¿ Introduction
Pediatric cerebral palsy (PCP) is a permanent non-progressive disorder of movement and posture caused by cerebral injury at the development stage.1 It has the first place on the list of disability problems during childhood. Two thirds are associated with mental disability and 50% to 60% to visual disorders and strabismus.2 The first articles about the treatment (and follow up) of strabismus with botulinum toxin (BT) in children were done by Scott starting in 1980, where he mention treating endotropy and exotropy even with previous surgery.3
The strabismus treatment in children with PCP is difficult due to their overall health condition. Frequently, these children have motor skills disorders and severe systemic complications that lead to sensory and motor deterioration.4,5 Neurologic instability and the disorders of the cortical and subcortical control centers are destabilizing factors of the surgical outcomes that result in hypercorrections in the medium and long term. These results can be attributed to the poor fusion potential.6
Several studies have described the harmlessness and therapeutic usefulness of the botulinum toxin for several types of strabismus, such as congenital endotropy, intermittent constant exotropy and paralytic strabismus.7 Other less studied field is strabismus in patients with systemic diseases and psychomotor delay; where variable angle and vertical strabismus are described as more frequent4,8 and with PCP are described as less frequent.8,9
¿ Objective
To assess the results obtained after the treatment of strabismus in patients with neurologic deterioration, with systemic motor disorders and with different degrees of mental disability that delay or make impossible the surgical treatment.
¿ Methods
Prospective clinical study with self controls done between July 2008 and January 2010. All patients signed informed consent forms and the study was approved by the research council. Children of all ages that came to an ophthalmology appointment were included. Each one of them was fully evaluated by a rehabilitation specialist and they also had a previous diagnostic of PCP associated with horizontal strabismus, with or without mental disability and with any type or extension of the cerebral injury and the disability degree.
All patients underwent a full ophthalmologic examination to assess: visual acuity (using optotypes for verbal children who cooperate), visual conduct profile, fixation of luminous stimuli and of different objects (for children who do not cooperate).10 Patients were grouped according to the WHO (World Health Organization) visual acuity classification: normal or better (20/60); subnormal (20/70 - 20/200); severe deterioration (< 20/200 of size perception); and blindness (no perception of light).11,12 This last class was an exclusion criterion. The type of strabismus, endotropy or exotropy was assessed by alternate cover and cover-uncover tests; and its severity was measured in prismatic dioptres with the Krimsky method, evaluating fixation preference and muscular balance. In cooperative children we also performed the following tests: biomicroscopy, ophthalmoscopy, slit-lamp examination under cycloplegia with 1% cyclopentolate and full refraction tests.13
Based on their IQ score, the patients were classified by the International Classification of Diseases 10th Revision (ICD-10) in the following way: Mild mental retardation (MR), IQ range 50 to 69 (in adults, mental age from 9 to under 12 years); Moderate MR, IQ range of 35 to 49 (in adults, mental age from 6 to under 9 years); Severe MR, IQ range of 20 to 34 (in adults, mental age from 3 to under 6 years); Profound MR, IQ under 20 (in adults, mental age below 3 years).11
PCP was classified according to posture, motor control and functional activity limitation.1,14
All the children underwent strabismus treatment with BT type A diluted at 5 IU/0.1 mL.
Application technique: the BT was infiltrated under sevoflurane sedation, with previous instillation of topic tetracaine in the eye being treated, after transconjutival muscle identification, direct application with 27 G needle and without electromyographic guide at the following dose: 5 IU in the horizontal rectus muscle for strabismus below 20 dp, in the medial rectus for endotropy and in the lateral rectus for exotropy. In strabismus of 20 - 40 dp 5 IU were used in the two horizontal rectus muscles: medial rectus for endotropy and lateral rectus for exotropy. For strabismus above 40 dp we used 7.5 IU and 5 IU in horizontal rectus muscles for the non-fixating and the fixating eye respectively. The patients were summoned back for an assessment appointment at 2, 4, 6 and 12 months after treatment to measure the angle deviation and to undergo a second and third dose after the sixth month according to the size of an angle above 15 dp. The frequencies of the patients' characteristics were described with averages, standard deviation and proportions. The averages of numeric dependent variables were compared before and after treatment with Student's t-test for related samples. We evaluated the response to treatment according to age, type of strabismus, visual acuity, degree of MR and degree of PCP disability with ANOVA. SPSS Ver.19 was used for statistical analysis.
