In abdominal trauma, spleen is the most commonly injured abdominal organ. Spleen injuries can be managed in three modes: splenectomy, nonoperative management and splenorrhaphy, all based on the scale of severity of splenic injury of the American Association of Trauma.
ObjectiveTo determine the incidence of splenic injury and management at the Balbuena General Hospital according to the severity scale of the American Association of Trauma.
Materials and methodsAn observational, descriptive and retrospective study was conducted in patients attending at the General Hospital Balbuena with splenic injury in abdominal trauma, in the period from January 2010 to December 2014, excluding all patients under 18 years old, with splenic injury.
ResultsWere found a total of 59 cases of patients with splenic injury. Of the total population 84.7% splenectomy was performed, 85% of cases were male and 15% female. The group with the highest number of cases of splenic lesion was found in the range from 20 to 29 years, representing 28.81%. Of the study population 55.93% are blunt abdominal trauma.
ConclusionThe blunt abdominal trauma remains one of the most common causes of splenic injury. The clinical status of the patient, the degree of hypovolemic shock, the degree of splenic injury and associated injuries are the guidelines on the type of approach and treatment in patients with splenic injury. Today the blunt abdominal trauma with severe splenic injury is the most frequent indication for splenectomy.
En el trauma de abdomen, el bazo es el órgano abdominal lesionado con mayor frecuencia. Las lesiones de bazo pueden ser manejadas en tres modalidades: esplenectomía, esplenorrafía y manejo no quirúrgico, basado en la escala de severidad de daño esplénico de la Asociación Americana de Trauma.
ObjetivoConocer la incidencia de la lesión esplénica y su manejo, en el Hospital General Balbuena, según la escala de severidad de la Asociación Americana de Trauma.
Material y métodoSe realizó un estudio retrospectivo observacional y descriptivo en pacientes que acudieron al Hospital General Balbuena, con lesión esplénica en traumatismo abdominal, en el periodo de enero del 2010 a diciembre del 2014, en el cual se excluyó a todos los pacientes menores de 18 años con lesión esplénica.
ResultadosSe encontraron un total de 59 casos de pacientes con lesión esplénica. Del total de la población, en el 84.7% se realizó esplenectomía; el 85% de los casos fueron del sexo masculino y el 15% del sexo femenino. El grupo con mayor número de casos de lesión esplénica se encontró en el rango de 20-29 años, representando 28.81% del total de individuos. De la población estudiada, la mayor proporción (55.93%), corresponde a traumatismo cerrado de abdomen.
