The purpose of the current study was to assess changes in human corneal rigidity after treatment with riboflavin and UVA using a new device, the Corneal Displacement Unit (CDU).
DesignExperimental study. The CDU was designed to quantitatively measure the effect of cross-linking (CXL) in complete human donor cornea buttons. This apparatus measures the tissue displacement associated to computer-controlled variations in pressure.
MethodsBaseline measurements with the CDU were taken from 10 de-epithelialized human corneas. They were exposed to 0.1% riboflavin drops every 2min for 1h with exposure to UVA light during the last 30min after which CDU measurements were taken again. Results were analyzed using a non-parametric test. Significant tests were set at P≤.15 and non-significant correlation coefficients at rho≤.15 to reject abnormal measurements. For each of the 10 corneas, pachymetry values and 1988 CDU measurements were collected before and after treatment.
ResultsPressure measurements averaged across the corneas were similar before and after treatment (P≥.99), and were highly correlated (Spearman rho=.88, P<.001). Corneal displacement observations after treatment were significantly different from baseline, showing a reduction of .084 microns on average (P<.001), and thus demonstrating a reduced displacement in cross-linked corneas.
ConclusionsThe present study demonstrated a significant increase in the mechanical rigidity of human corneas after CXL. The CDU was able to quantify the mechanical strength of whole corneal buttons ex vivo with minimal damage to the tissue.
El objetivo de este estudio fue estudiar los cambios en la rigidez corneal tras el tratamiento con Riboflavina y luz ultravioleta (UVA) utilizando un nuevo aparato, la unidad de desplazamiento corneal (CDU).
DiseñoEstudio experimental. El CDU fue diseñando para medir cuantitativamente el efecto del cross-linking (CXL) en botones corneales humanos. El instrumento mide el desplazamiento asociado a variaciones en la presión controladas por computadora.
MétodosTomamos medidas basales con el CDU en 10 corneas tras remover el epitelio. Las corneas fueron expuestas a Riboflavina 0.1%, 1 gota cada 2 minutos durante 1 hora con exposición a UVA durante los últimos 30 minutos, al finalizar se tomaron mediciones con el CDU nuevamente. los resultados fueron analizados con prueba no paramétrica., La validez se estableció con P ≤ .15 y el coeficiente de correlación no significativo en rho ≤ .15 para descartar mediciones anormales. Para cada cornea, valores paquimétricos y 1988 mediciones del CDU fueron tomadas antes y después del CXL.
ResultadosLos valores promedio de presión entre las corneas fueron similares antes y después del tratamiento. (P≥0.99), con una alta congruencia (Spearman rho=0.88, P<0.001) a diferencia de las mediciones de desplazamiento, donde los valores después de CXL mostraron una reducción promedio de 0.084 micras (P<.001); demostrando así un desplazamiento reducido en las corneas tratadas.
ConclusionesEste estudio demuestra un aumento en la rigidez corneal tras tratamiento con CXL. El CDU logro cuantificar el endurecimiento de botones corneales ex vivo con daño mínimo al tejido.
Corneal cross-linking (CXL) is a novel approach to strengthen the cornea by increasing the mechanical and biochemical stability of stromal tissue. CXL consists in photopolymerization of stromal fibers by the combined actions of a photosensitizing agent (riboflavin) and Ultraviolet-A (UVA), which leads to an increase in the collagen fiber diameter and corneal stiffness.1,2
Biomechanical properties of the cornea have been widely studied as a way of addressing corneal changes after CXL, providing crucial information to understand the fundamentals of this treatment. Wollensak and coworkers3 analyzed corneal rigidity by stress-strain measurements of corneal strips on a microcomputer-controlled biomaterial tester. They found an increase in rigidity, indicated by rise in stress, of more than 300% in treated human corneas. Later, Kohlhaas et al.4 used corneal biomechanical properties to describe the localized effect of CXL in the anterior portion of strips of human and porcine corneas.
