, diastolic and mean blood pressure are presented as mean and standard deviation (SD); Kolmogorov–Smirnov normality test was applied, assuming equal variance with the Levene test. The data were then analysed with Student's t test for two-tailed independent samples.
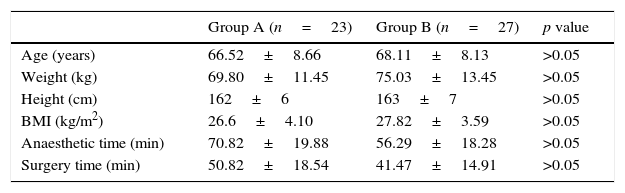
ResultsThe patients’ demographic characteristics were similar in the two groups. Anaesthetic time was slightly longer for the patients in group A; however, for the purposes of our study, only the data up to 60min was recorded (Table 1).
Patient characteristics and anaesthetic and surgery times.
| Group A (n=23) | Group B (n=27) | p value | |
|---|---|---|---|
| Age (years) | 66.52±8.66 | 68.11±8.13 | >0.05 |
| Weight (kg) | 69.80±11.45 | 75.03±13.45 | >0.05 |
| Height (cm) | 162±6 | 163±7 | >0.05 |
| BMI (kg/m2) | 26.6±4.10 | 27.82±3.59 | >0.05 |
| Anaesthetic time (min) | 70.82±19.88 | 56.29±18.28 | >0.05 |
| Surgery time (min) | 50.82±18.54 | 41.47±14.91 | >0.05 |
Data are expressed as mean plus standard deviation.
kg: kilograms; cm: centimetres; BMI: body mass index; min: minutes.
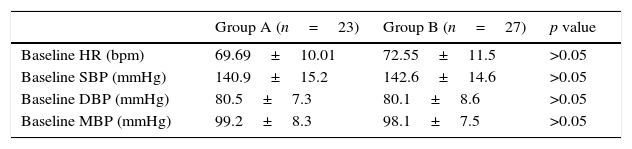
There were no statistically significant differences between the two groups in baseline vital signs (Table 2, p>0.05).
Baseline vital signs between group A (sitting) and group B (lateral decubitus).
| Group A (n=23) | Group B (n=27) | p value | |
|---|---|---|---|
| Baseline HR (bpm) | 69.69±10.01 | 72.55±11.5 | >0.05 |
| Baseline SBP (mmHg) | 140.9±15.2 | 142.6±14.6 | >0.05 |
| Baseline DBP (mmHg) | 80.5±7.3 | 80.1±8.6 | >0.05 |
| Baseline MBP (mmHg) | 99.2±8.3 | 98.1±7.5 | >0.05 |
Data are expressed as mean plus standard deviation.
HR: heart rate; SBP: systolic blood pressure; DBP: diastolic blood pressure; MBP: mean blood pressure; bpm: beats per minute; mmHg: millimetres of mercury.
There were statistically significant differences between groups in heart rate after drug administration at 20 (p=0.034) and 25 (p=0.008) min, with a maximum decrease of 8.85% in group A and 18.99% in group B. No patients in group A required administration of atropine to increase heart rate. Only one patient in group B required the administration of atropine to achieve a heart rate greater than 50beats per minute.
There was no statistically significant difference between groups in systolic blood pressure (SBP) after administration of the drug. The maximum decrease in SBP from baseline was at 25min in group A (16.7%) and 20min in group B (21.38%), with no significant difference between the two groups being found when comparing the time of maximum decrease (p>0.05).