ConclusiónEl trauma cerrado de abdomen sigue siendo una de las causas más frecuentes de lesión esplénica. El estado clínico del paciente, el grado de choque, el grado de lesión esplénica y las lesiones asociadas, son las directrices en el tipo de abordaje y tratamiento en el paciente con lesión esplénica. Hoy en día, el trauma cerrado de abdomen con lesión esplénica severa es la indicación más frecuente para esplenectomía.
The World Health Organisation estimates that by 2020, trauma will be the primary cause of losing years of productivity for the global population.1 In centres that specialise in trauma, abdominal lesions are distributed into four compartments: intra-thoracic abdominal, central abdominal, retroperitoneal, and pelvic. Intra-thoracic abdominal lesions are the most common and the spleen is located in this compartment. The spleen is the abdominal organ most frequently injured in blunt abdominal trauma2; in open abdominal trauma, it is in sixth place.3
The diagnostic and therapeutic approach to patients with spleen injuries has evolved significantly. Initial resuscitation along with FAST ultrasound (Focused Assessment with Sonography for Trauma) or Computerised Axial Tomography (CAT), are the image studies indicated for detecting spleen injury in patients exhibiting minimal signs, and form part of current spleen injury management guidelines, providing three modes of treatment: non-operative management, splenectomy, and splenorrhaphy.4
The decision for non-operative management is based on the patient's request upon resuscitation with liquids and haemodynamic monitoring.5,6 However, the presence of one of the following criteria: evidence of haemodynamic instability during monitoring, characterised by hypotension; increased haemoperitoneum evidenced by ultrasound, and haematocrit reduction; the presence of active bleeding requiring the transfusion of more than 4 units of blood in the first 24h; development of complications; and patients who reject conservative treatment, is an indicator of emergency surgical treatment.7
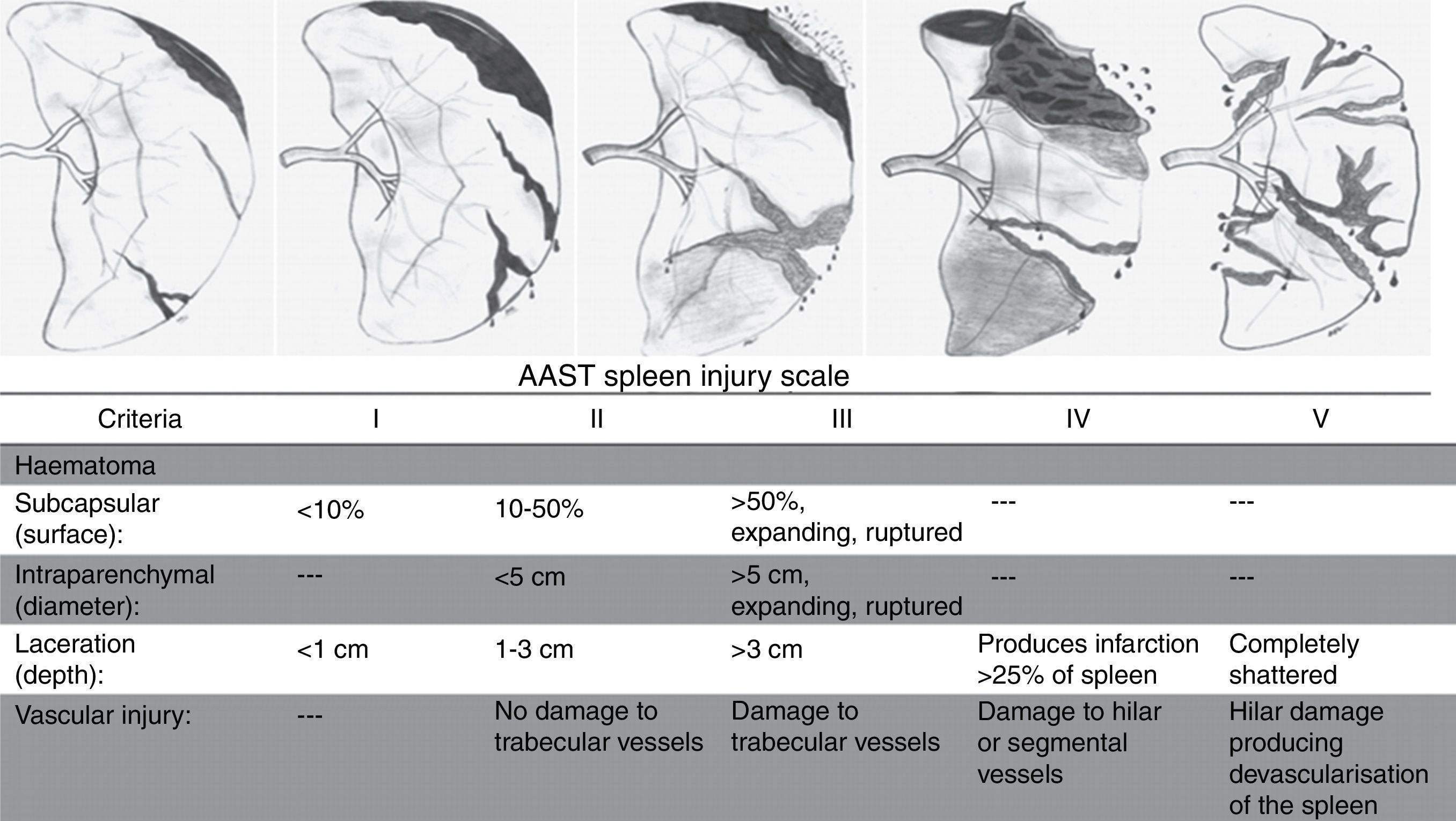
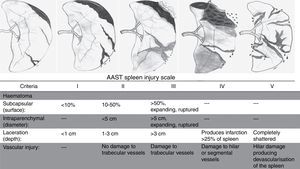
The decision to perform a splenectomy, partial splenectomy or splenography and the type of approach is relative to the degree of injury, according to the Spleen Injury Scale of the AAST (American Association for the Surgery of Trauma).8Fig. 1, American Association for the Surgery of Trauma Spleen Injury Scale.
