Psychiatric neurosurgery or psychosurgery remains as an alternative for treatment of psychiatric disorders. However, its historical antecedents, the vulnerable specific condition of psychiatric patients, the high cost of instrumentation and the ethic dilemma about the autonomy of subjects whose are candidates to this kind of procedures condition to get a interdisciplinary and specialized staff and at less supervision for ethic local committee. There are ablative or deep brain stimulation procedures accepted as compassionate or investigational use. Into systematic review four International Ethic Guides are accepted for the indication, the implantation and the follow up of these treatments. 24 bioethics essays were found them and 9 ethics specific dilemmas were published. Expectancy and development of this medical issue are inherent to financial or biotechnological aspects, consequently is important to promote a scientific and philosophical discussion.
La neurocirugía psiquiátrica ó psicocirugía continúa siendo una alternativa de tratamiento para las enfermedades psiquiátricas. Sin embargo, sus antecedentes históricos, el estar dirigida a una población vulnerable, los altos costos de instrumentación y el dilema sobre la autonomía del sujeto a decidir sobre este tipo de cirugía, condicionan a que estos casos sean abordados por equipos interdisciplinarios, altamente especializados y al menos bajo la supervisión del Comité de Etica de la institución donde se realicen. Existen procedimientos ablativos y por estimulación eléctrica cerebral profunda, los primeros aceptados como tratamiento de uso compasivo y los segundos se encuentran en fase de investigación. En la revisisón sistemática existen 4 guías éticas internacionales aceptadas respecto a la indicación, la aplicación y el seguimiento de estos tratamientos. 24 ensayos éticos fueron encontrados y 9 dilemas éticos fueron publicados. Las expectativas y el desarrollo de esta rama médica están inherentemente ligadas a la aplicación tecnológica, así como a los aspectos financieros, por lo que es importante desarrollar una discusión científica y filosófica del tema.
Neurosurgery has been applied as a treatment to solve psychiatric disorders since the beginning of the past century. In its origins, this chapter of neurological surgery was denominated as Psychosurgery, today this term has been replaced by Psychiatric Neurosurgery or Neurosurgery for Mental Disorders; however, they still handle differently. Why is neurosurgery considered as an alternative in the treatment of mental disorders? Fundamentally because of four reasons: The high prevalence of psychiatric diseases and their social repercussions,1–5,8 the existence of a group of patients refractory or hard to control with conventional methods whether adjuvant pharmacologic or therapeutic (physical or psycodynamical),1,6–13 the abundance of information regarding the physiopathologic brain substrate of mental disorders and the remarkable technological development that has transformed neurosurgery in a safer and more precise speciality. However, neurosurgery for mental disorders must be revised from the ethical and moral perspective. In this essay we will evaluate some ethical and legal considerations regarding the use of psychiatric neurosurgery.
Historical backgroundPsychosurgery was defined by the World Health Organization as: “The selective surgical resection or destruction of the neural pathways or normal brain tissue, in order to modify the behaviour”.14 Neurosurgery for the treatment of psychiatric diseases might be one of the most controverted scientific activities of the twentieth century. In the beginning of humanity, trephine (based in mystical and magical aspect rather than scientific) was the first attempt of surgical treatment for psychiatric disorders. Later on, in the anecdotic case of Phineas Cage, clinically described by John Harlow in 1860, demonstrated that lesions of the frontal structures produced disinhibition of social learned conducts.15 Because of the absence of psychopharmacological treatments, in 1888, Gottlieb Burckhardt a Swiss psychiatrist performed the first surgical procedures in psychiatric patients with the anatomic and physiologic theories of that time. Burckhardt treated patients with behaviour alterations, “eliminating or diminishing” the areas of brain with pathologic behaviour. On December 29 of 1888, he performed the first topectomy and in 1891 published his experience with six patients described as demented and aggressive, mentioning three important successes, two partial results and a failure that led to the patients’ death.16
At the start of the twentieth century, the psychiatric effects induced by injuries in the frontal lobes on wounded soldiers of the First World War revealed new information. In 1935 Fulton and Jacobsen, presented, in the Second World Congress of Neurology in London, their works performed on chimpanzees, detailing the changes on behaviour after frontal lobectomy. These experimental findings on non-human primates encouraged the possibility to influence, via surgical procedures, the control of psychiatric disorders.17