¿ Results
Forty five patients were included in this study: 21 (46.7%) were male and 24 (53.3%) were female, the age range being between 1 and 18 years old and the mean age of 7 years old. The minimum follow up period was 1 year.
The PCP motor assessment revealed: anatomic presence of quadriparesia in 35 patients (77.8%) and the most frequent; followed by diparesis in 8 (17.8%), hemiparesis in 1 (2.2%) and paraparesis in 1 (2.2%). According to the type of injury, the spastic type had the highest incidence in 34 patients (75.6%), followed by the hypotonic type in 4 (8.9%), the dyskinetic type in 3 (6.7%), ataxic and mixed types in 2 patients respectively. According to the degree of disability to perform everyday activities we found 28 severe cases (62.2%); 13 (28.9%) were moderate cases and 3 (6.7%) were mild cases. Based on the intellectual function, 34 (75.6%) patients were classified with severe and profound MR, 2 (4.4%) had mild MR and 4 (8.9%) were normal.
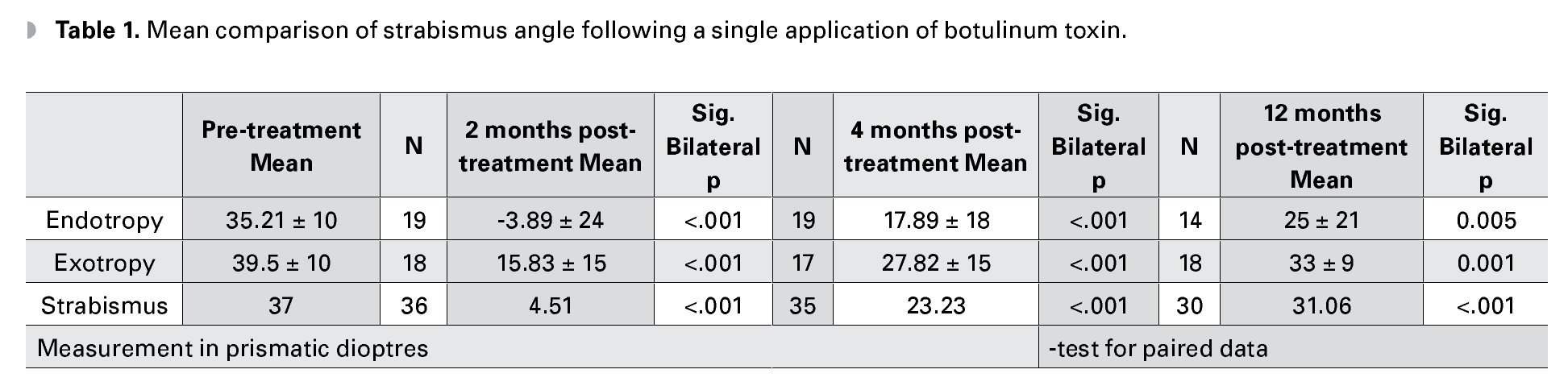
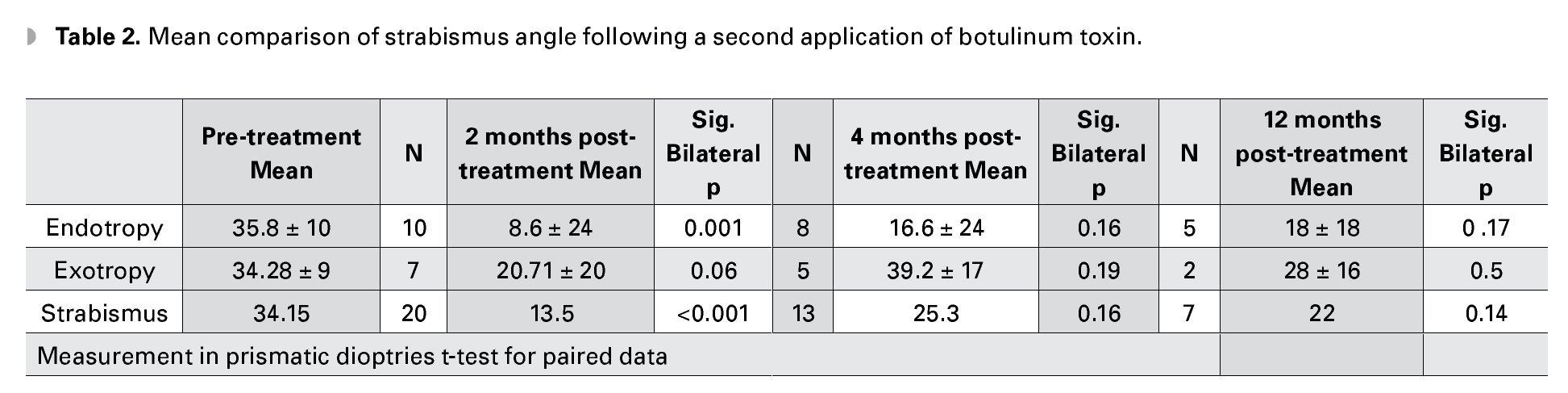
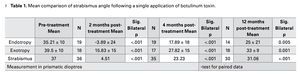