Until recently, the study of tissue mechanical properties has relied on methods such as tensile tests, which require the samples to be cut. To better ascertain the effects of the CXL process, it is necessary to utilize techniques that are capable of evaluating biomechanical properties within complete corneas. The aim of the present study was to assess changes in human corneal rigidity after treatment with riboflavin and UVA irradiation. For this purpose we designed a new device, the Corneal Displacement Unit (CDU), to quantitatively measure the effect of CXL in complete human donor cornea buttons. This apparatus measures the tissue displacement associated to computer-controlled variations in pressure. Results obtained from this study may further expand our understanding of CXL process and its potential role in our therapeutic armamentarium.
Materials and methodsThe CDU was designed with the help of the bioengineering department at our university; once the final model was built, several test runs with human corneal buttons demonstrated stability of the measurements; corneas without exposure to riboflavin or UVA light were maintained in the artificial chamber and measurements repeated twice during the next hour, these preliminary data taught us that as long as we kept a stable pachymetry throughout the experiment the displacement remained steady. Taking this into consideration we designed the present study to assess the effect of CXL in corneal displacement with the CDU.
Ten research grade corneas not suitable for corneal transplantation were obtained from the San Diego Eye Bank. The post-mortem time of the human eyes was less than 48h. Corneas that had prior surgery, scarring or pathology that could affect corneal clarity or hydration were not accepted for the study.
We removed the corneal epithelium from 10 corneas, took baseline measurements with the CDU, and then exposed the corneas to 0.1% isotonic riboflavin drops (10mg riboflavin-5-phosphate in 10ml dextran T-500 20%) every 2min for 1h with exposure to UVA light during the last 30min after which CDU measurements were taken again.
Pachymetry measurements were performed in all corneas immediately after removal of the epithelium, before UVA exposure and before the second CDU measurement to ensure a stable pachymetry between readings (±40μm).
UVA irradiationUVA exposure was performed with a Vega LED-based UV emitter (CSO Srl. Firenze, Italy) assembled and tested according to the manufacturers instructions. The Vega LED is preset to emit radiation of 370nm wavelength at an intensity of 3.0mW/cm2; a UV meter was used to check the UV emission power at the treatment plane before exposure. Exposure was carried out for 30min with a 10mm treatment diameter as per the manufacturer's protocol.
Corneal Displacement UnitThe CDU consists of a computer regulated piezo-electric pressure transducer that is connected to an artificial anterior chamber via semi-rigid surgical tubing filled with balanced salt solution (Fig. 1). Ex vivo human corneal tissue was then mounted onto the artificial anterior chamber and a watertight seal was obtained. This system allowed for precise computer control of the internal pressure within the artificial anterior chamber using LabView (National Instruments Corporation, Austin, TX).
Corneal Displacement Unit: a computer regulated piezo-electric pressure transducer is connected to an artificial anterior chamber via semi-rigid surgical tubing filled with balanced salt solution. This system allowed for precise computer control of the internal pressure within the artificial anterior chamber using LabView (National Instruments Corporation, Austin, TX).
A HeNe laser emitter and solid-state detector unit with fixed placement were both mounted above the apex of the corneal tissue. After internal calibration of the laser, the tissue was placed at an appropriate distance from the laser such that the reflected beam was within the detectors range to allow for measurements of the physical displacement of the corneal apex. These measurements were obtained using LabView and were correlated with the corresponding pressure applied by the pressure transducer within the artificial anterior chamber. We placed the corneas in pressure cycles that range from 0.1 to 1.0 PSI, which corresponds to an intra-ocular pressure of 5.6mmHg to 56mmHg, with a frequency of 6 cycles per minute for 10min.
We performed preliminary testing in 5 corneas which were placed in the CDU for a full hour without the CXL procedure; these corneas showed pressure and corneal displacement measurements that were stable throughout the timeline validating the accuracy and baseline measurements for our study. In this study we compared pretreatment and post-CXL CDU measurements in each cornea tested.