With the surge of laparoscopic surgery, blunt trauma cases have been reported in which a laparoscopic approach has been used, particularly for partial splenectomies. Evidence, however, has not yet reached acceptable standards; in addition, the procedures have only been performed on haemodynamically stable patients with injuries below Grade III, according to the AAST scale.9,10
When splenorrhaphy is decided upon, it should be performed by an experienced surgeon skilled in the technique, using absorbable sutures 2-0(8). Blunt abdominal trauma with severe spleen injury is the most common indication to date for performing a splenectomy, and open splenectomy continues to be the main surgical option in emergencies and for grade IV and V injuries.9,11
MethodA retrospective observational and descriptive study was carried out that included all patients who attended Hospital General Balbuena between 1 January 2010 and 31 December 2014 with abdominal trauma, and who were diagnosed with some grade of spleen injury, according to the criteria of the AAST spleen injury scale. All patients under 18 years of age who were diagnosed with spleen injury were excluded.
Eleven variables were measured in this study: age, gender, type of abdominal trauma, injury mechanism, injury site, degree of shock upon admitting the patient, degree of injury diagnosed during the surgical event, treatment of the spleen injury, associated injury by organ, number of deaths, and length of hospital visit.
A database was created using the SPSS (Statistical Package for the Social Sciences) programme for data analysis. Frequency, averages and percentages of the cases presented were determined, the results were organised and graphic representations were drawn up for interpretation of the data.
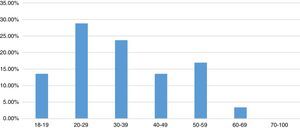
ResultsA total of 59 cases presented spleen injury due to abdominal trauma between January 2010 and December 2014 at Hospital General Balbuena. Of the 59 cases, 9 (15.25%) occurred in 2010, 18 (30.51%) in 2011, 16 (27.12%) in 2012, 11 (18.64%) in 2013 and 5 (8.47%) in 2014. Of the 59 spleen injury cases, 9 cases (15%) were female, while 50 cases (85% of this population) were male.
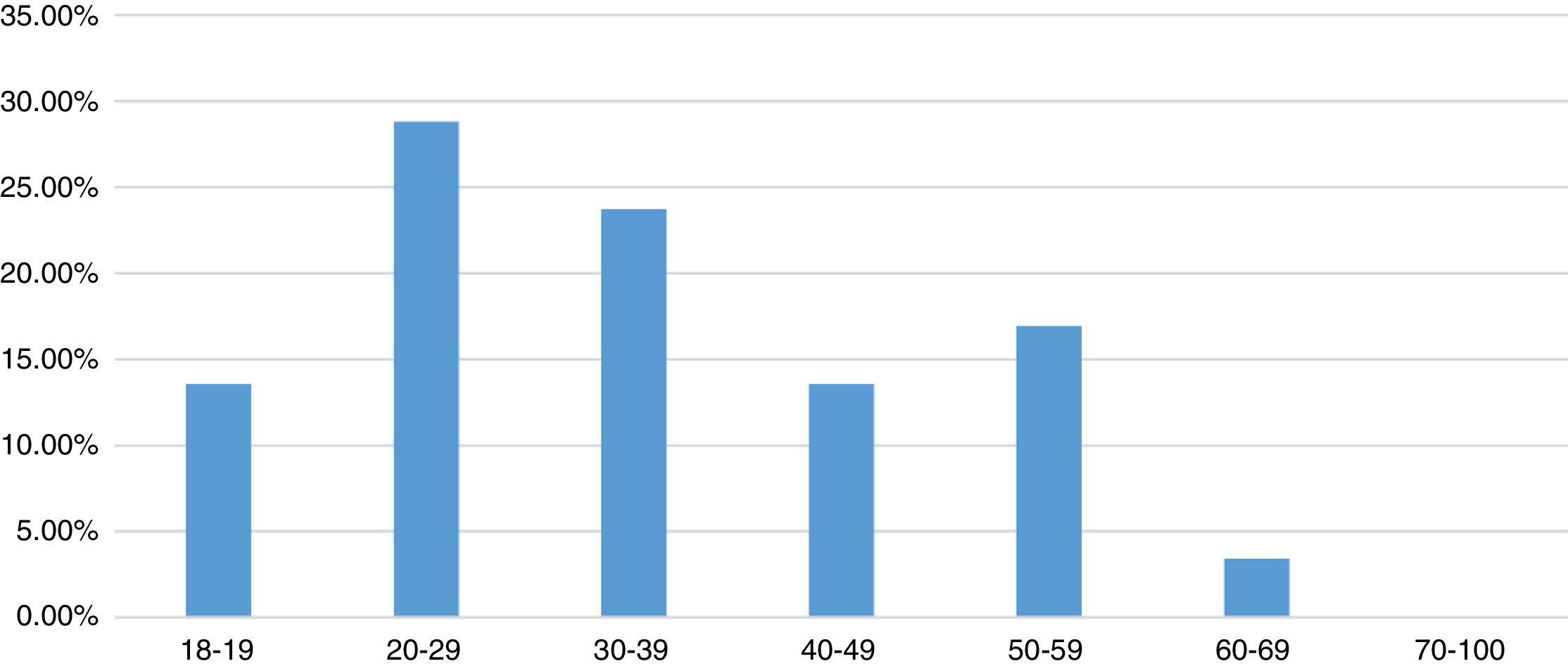
7 groups were formed based on age range: from 18 to 19 years of age, with 8 cases (13.56%); 20–29 years of age, with 17 cases (28.81%); 30–39 years of age, with 14 cases (23.73%); 40–49 years of age, with 8 cases (13.56%); 50–59 years of age, with 10 cases (16.95%); 60–69 years of age, with 2 cases (3.39%) and over 70 years of age with zero cases (Fig. 2).
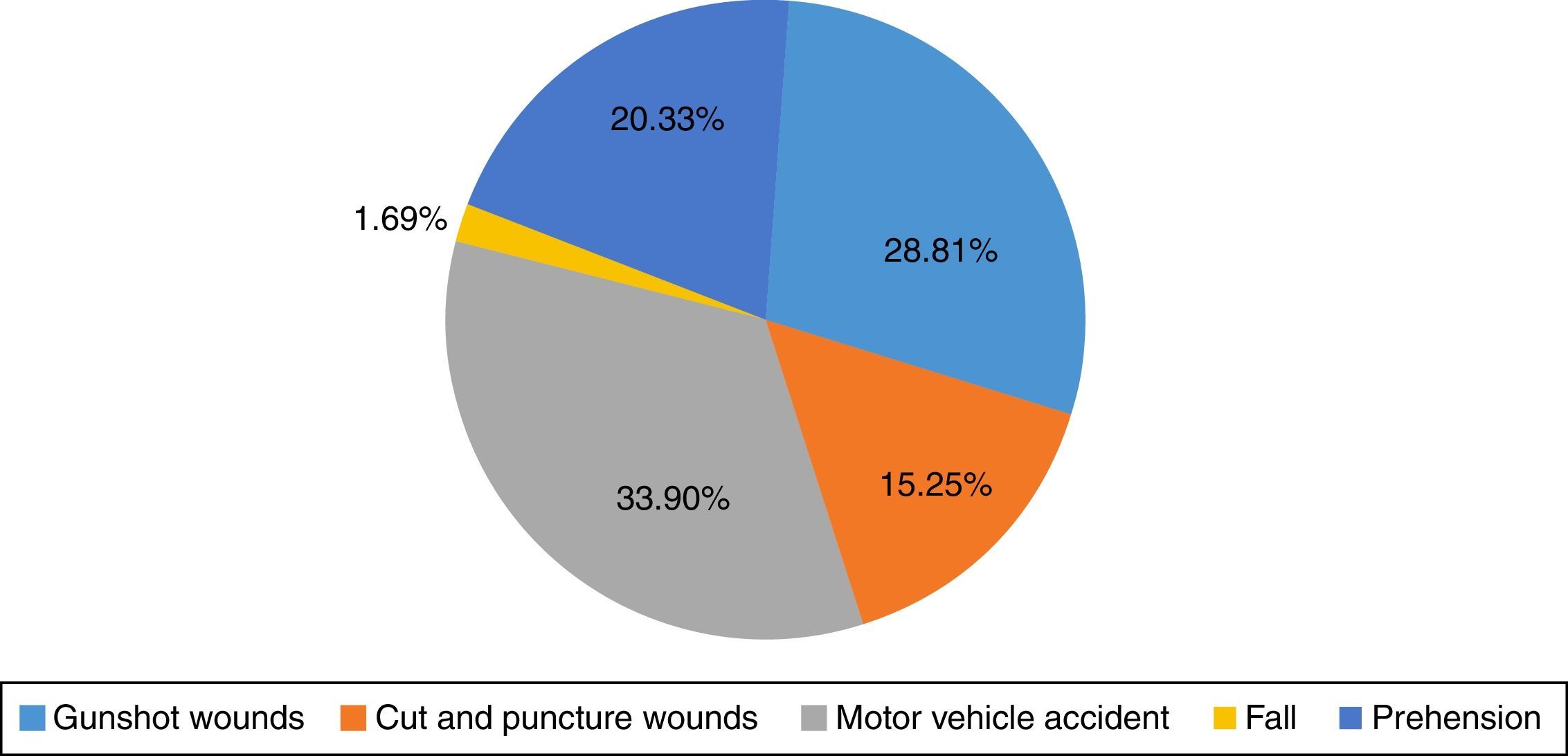
In the population studied, 33 cases presented with blunt abdominal trauma (55.93%) and 26 cases were secondary to open abdominal trauma (44.06%).