Assessment based on type of strabismus: 21 patients had endotropia with a deviation angle between 18 and 60 dp. Two months after treatment 17 (89.5%) of them had good results with hyper-corrections from 2 to 66 dp and a residual angle below 15 dp. After 4 months, 8 (42.1%) of them achieved. After 1 year, 5 (35.7%) of them was successful (Table 1).
A total of 24 patients had exotropy with a mean deviation angle between 20 and 60 dp. After 2 months, 8 (45%) were successful cases with hypercorrections of up to 10 dp. After 4 months, 3 (18%) cases were still successful. And after 1 year, only 1 case (Table 1).
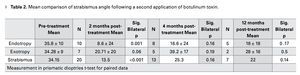
Of 17 treated cases with endotropy and exotropy and a mean correction angle of 35.8 dp, in endotropy and 34.2 dp in exotropy, the success rate for endotropy after 2 months was 5 (62.5%) cases with a mean angle of 8.6 dp and 2 (28%) successful exotropy cases. After 4 months, in the endotropy group we had 2 (33.3%) successful cases with a mean hypercorrection of 16.6 dp and in the exotropy group we have none. After 1 year of treatment, 5 (23%) endotropy cases remained with an hypercorrection of 10 dp; and 2 (4.1%) exotropy cases had residuals below 15 dp (Table 2).