Statistical analysisFor each of the 10 corneas, pachymetry values and 1988 CDU measurements were collected before and after treatment. Stability of measurements before and after treatment was examined for each cornea using non-parametric tests, i.e., Wilcoxon matched pairs test, and Spearman correlation. Significant tests were set at P≤.15 and non-significant correlation coefficients at rho≤.15 to reject abnormal measurements. All measurements were then averaged across all corneas retained for analysis and analyzed using non-parametric tests to assess any change in displacement post-CXL treatment from preoperative CDU measurements.
ResultsWe were able to perform all the measurements in 9 out of 10 corneas; results from corneal button # 1 were discarded due to abnormal values caused by a leak from the artificial anterior chamber. This leak was likely caused by a small diameter scleral ring. Another 2 corneal button measurements were discarded after statistical analysis due to skewed observations between the data collected before and after CXL. The computer captured too many data points at the highest pressure values on the untreated corneal buttons and too many points at the lowest pressure values once the corneal buttons were CXL; these data had a correlation near to 0 and therefore could not be utilized in our study.
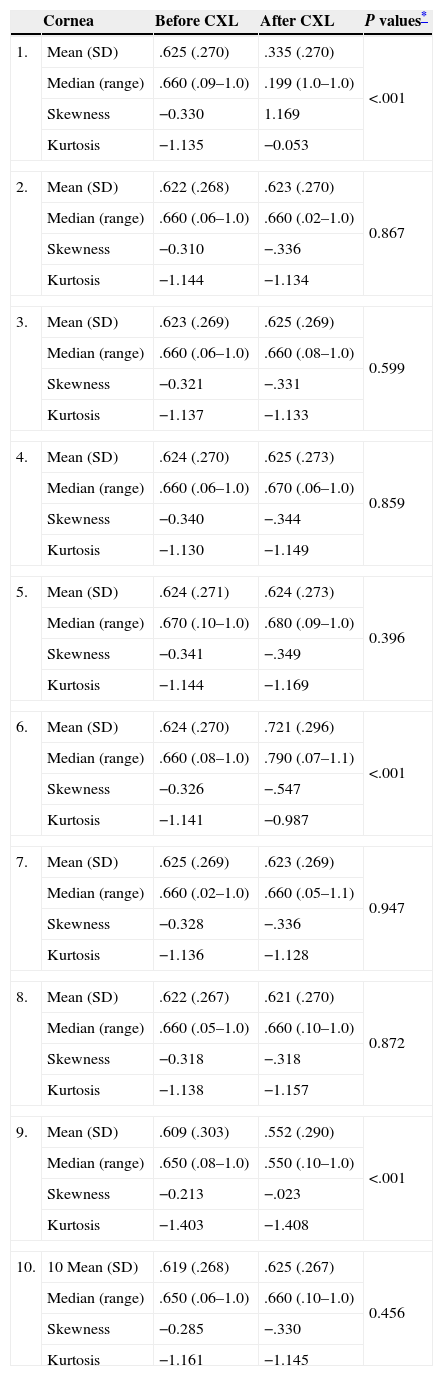
Tables 1 and 2, respectively, show IOP and corneal displacement measurements for 10 human corneas before and after CXL treatment. Pressure measurements averaged across the 7 remaining corneas were similar before and after treatment (P≥.99), and were highly correlated (Spearman rho=.88, P<.001). Corneal displacement observations after treatment were significantly different from baseline, showing a reduction of .084μm on average (P<.001), and thus demonstrating a reduced displacement in cross-linked corneas (Table 3, Fig. 2).