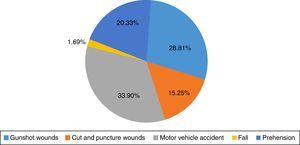
Of all the study subjects, 17 were admitted for GSW (28.81%); 9 cases due to puncture wounds (15.25%); 20 (33.9%) were admitted following a motor vehicle accident; 12 patients (20.33%) secondary to falls from varying heights; and only one case due to prehension (1.69%) (Fig. 3).
From the time patients were admitted to A&E until undergoing surgery, it was reported that 25.42%, or 15 patients, presented with grade I hypovolaemic shock; 32.20%, or 19 patients, presented with grade II hypovolaemic shock; 11.86%, or 7 patients, presented with grade III hypovolaemic shock; and 18 patients, or 30.51% of the population, presented with grade IV hypovolaemic shock; taking haemorrhaging into account as of their assessment in A&E and the cumulative balance by the anaesthesiology department.
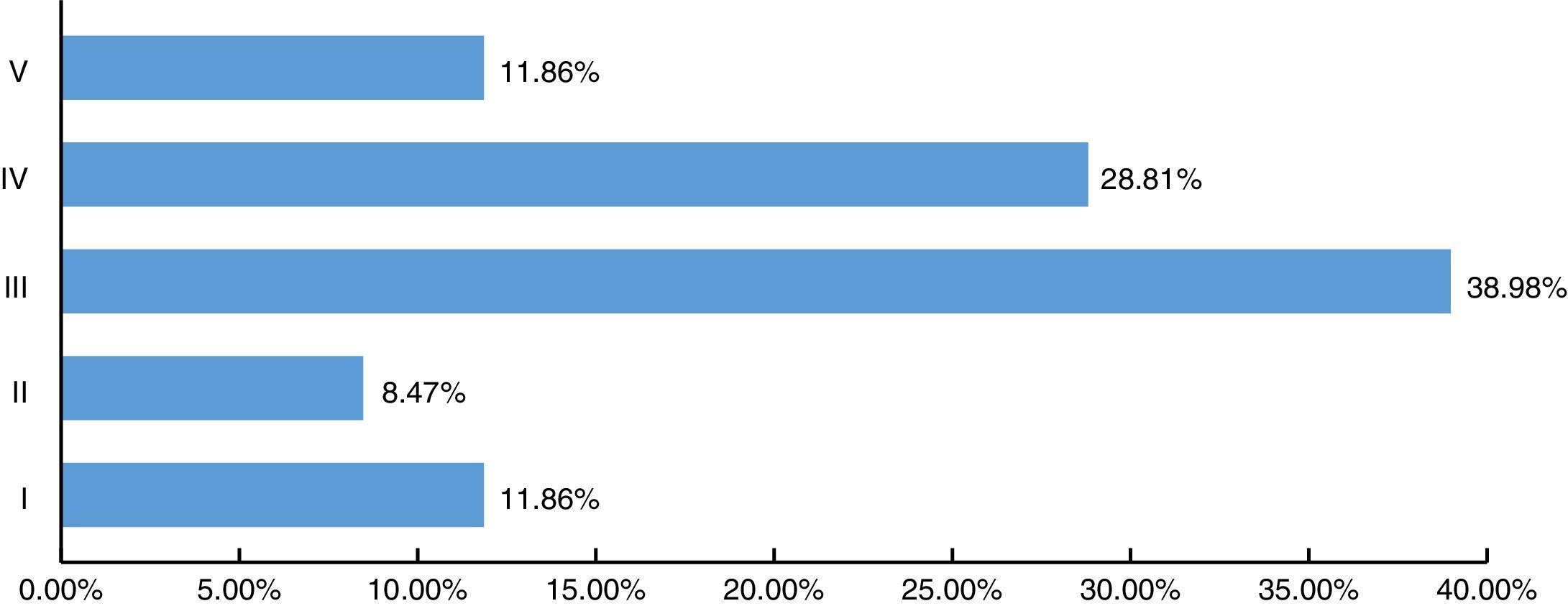
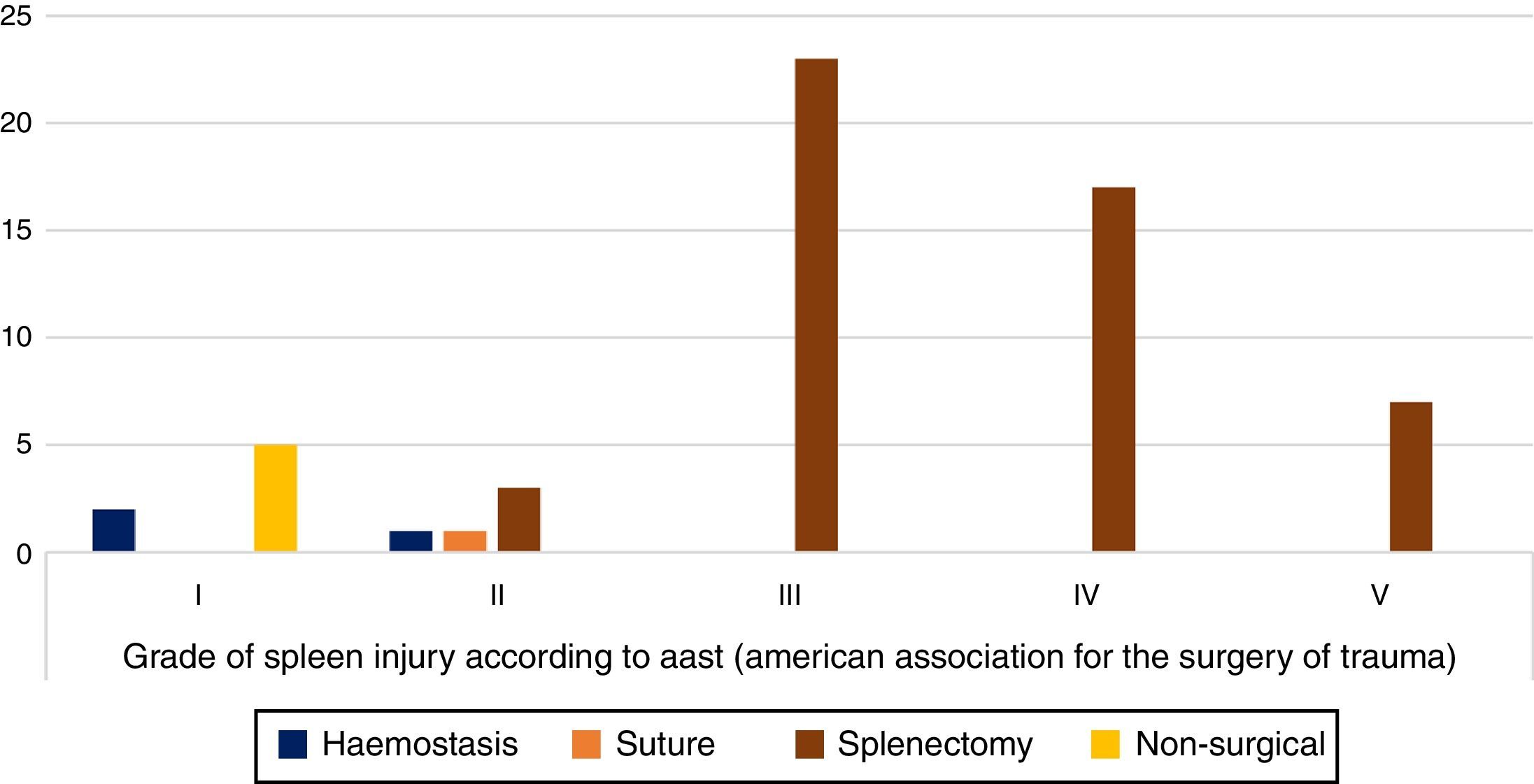
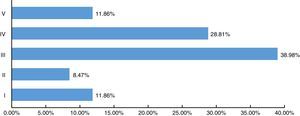
According to the AAST spleen injury scale, of the 59 cases reported: 7 corresponded to grade I (11.86%), 5 cases grade II (8.47%), 23 cases grade III (38.98%), 17 cases grade IV injury (28.81%) and 7 cases grade V injury (11.86%) (Fig. 4).