Thus, the series of events that led to the massive development and use of psychiatric neurosurgery, during the fifties, cannot be appreciated without the comprehension of the political and social environment that surrounded the psychiatric disease at the start of the century. Psychiatrics and neurologists were the responsible for taking care of these patients. The number of psychiatric patients incremented according to the population growth and these patients were secluded on mental institutions and asylums. It must be noted that the debate between Sigmund Freud against the functional approach that Emil Kraeplin presented, regarding mental disorders, induced psychiatrists to become independent from the medical branch, which explains why neurologists involved themselves more in the diagnosis and treatment of patients with mental diseases. In fact, neurologists rather than psychiatrists were the ones who became the strongest supporters of psychosurgery, given that, generally, the patients from that time received years of psychotherapeutic treatment and “somatic therapies” (such as induced coma, by insulin or metrazol, and electroconvulsive therapy), without achieving the adequate therapeutic effects nor social readjustment.13
Properly speaking, it was Egas Moniz who “started” psychosurgery on humans when he proposed to the scientific community the surgical interruption of the front-thalamic tract a cross of bifrontal burr holes. Egas Moniz and Almeida Lima performed more than 100 prefrontal leucotomies and despite their data never being systematized nor having any clinical follow up, in 1949 he received the Nobel Prize in Physiology and Medicine for his work “Prefrontal Leucotomy”.18,19 These works encouraged American neuropsychiatrist Walter Freeman together with neurosurgeon James Watts to “optimize” the original procedure from Moniz-Lima and instead of performing frontal trepans to approach the front-thalamic tract, they would apply an alternate approach by supraorbital via, denominating it “frontal lobotomy” applying an surgical instrument similar to “ice pike”. Unfortunately, this procedure was massively applied, in the United States and around the world, for any kind of mental illness, without achieving specific beneficial results, so in 1955 more than 50,000 surgeries had been realized. Psychosurgery was then considered as a set of highly invasive surgical procedures. Frontal and temporal lobectomies were stigmatized by their poor efficiency, high risk of collateral damage and limited scientific basis.20
Functional stereotaxic neurosurgery was born in the first third of the twentieth century, due to the lack of pharmacological treatment for functional neurologic diseases such as movement disorders, epilepsy, pain and psychiatric diseases. The main objective of this general neurosurgery branch was to perform minimal injuries, in specific sites (nucleus or tracts), thus achieving equilibrium of neural activity. The theories of James Papez and the contributions of Paul Mac-Lean, made that the cingulum, the amygdala, the hypothalamus and the thalamus were recognized as important components of a regulatory system for emotions and instinctive conduct, hence, being adequate sites for the chirurgical treatment of mental disease.21 Nowadays, the following neuronal structures are identified as chirurgical sites for the treatment of psychiatric diseases: the anterior cingulum, the subcaudate tract, the anterior limb of the internal capsule, the hypothalamus, the mammillary bodies, the fornix, the subgenual region, the accumbens nucleus, the amygdala and the subthalamic nucleus.22
In 1954, the pharmaceutical company Smith, Kline & French received the approbation by the Food and Drugs Administration for the use of antipsychotic drug denominated chlorpromazine.19 By the end of 1954, the chlorpromazine had already been administrated in more than 2,000,000 mentally ill patients in the United States, establishing with it the premise that “drugs were effective and safer that psychosurgery”, bringing an end to the first stage of psychosurgery.23
Psychosurgery still produces fear in many countries for it is considered it could be used as a mean of political or social control.24 Despite the severe restrictions and public denounces, psychosurgery continued and continues being performed restrictively in the United States. On the other hand, countries like Mexico, Brazil, Finland, Sweden, England, Spain, India, Italy, Germany and Belgium allow the performing of these procedures with humanitarian purposes. Psychiatric neurosurgery is prohibited in Japan, France, El Salvador and Australia.