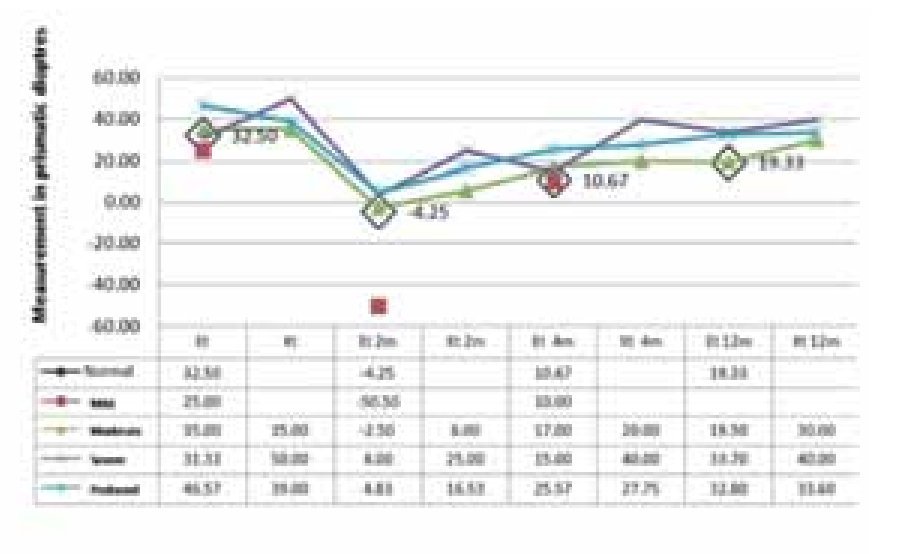
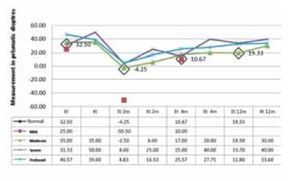
Results by MR: After 2 months, in the endotropy group the best responses were observed in 2 children with mild MR: 75 dp of correction. After 12 months, the mean correction was 15 dp in patients with mild and moderate MR. The worst results were observed in children with severe MR; in this group, 27 dp corrections were observed after 2 months, and after 12 months the mean correction was 9 dp. In the retreatment cases, we observed a significant less response and regression to the original strabismus, especially in children with severe MR.
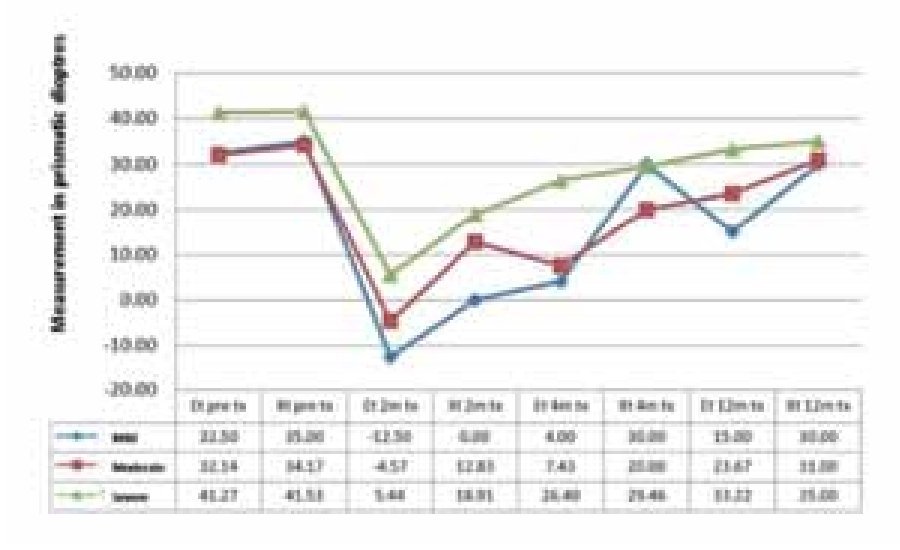
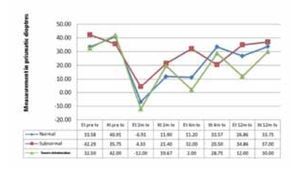
All the patients from the exotropy group had moderate, severe and profound MR. At the 2 and 4 month follow up, there was no difference in the response. But at the 12th month follow up they had a mean correction of 6.6 dp. The retreatment cases received a 2nd dose observing a minimum response; and at the 4th month after retreatment these cases returned to their original strabismus. Exotropy group: all the patients had moderate, severe and profound RM. At the 2nd and 4th month follow up there was no significant differences in the outcomes. The correction of 6.6 dp was achieved until 12 months. The retreatment cases received a 2nd dose with a minimum response, and after the 4th month all of them regress to the original strabismus (Figure 1).
¿ Figure 1. Mental retardation and strabismus.