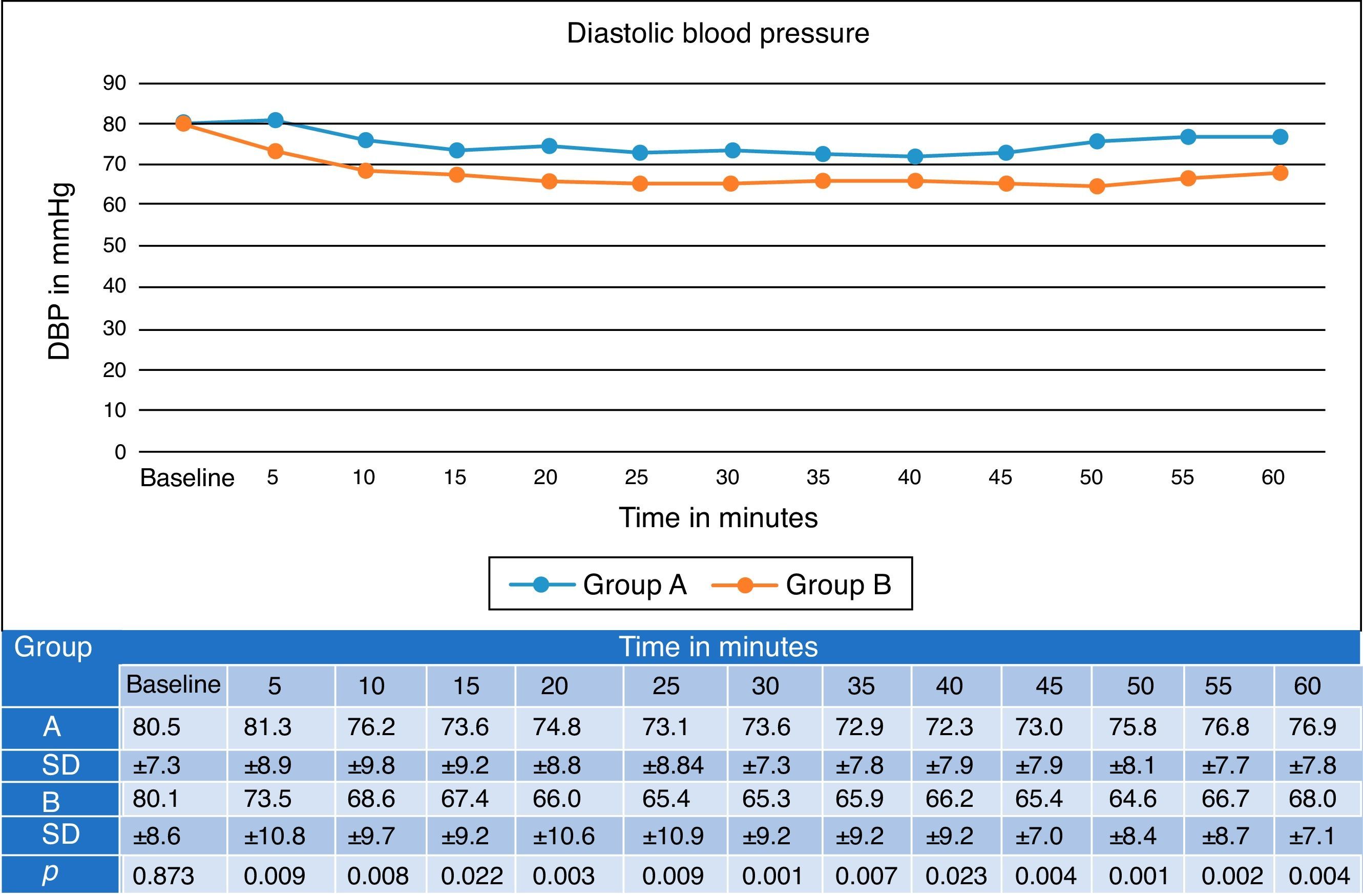
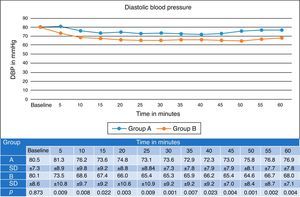
Diastolic blood pressure was higher in group A at all time points after the block, with lower values in all cases in group B and the differences being statistically significant from minute 5 after administration. The maximum decrease was 10.18% in group A and 19.35% in group B (Fig. 2).