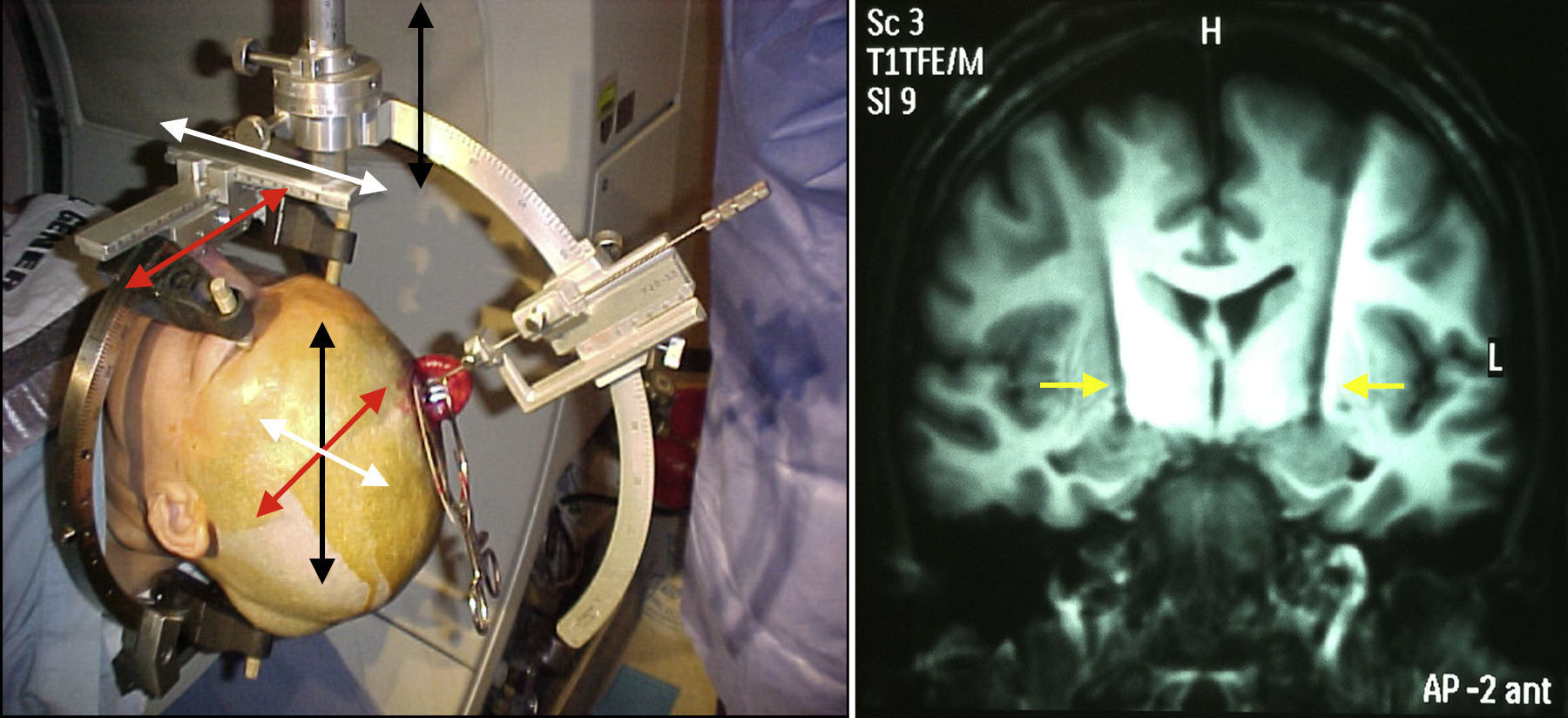
Non stereotaxic psychiatric neurosurgery from the first half of the twentieth century was characterized for being unspecific, highly invasive and mutilating, performed with the use of craniotomies, frontal and temporal lobectomies and, more refined, front-thalamic leucotomy by trepans and by trans-orbital via. On the second half of the twentieth century, stereotaxic psychiatric neurosurgery proved to be very precise based on the polar or cartesian localization (Fig. 1), reproducible by the milimetrical human brain atlas, with scientific bases using well defined physiological concepts and performing proof of electric stimulation before to perform a lesion (confirm the result prior to use thermo-coagulation with radiofrequency). Ablative neurosurgery is less known and entails humanitarian purposes when applied on patients, under the bioethics concept of the less damage possible to improve the functional result, and has been a common practice in many developed and undeveloped countries.
In this picture on left side it is showing a stereotactic procedure. The head of patient is fixed inside of Cartesian coordinates system (X: red, Y: black, Z: white) in order to localize a specific target through a burr hole in the skull. Prior the coordinates were found out by software that analyzed magnetic resonance and CT-scan images. Right side shows two electrodes into basal ganglia (yellow arrows).