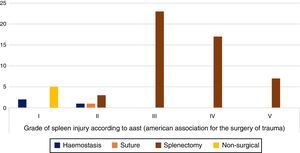
Of the patients with grade I injuries, 2 patients received haemostasis while the remaining 5 did not receive any therapeutic treatment to the spleen; in patients with grade II injuries, haemostasis was applied in 1 case, splenorrhaphy in 1 case and splenectomy in 3 cases; of the 23 grade III cases, splenectomy was performed in 100% of cases; for grade IV injuries, splenectomy was performed on 17 patients, representing 100% of the cases; in the 7 cases with grade V injury, splenectomy was performed in 100% of the cases. Splenectomy was performed in 50 of the total number of cases, representing 84% of the patients studied (Fig. 5).
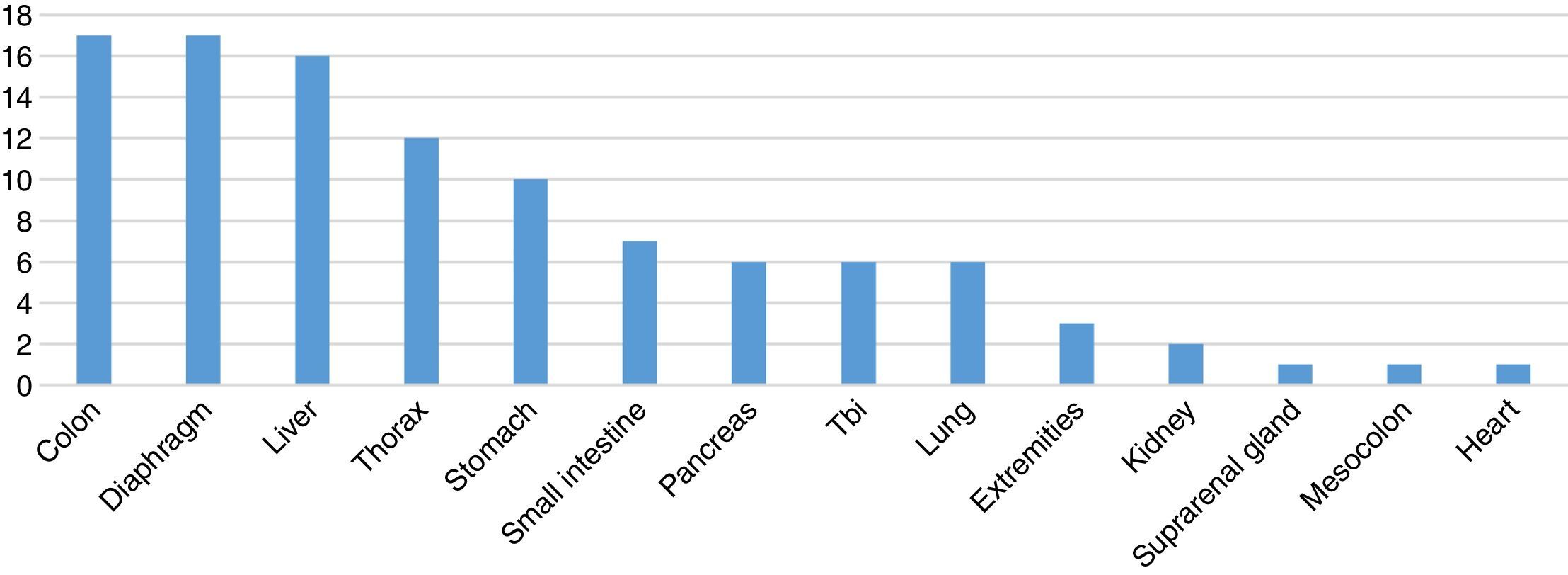
Of the 59 cases studied, 6 patients (10%) presented with isolated spleen injury and of the remainder, 53 patients (90%) presented another type of injury associated with another organ.