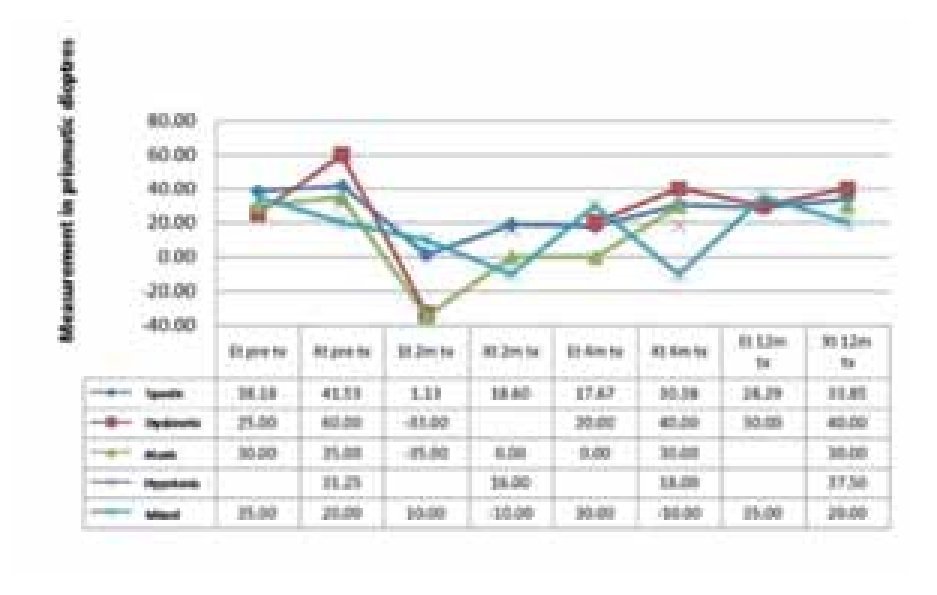
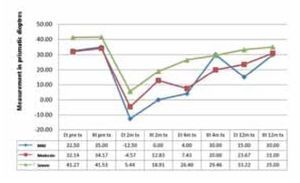
Response by degree of functional disability: in the endotropy group the best outcomes were observed in the mild cases and the worst corrections in the severe ones, with 18 vs. 8 dp. In the exotropy group the mean correction was 5 dp. The response tendency to retreatment was significantly less in the exotropy group (Figure 2).
¿ Figure 2. Strabismus and severity of the cerebral injury.
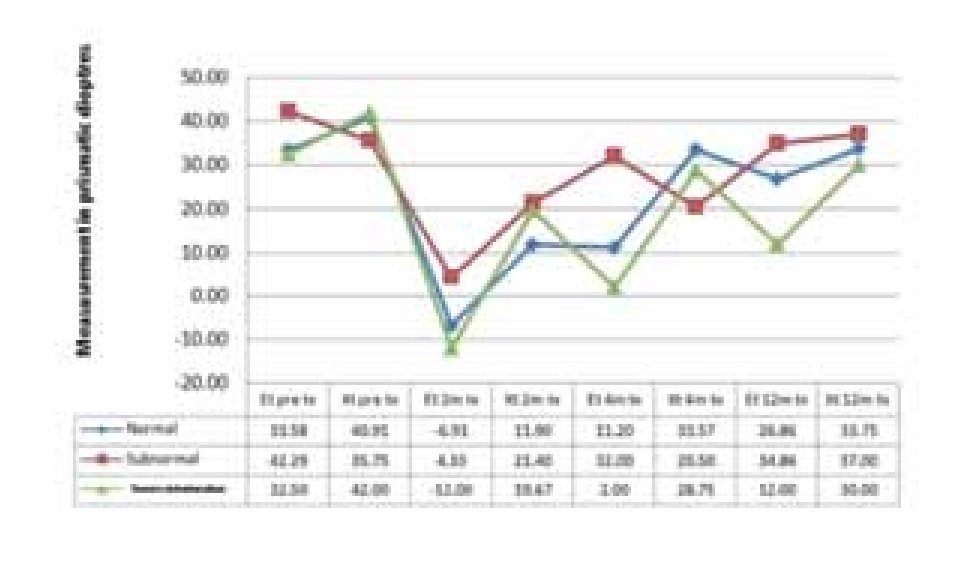
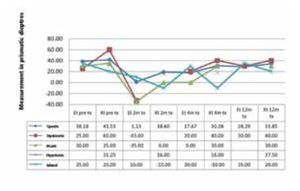
Response by type of injury: of the 34 patients with spastic PCP, 17 had endotropy and 17 had exotropy. Their outcome was: for the endotropy group the mean angle of correction was 38 dp after 2 months, 15 (88%) of them archived a correction of 37 dp making them successful cases. After 4 months they regressed to a residual mean of 18 dp and after 1 year to 28 dp. In the exotropy group the correction angle was 42 dp. After 2 months the correction was 19 dp and after 4 months and up to 1 year, all of them regressed to 34 dp. Arranged by frequency, the 4 patients with hypotonic PCP had exotropy with a correction angle of 31 dp; after 2 months the angle decreased to 16 dp, after 4 months 18 dp and after 1 year 37 dp (none of them were successful cases). Of the 3 children with dyskinetic PCP, 2 of them had endotropy and 1 exotropy. The endotropy group had an initial angle of 25 dp; after 2 months they achieved a hypercorrection of up to 33 dp, after 4 months they regressed to 20 dp and after 1 year they had a residual mean of 30 dp. The only exotropy patient with an initial angle of 60 dp underwent just one post-treatment follow up after 4 months with a residual of 40 dp. Of the 2 children with ataxic PCP, 1 had endotropy and 1 exotropy. In both cases the initial angle was 32 dp and after 2 months the endotropy had an hypercorrection of 35 dp and normal position after 4 months. Finally, of the 2 patients with mixed PCP, 1 had endotropy and 1 exotropy respectively; with the endotropy angle (35 dp) being