Deep brain stimulation has (DBS) has been an efficient and save alternative for the treatment of chronic neurologic diseases such as epilepsy, Parkinson's’ disease and neuropathic pain (Fig. 2).10 Since 2002 the first informs regarding the use of DBS on psychiatric diseases have been published, more concretely in respect to the treatment of mayor depression disorder8,10,25 and obsessive-compulsive disorder.8,10–12,25 In short time, other psychiatric disorders were included such as Tourette's syndrome, violent behaviour, nervous anorexia, addiction to substances and other neuropsychiatric disorders such a dementia.9,10,25–27 The main advantage of DBS lies on the possibility to “module the brain function” in such a way that it leads to the desired clinical effect and avoid collateral effects; its action mechanism different from the stereotaxic selective lesion allows the possibility to liberate a dose of electric current on anatomic structures very circumscribed using a combination of amplitude, frequency and duration of the electric impulse.25 The main disadvantage of DBS is the cost that limits in almost all the world its application and could even be considered an ethical dilemma.
Despite the increase of scientific papers discussing this subject, the present evidence, even for the mayor series, is still incipient and DBS for this kind of disorders is still considered an experimental treatment. Additionally, the number of randomized and masked clinical essays designed for DBS in mental disorders is small. This is justified because proposing a “placebo” manoeuvre over a neurosurgical procedure would be ethically questionable. However than DBS offers the possibility to effectuate clinical trial with a “sham” arm, if it is consented to the individual subjected to the study to be included randomly on a transitory period without electric stimulation to later be subjected to DBS therapy. In any case, the increasing interest in this area of neurosciences has encouraged the establishment of specific ethical guides. The more broadly diffused is the one published on 2009 by Rabins et al. In it specific aspects are taken into account, such as considering all scientific evidence preclinical and clinical before performing a new research project with DBS, not forgetting the historical experience regarding the unmeasured and uncontrolled use of this therapy, establishing very specialized and interdisciplinary work teams, assuring the wellbeing of the research subjects not only in their clinical conditions but also in their wellbeing and quality of life, establishing a sustainability program of the DBS therapy that assures the patients the possibility to continue with their treatment specially when this has had a beneficial effect, maintaining supervision over the work groups of the local ethical committees on research to ensure the observance of research subjects rights and continuing clinical studies with more evidence regarding the effects and action mechanisms of DBS.28
Schermer in 2011 published than DBS practice is structured in the four basic principles of medical ethic: (1) Non-maleficence, “first do no harm” (to calculate risk, physical and psychical side effects, to avoid personality changes or developing brain). (2) Beneficence, “do well” (effectiveness and need of psycho-social cares), (3) Proportionality and subsidiarity, “risks and benefits in proportion,” “choose least burdensome alternative?” and “refractory to others treatments”, (4) Justice, “treat like cases alike” respect patients’ well-informed choices” (rationing and prioritizing, inform consent, avoid desperation and unrealistic expectation, competence to consent and special evaluation in minors).29
The aim of this review was to analyzed the ethical and regulatory aspects of psychiatric neurosurgery.
Method and materialFor this review the authors made a bibliographic research looking up non-mesh combination terms: ethical issue AND psychosurgery; ethical issue AND psychiatric neurosurgery; ethical considerations AND psychosurgery and ethical considerations AND psychiatric neurosurgery. Limits were English or Spanish language, 10 years prior to searching (from 2005 to 2014), abstract available, containing statements about ethical discussion or regulatory issues about psychosurgery. Further analysis in order to find papers shared in different searchers. The information was classified to present ethical discussion for specific surgical procedures, ethical or regulatory aspects and ethical dilemmas. Exclusion criteria were containing animal model information or unspecific conclusion.
ResultsInitially, this searching strategy allowed finding 77 studies. 29 papers completed inclusion and exclusion criteria. Four articles were guide or regulatory works.40–42 Twenty-four were ethical discussion18,38,43–65 and 9 ethical dilemmas.46,66–74
More important essays included: Consensus on guidelines for stereotactic neurosurgery for psychiatric disorders, published in 2014 where is commented about the necessity of increase the level of evidence and design randomized blinded clinical trials in order to get information of ablative or DBS procedures. Always is mandatory to observe to enhance patient safety. Expert committee conducted this study.