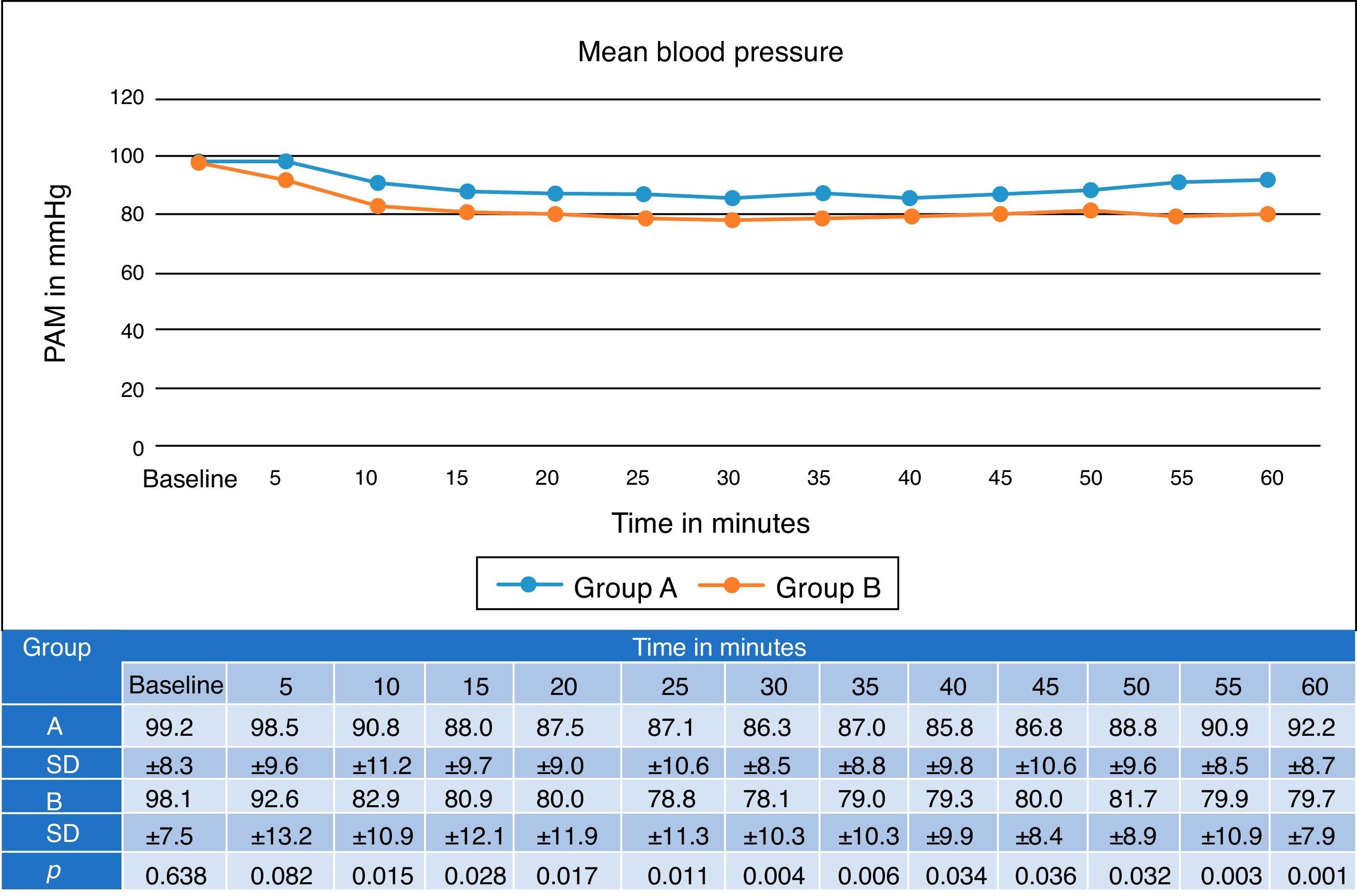
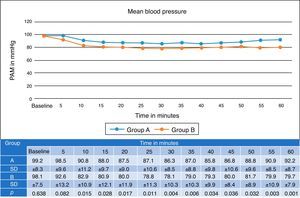
Mean arterial pressure values were statistically significant from minute 10 after administration of the block, with lower figures in group B. There were no reports of mean blood pressure below 60mmHg in either group. The maximum decrease in group A was 13.5% and in group B, 20.38%. Administration of ephedrine was necessary in two patients in group B for lowering of blood pressure which compromised the patient's haemodynamic status. None of the patients in group A required ephedrine (Fig. 3).
The onset of sensory block in group B (164±27.99s) was faster than in group A (200±32.78s), the difference being statistically significant (p<0.001), and that correlating with the faster and more marked decrease in blood pressure in group B.
The highest dermatome sensory block level achieved in group A was at 40min after injection of local anaesthetic and in group B, 30min. These results correlate with the lower mean blood pressure detected at the same time points, with the level achieved in group A always being lower; the differences were statistically significant difference at all time points up to 60min (p<0.05). None any of the patients in either group suffered a drop in oxygen saturation or ventilation-related problems as the sensory block did not reach beyond the T4 dermatome level.
In group A, onset of motor block was different in all patients, but was achieved in most cases by minute 30. In group B, all patients had motor block at 15min and all continued to have complete motor block at minute 60, with the difference statistically significant up to minute 15 (p<0.05). In the recovery room, regression of the motor block was faster in the patients in group A, with regression on the modified Bromage scale of 0 at 120min, while patients in group B had still not achieved total regression of the motor block at 140min.
DiscussionBenign prostatic hyperplasia (BPH) is a common condition among older men, and transurethral resection of prostate is the method of choice for prostates of intermediate volume between 30 and 60cm3.9 Spinal anaesthesia is preferred for its efficiency, speed, minimal effects on mental state, reduced blood loss, protection against thromboembolic complications, early mobilisation after surgery, minimal respiratory complications, analgesia and short hospital stay, and the fact that it allows a lower volume and dose of anaesthetic to be used, reducing the risk of toxicity.