higher than the exotropy (20 dp). After 2 months the endotropy was no corrected. After 4 months it was not corrected. After 6 months with 35 dp, it was reinjected. An after 1 year it archived -10dp. The exotropy had an initial hypercorrection of 10 dp, regressing to the initial angle after 4 months and to a residual of 20 dp after 1 year (Figure 3).
¿ Figure 3. Strabismus and type of cerebral palsy.
Results by visual acuity: 23 (51%) patients had normal vision (mean age 6 years old); 15 (33%) had subnormal vision (mean age 10 years old) and 7 (16%) had severe visual deterioration (the smallest children). In the patients with normal vision we had 4 successful cases after 1 year with corrections of up to 35 dp (all of them had endotropy). In the subnormal vision group we had 3 successful cases, and among the severe group we only had 2 successful cases. During retreatment, we had 2 successful cases among the normal vision group with corrections of up to 50 dp after 1 year of follow up. In the subnormal vision group we only had 1 endotropy case that achieved a correction of 45 dp after 1 year of treatment. None of the patients with severe deterioration were successful (Figure 4).
¿ Figure 4. Strabismus and visual acuity.
From the ethyology point of view, the most frequent cases15 were the children with history of perinatal asphyxia, where 62% of them had exotropia and 56% had subnormal vision with severe deterioration. The second cause was prematurity in 15 cases; where 66% of them had endotropy, 46% with subnormal vision and severe deterioration. The third place with 4 cases went to the infectious diseases; 75% with exotropy, 50% with subnormal vision and severe deterioration. The smallest frequency was represented by postnatal accidents as well as genetic and congenital disorders.
We also had 2 cases of consecutive exotropy in children with spastic PCP and severe MR after 1 year of retreatment. Some of the secondary effects seen are: transitory ptosis with spontaneous resolution during the 2 first weeks and subconjunctival hemorrhage.