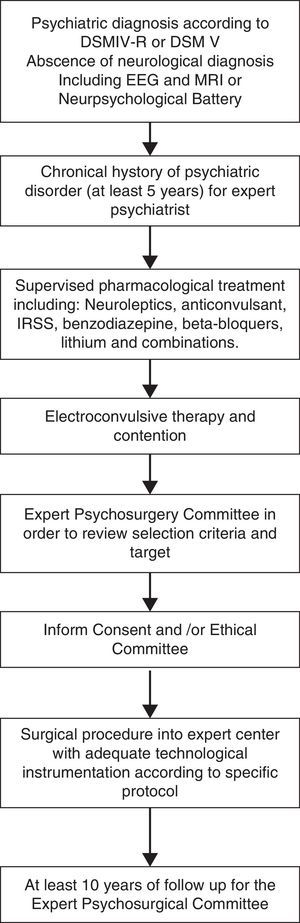
Algorithm of study and treatment of this kind of patients was proposed in Fig. 2.
DiscussionPsychosurgery has many aspects to be analysed from the bioethical point of view. One of these, as mentioned before, is the controversial history of the first half of the twentieth century. Psychosurgery had its origin in a moment in which there were no psychopharmaceutic treatments and the only option to treat psychiatric signs was surgery. The fact that an operation alleviated the psychiatric symptoms was the motif that gave the Nobel Prize to Egas Moniz during the thirties and both society and the scientific community validated these therapeutic procedures. Yet, despite the evident lack of clear indications for its application, the beneficial results sometimes not very tangible and the great quantity of secondary effect of psychiatric neurosurgery of the fifties, Dr. Freeman was convinced that what he was doing was helping patients in their suffering, always acting under the principle that his patient could improve. However, the acting of Dr. Freeman and other neurosurgeons created a tension in society clearly reflected in movies like One Flew Over Cuckoo's Nests. Despite scientific data of the beneficial effect of psychosurgery when performed specific indications, stereotaxic techniques and radiofrequency, the social pressure made the United States Congress to limit the use of psychosurgery, thus, for a few decades, only some areas in the American Union allowed these procedures. Something similar happened in other countries. In Japan, professor Narabayashi was taken out from the back door of the hotel in which he presented some of his data, for a crowd nearly lynched him. From heaven, by receiving the Nobel Prize, to hell, with limitations that almost extinguished the procedure. Two events provoked the stigmatization of psychosurgery: The rise of psychopharmaceutic, which allowed the control of the symptomatology, and the ethical disdain of avoiding to fall in the hands of neurosurgeons apparently without scruples. Is very valid to make a reflexion to consider the real ethical dilemma regarding surgical techniques and the physiopathology of psychiatric diseases during these period. Unfortunately, up to this point no animal model will suffice to understand the physiopathology of every human mental disorder. In consequence, the neurosurgical treatment of psychiatric disorders was and will be many times extrapolated from the experience of the neurosurgeon during the treatment of other diseases such as Parkinson's, dystonia or the very mental disease. Despite the possible limitations of psychiatric neurosurgery; if used correctly the ethical principle of the lesser bad, psychosurgery was and is preferable to having patients in which no concrete therapy can be offered (Table 1).
This table shows main targets and their indications for psychiatric disorders by original authors.
| Author | Indication | Anatomic structure | Year | Improvement | Side effects |
|---|---|---|---|---|---|
| Gabriëls30 | OCD | IC | 2003 | 44–59% | None |
| Sturm31 | OCD | NAc | 2003 | Significant | None |
| Jiménez32,33 | MDD/OCD | ITP | 2005/2009 | 100/50% | Anxiety |
| Mayberg34 | MDD | Area25 | 2005 | Sustained remission | None |
| Visser-Vandewalle35 | Tourette | InLThN | 2006 | Significant | Hypomania |
| Mallet36 | OCD | STN | 2008 | 32% | Edema, bleeding and infection |
| Kuhn26,27 | Addiction alcohol/tobacco | NAc | 2007/2009 | 100/20.30% | None |
| Wu37 | Anorexia | NAc | 2013 | 85% | None |
Another aspect to analyse is the one implying the coexistence of relatives with a psychiatric patient without adequate or refractory control. The practice has demonstrated that certain aggressive patients with mental retardation have provoked a wear syndrome on their relatives, very common on personal working in chronical and psychiatric hospitals. Psychosurgery has diminished auto and hetero aggression, thus preventing injuries to the patients and others. Every time a psychiatric patient is proposed for a surgical procedure that improves their psychiatric symptoms, its case must be presented to a Hospital Committee of Bioethics or to a Committee of Research Ethics, depending on the case, and the rights and wellbeing of the patient must be evaluated same as his reinsertion on familiar, social and, if possible, working life.