Of the 53 patients with an associated injury, 19 (35.6%) presented an injury other than the spleen injury; in 15 of the cases (28.30%), two types of associated injury were found; a further 15 cases (28.30%) presented three types of injury other than that of the spleen; and 3 cases (5.66%) presented four or more injuries other than that of the spleen.
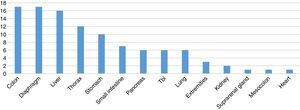
In spleen injuries associated with one or more concomitant injuries, the following was reported: 17 cases with a colon injury, diaphragm injury in 17 cases, liver injury in 16 cases, injury to the thoracic cavity in 12 cases, stomach injury in 10 cases, small intestine injury in 7 cases, pancreatic injury in 6 cases, traumatic brain injury (TBI) in 6 cases, lung injury in 6 cases, injury to the extremities in 3 cases, associated with kidney injury in 3 cases, associated with bladder injury in 2 cases, suprarenal injury in 1 case, mesocolon injury in one case and heart injury in one case (Fig. 6).
Of all 59 cases of spleen injury, deaths following surgical treatment were reported in only 12 patients; of these cases, 3 corresponded to a grade III injury, 6 cases to a grade IV injury, and 3 cases to a grade V injury. More than two associated injuries were seen in all the deaths reported and none with an isolated spleen injury. Causes of death were: 6 cases with pneumonia associated with health care, 1 patient with heart injury, 3 patients secondary to severe traumatic brain injury and 2 patients secondary to grade IV hypovolaemic shock.
DiscussionIn our series, males were most affected, representing 85% of all cases. Furthermore, in 31 of the 59 reported cases, the greatest number occurred during the productive years, between 20 and 39 years of age.
The type of abdominal trauma, the haemodynamic state of the patient when being assessed in the emergency room and the potential associated injuries were the main indications for performing an immediate exploratory laparotomy. It should be mentioned that, at our institution, in spite of being a reference site for trauma surgery, we do not have computerised tomography or ultrasound 24h a day, and therefore the decision to perform surgery is based on the patient's clinical state.
It was during the systematic exploratory laparotomy that the spleen injury was identified along with its grade. More than 60% of patients throughout this review presented with a spleen injury of grade III or higher on the AAST scale, with grade III being the most prevalent. Following splenectomy, 12 patients were reported as having died.
During the exploratory laparotomy, the decision on the type of surgical treatment to perform was made, initially based on the AAST spleen injury scale, the patient's haemodynamic state and the number of associated injuries.
Upon reviewing similar studies, it was reported that in Medellín, 25.6% of patients required immediate surgery. The decision to provide surgical management upon admittance was based on the haemodynamic state of the patient and signs of peritoneal irritation, without needing to use other diagnostic methods. Total splenectomy was performed in 71.4% of cases, followed by splenorrhaphy (28.6%), which was successful in 5 of the 6 patients.12
Meanwhile, in a multicentre study in Spain, treatment was initially surgical in 56.6% of cases, with the remaining 43.4% being conservative. Of these, 6.5% eventually needed surgery and in 8.8%, splenic angioembolisation was performed. Of the patients initially treated, splenectomy was performed in 85.3% of cases and conservative spleen surgery (splenorrhaphy and mesh) in 14.7%, of which 4.6% failed and required additional surgery with splenectomy.13
The decision between surgical and non-surgical treatment depends on a careful analysis of the risks and benefits for each patient, as well as on the experience of the surgeon and the hospital's multi-disciplinary team.14 Compared with other series, the percentage of patients receiving splenectomies is similar; in our study, total splenectomy was performed in 84% of cases and splenorrhaphy in only 1.69% of cases. The knowledge of the different injury mechanisms and the proper assessment of patients will allow the surgeon to formulate an accurate diagnosis and select surgical or expectant management to prevent or significantly reduce potential complications.15
ConclusionOur results regarding the injury mechanism are comparable to those reported in different series in which blunt abdominal trauma predominates over open abdominal trauma. However, in contrast to various research studies in which a grade IV or V injury are the main indication for splenectomy, we were able to observe that the indication for splenectomy centres not only on the grade of spleen injury, but also on the patient's haemodynamic state and the various associated injuries that presented in each of the patients and the type of organ affected.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.