¿ Discussion
Strabismus associated with PCP represents a problem for the motor and sensory diagnosis, particularly in those patients that also have systemic complications that endanger their lives and intellectual development. Therefore we must not delay the strabismus treatment and treat patients with advance deterioration of the motor and sensory eye functions. Previous studies show that the surgical treatment of these patients has uncertain results due to the neurologic instability secondary to the cerebral injury, the compromise of the cortical and subcortical control centers and the poor fusion potential; all of these lead to hypercorrections.2,4 Surgical treatment has been substituted by the BT in these patients, and its effectiveness and innocuousness has been demonstrated in neurological healthy patients and those with cerebral injury secondary to diagnosis different to cerebral palsy and in those with systemic diseases where there is a high risk during the anesthetic procedure.2,3
Strabismus is very frequent in patients with cerebral injury. According to several studies the frequency range is 30% to 80%. In our center, 60% of the patients with PCP have some type of strabismus. We agree with the results published by Arroyo Yllanes, who reports that quadriparesia is more frequent (75%), while in our center we have a 77%. The author reports the spastic type as the more frequent (67%). We agree with a higher percentage (75%).16,17 Another important fact in the published work of the above mentioned author is that there is no correlation between the type and the severity of the PCP with the type of strabismus. However, we can say that the exotropy does have a relationship with the hypotonic type and severe PCP. A clinical element that is particularly important is the variation of the deviation angle.4,16 In our work, we did not take it into account for the determination of the result. However, we did treat strabismus cases with angle variation and the biggest angle was taken into consideration. Several published studies mix up patients with different types of cerebral injury. We only included patients with diagnosis of PCP in an effort to homogenize our study group. As a comparison, we can mention the results according to the type of strabismus published by Moguel, where the endotropy group had a 69% rate of success4 and Arroyo Y had a 31% rate of success8 when compared with the 38.1% of our group in the long run. For the exotropy group Moguel reports a 40% rate of success4,5 compared with the 16.6% in our cases and pointing out as successful patients those within a residual of 15 dp. The difference in the success rate is very obvious, above all among the published results of neurological healthy children, as in the Gómez de Liaño study where the success rate was between 66% and 76% in the endotropy group with a residual of 10 dp.18,19 It is likely that our evaluation criteria for a good result was strict, because if we add the outcomes where the residual deviations were within 15 dp, the percentage goes up to 84.2% in the endotropy group and 42.1% in the exotropy group after 2 months. In our study series we found 2 (9.5%) cases of consecutive exotropy, that Arroyo Y. and collaborators also points out in 25% their cases8 and Tejedor and collaborators in 0.3% of their 2245 patients treated for endotropy;20 all them needed surgical correction after 1 year of treatment with BT. The possible contributing factors to this result could have been the high dose of toxin and the bad sensory status. In our patients, we observed this after the second application; therefore we can attribute it to an excessive dose. It is possible that the consecutive exotropy in children with psychomotor delay is the result of multiple factors, among them the bad development of the centers of binocular cortical integration, convergence insufficiency and reinjection. Even though the treatment success outcomes of strabismus in children with PCP are not encouraging, we agree with Keith W McNeer21,22 in that one of the most important factor in strabismus treatment is to maintain a good eye alignment as long as possible during the visual development period.
¿ Conclusion
In the short term, the BT is effective in PCP with endotropy, showing a high rate of success after 2 and 4 months of treatment. But in the long run it had a low rate of success if we only consider the size of the deviation angle. However, we can consider that the children with mild cerebral injury and a lower degree of MR with small to medium entropy angles have a better response even with a history of prematurity.
The BT is not effective in the long run for PCP with exotropy. However, we did see a decrease of the deviation angle after 2 months of treatment with a tendency to return to the original strabismus. These are associated with severe and profound MR and severe visual deterioration.
Even though it was not statistically significant, we can establish a relationship between the hypotonic PCP cases with great exotropy and the worst results.
We consider that the failures in the endotropy and exotropy groups are due to the poor fusion potential of the children with cerebral injury.
The children with better vision (in the endotropy and exotropy groups) have a better response to the first application and did not show differences in the following one. Therefore, the first application of BT decides the response to treatment.
Corresponding author: Copal 4575, frac. Arboledas del Sur, Guadalajara Jalisco México C.P. 44980.
Phone: 33 31342552, fax: 33 31342525.
E-mail address: isegura@teleton-occ.org.mx