We studied 50 patients undergoing transurethral resection of prostate at Hospital General de México “Eduardo Liceaga”. Baseline vital signs were measured every 3min for the first 15min and then every 5min until the end of surgery; the results tables show every 5min and they are only reported up to 60min into the block since, as discussed in the article by Veering et al.10, hyperbaric anaesthetic can take up to 60min to “take hold” and after this period, it is highly unlikely that major changes in vital signs or in the intensity of the block will be due to the effect of the local anaesthetic.
The characteristics in terms of age, weight, height and BMI were similar in both groups, with no statistically significant differences. Only patients with ASA physical status I and II were included; 5 patients were excluded from the study because when entering the operating theatre, they were found to have very high blood pressure, making it impossible to proceed with the surgery.
There were no statistically significant differences in heart rate. By group, there were no heart rate figures below 50beats per minute; only one patient in group B required atropine to maintain a heart rate above 50beats per minute.
Sistolic blood pressure was higher in group A at all time points except baseline, but there were no statistically significant differences. Diastolic blood pressure was also higher in group A, showing a significant difference from 5min after administration of the block, with a significant difference in mean arterial pressure from minute 10. These changes can be attributed to the fact that in group B, the level of sensory block was higher, indicating that the sympathetic blockade, which is regularly 2–4 segments above the level of analgesia, occurred more frequently in group B. In 2 patients in group B, but none in group A, ephedrine had to be administered to increase blood pressure.
The onset of sensory block was faster and reached higher dermatomes in group B than in group A. The motor block was also more intense in group B. The regression of the blockade in the recovery room occurred earlier in group A, which allowed patients to be returned more quickly to their hospital beds.
In our study, the time at which the maximum decrease in mean blood pressure occurred in group A was minute 40, which is consistent with the results obtained by Veering et al10, who found a maximum decrease of 20% in blood pressure in patients similar to our group A. For the sensory block, similar figures were found at minute 20 and for the maximum block achieved using 12.5mg, in our case, versus 15mg of hyperbaric bupivacaine. We had a sample of 23 patients compared to the 15 patients per group reported in their study. In contrast to their conclusion, we found that the position did influence the distribution of hyperbaric local anaesthetic in the subarachnoid space when comparing a sitting position to lateral decubitus, and that a period of 5min is appropriate for limiting that distribution, without causing significant delay to the anaesthetic/surgical procedure.
According to the metameric level of sensory block reached in our study and comparison with the study by Guang Han et al.,11 the sensory levels found in our study were higher, and always higher in group B, with statistically significant differences at all time points. Guang Han et al. report statistically significant differences only up to minute 15. In our study, statistically significant differences were found in the diastolic blood pressure from minute 5 and the mean blood pressure from minute 10, similar to the data found in the Guang Han et al. study, where statistically significant differences were found in mean blood pressure from minute 10 to minute 30 after application of the local anaesthetic. Neither study found statistically significant differences in heart rate.
Our study is supported by a study by JD Kelly et al.,12 which reports a more marked decrease in systolic and mean blood pressure in patients placed in supine position immediately after spinal block than in the group of patients left for 30min in the lateral position, while at the same time, the level of sensory block was higher on the dependent side than on the non-dependent side, showing that the most effective “settling” of the local anaesthetic is dependent on position.
Limitations of the study include the fact that it was carried out on a single population (in this case TURP patients) and only included male patients, so it is not possible to extrapolate to other populations. One bias that was identified was the fact that the study was only single-blind, since the patients were not informed which group they were in, but it was the anaesthetist who administered the drug who collected the information.
ConclusionsSpinal anaesthesia in sitting position promotes cardiac and cerebral perfusion in elderly patients, and can reduce intraoperative stress. In this study, the sitting position was adopted for 5min, and resulted in significant differences in diastolic and mean blood pressure, as well as in the onset of sensory and motor block, proving that applying spinal anaesthesia in a sitting position involves less haemodynamic variation (heart rate and blood pressure) for elderly patients undergoing transurethral resection of prostate. Our plan is to enlarge the sample size to achieve greater accuracy in the results.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThere was no external funding for completion of this article.
Conflict of interestsThe authors declare that they have no conflict of interests.
The full protocol is available on the website of the UNAM central library under the title “Comparison of haemodynamics in spinal block with hyperbaric bupivacaine in a sitting versus lateral decubitus position for transurethral prostatectomy”.