The best ethic model for this kind of problems remains punctually projected only to man. The great advantages of DBS in comparison with stereotaxic brain lesions has produced a very important resurgence of psychiatric neurosurgery; the reversibility of the effects that avoids direct damage over the neurons or the fibbers, the adjustment of electric parameters by telemetry from the outside without need of invasion to the patient with the exception of placing the system and the versatility regarding the stimulation programs, make the new implantable systems able to help patients. Yet again the counterpart of disadvantages emerges, which could become real ethical dilemmas: an DBS system is very expensive, with costs that go from 17 to 33 thousand dollars only for the equipment, adding the cost of medical assistance and follow up.
Which psychiatric patients can be candidates to this type of treatment? In the case that this could be consider a therapeutic alternative in state of art and not only an experimental alternative: Could systems of a social or private security accept that psychiatric disorders are a valid surgical indication? There are some research projects, like in the case of Tourette's syndrome, where four stimulators in different targets have been placed, which complicates considerably their use. Additionally, the lifespan of the pulse generator or battery is very limited and can vary, because depending on the clinical improvement is how the parameters are adjusted, mainly in amplitude. It has been reported that batteries can last from one to six years before a change is needed; therefore their replacement will be limited to a good medical expenses insurance that covers said equipment, or else, to the existence of donations to the matter. It is also needed a good expert medical team in the area to monitor the patient.
Another important bioethical question emerges, one aspect is to diminish the psychiatric symptoms and another is to modify thoughts and feelings of the patient. This aspect is more tangible. One thing is to manipulate only neurophysiologic sensitivity and motor skills, and another is to modify cognition or will. In the case that a depressed patient that has had various suicidal attempts DBS seems to be justified. In a patient with obsessive compulsive behaviours the actual evidence seems to prove that its functionality depends on the implantation and the equipment effect, again psychosurgery seems justified.
Koivuniemi and Otto published this year a paper that discusses the meaning of “Mind Control” in the context of DBS. They postulate three conditions that can clearly define what in the context DBS would mind control mean: The criteria of results that implies an objective change in the behaviour of the stimulated subject, the criteria of approval which means that the subject in question has not manifested its approval for the DBS to modify his behaviour and the third criteria would be of intention, this means that the researcher manifests that he intentionally looked for that change in the behaviour.38 These three criteria have not been present in any case up to now. However, in the case of the patients that cannot manifest their approval for the change of behaviour like in patients in vegetative state where Yamamoto has stimulated the thalamus to improve their vigilance state, or in cases in which the researcher finds a collateral effect that could be beneficial yet not the one desired (in 2007 Khun tried to diminish the anxiety of an alcoholic patient stimulating the accumbens nucleus and what he obtained was a diminishment in the desire to consume alcohol).27 On these cases if the researcher does not informs the patient, once observed the unexpected effect, we could talk about mind control.
Yet, this type of therapy opens the door to other collateral aspects. Is it ethic or moral the neuromodulation in order to increase the executive capacities not only of patients but also from sane subjects? This aspect of DBS is denominated “enhancement”. Is it licit to use certain brain areas to manipulate behaviours, which could be the case of placing electrodes in the amygdala and by stimulating this area favouring braver soldiers during battle? Could a modulation be placed that makes a person submissive? There is a whole bioethical discussion that can barely be seen.39
The purpose of bioethics is to encourage the reflexion in which individuals understand that the most important is the respect and dignity of people. Some years ago it was unthinkable that through an electrode thoughts could be modified, nowadays, this is a reality. Is technology bad? No; technology is nor good nor evil, it depends on how it is used and who uses it to make man complement what is more important as a prerogative after life, which is his freedom. However, in the case of psychosurgery is fundamental to understand that many of these patients are “tied” to a psychiatric disease that undermines their consciousness and thus limits their freedom.
Finally, psychosurgery opens another possibility: trans-humanism, meaning, the colocation of prosthesis or attachments that replace lost functions. The Cyborg neologism, conceptualized as a cybernetic organism, makes allusion to this fact. When a patient is implanted with a brain electrode, technology that tries to recover a function that is no more is being applied. Here could enter all science fiction literature that has generated in the last fifty year regarding human being that have become half robot half human beings. The bioethical discussion on this point is also very important.
Psychosurgery remain been a medical, social and philosophical challenge that must not forget the most important aspect which is the comprehension of the disease and the observance of the subjects’ human rights per se, maxim in a psychiatric patient.
Conflict of interestThe authors declare that they have no conflict of interests.
Fiacro Jiménez Ramírez for translation service.