Mean (SD), median (range) measurements of IOP in PSI for 10 human corneas before and after CXL treatment.
| Cornea | Before CXL | After CXL | P values* | |
|---|---|---|---|---|
| 1. | Mean (SD) | .625 (.270) | .335 (.270) | <.001 |
| Median (range) | .660 (.09–1.0) | .199 (1.0–1.0) | ||
| Skewness | −0.330 | 1.169 | ||
| Kurtosis | −1.135 | −0.053 | ||
| 2. | Mean (SD) | .622 (.268) | .623 (.270) | 0.867 |
| Median (range) | .660 (.06–1.0) | .660 (.02–1.0) | ||
| Skewness | −0.310 | −.336 | ||
| Kurtosis | −1.144 | −1.134 | ||
| 3. | Mean (SD) | .623 (.269) | .625 (.269) | 0.599 |
| Median (range) | .660 (.06–1.0) | .660 (.08–1.0) | ||
| Skewness | −0.321 | −.331 | ||
| Kurtosis | −1.137 | −1.133 | ||
| 4. | Mean (SD) | .624 (.270) | .625 (.273) | 0.859 |
| Median (range) | .660 (.06–1.0) | .670 (.06–1.0) | ||
| Skewness | −0.340 | −.344 | ||
| Kurtosis | −1.130 | −1.149 | ||
| 5. | Mean (SD) | .624 (.271) | .624 (.273) | 0.396 |
| Median (range) | .670 (.10–1.0) | .680 (.09–1.0) | ||
| Skewness | −0.341 | −.349 | ||
| Kurtosis | −1.144 | −1.169 | ||
| 6. | Mean (SD) | .624 (.270) | .721 (.296) | <.001 |
| Median (range) | .660 (.08–1.0) | .790 (.07–1.1) | ||
| Skewness | −0.326 | −.547 | ||
| Kurtosis | −1.141 | −0.987 | ||
| 7. | Mean (SD) | .625 (.269) | .623 (.269) | 0.947 |
| Median (range) | .660 (.02–1.0) | .660 (.05–1.1) | ||
| Skewness | −0.328 | −.336 | ||
| Kurtosis | −1.136 | −1.128 | ||
| 8. | Mean (SD) | .622 (.267) | .621 (.270) | 0.872 |
| Median (range) | .660 (.05–1.0) | .660 (.10–1.0) | ||
| Skewness | −0.318 | −.318 | ||
| Kurtosis | −1.138 | −1.157 | ||
| 9. | Mean (SD) | .609 (.303) | .552 (.290) | <.001 |
| Median (range) | .650 (.08–1.0) | .550 (.10–1.0) | ||
| Skewness | −0.213 | −.023 | ||
| Kurtosis | −1.403 | −1.408 | ||
| 10. | 10 Mean (SD) | .619 (.268) | .625 (.267) | 0.456 |
| Median (range) | .650 (.06–1.0) | .660 (.10–1.0) | ||
| Skewness | −0.285 | −.330 | ||
| Kurtosis | −1.161 | −1.145 | ||
Mean (SD), median (range) for corneal displacement measurements in microns for 10 human corneas before and after CXL treatment.
| Cornea | Before CXL | After CXL | Mean difference | P values* | |
|---|---|---|---|---|---|
| 1.E | Mean (SD) | .111 (.003) | .093 (.002) | −.018 (.003) | <.001 |
| Median (range) | .112 (.082–0.114) | .199 (.076–.095) | |||
| 2. | Mean (SD) | .099 (.002) | .107 (.003) | .008 (.003) | <.001 |
| Median (range) | .098 (.098–.110) | .106 (.105–.118) | |||
| 3. | Mean (SD) | .078 (.003) | .073 (.001) | −.005 (.003) | <.001 |
| Median (range) | .079 (.068–.082) | .073 (.064–.075) | |||
| 4. | Mean (SD) | .117 (.001) | .092 (.012) | −.025 (.012) | <.001 |
| Median (range) | .118 (.115–.123) | .073 (.071–.125) | |||
| 5. | Mean (SD) | .116 (.002) | .092 (.001) | −.026 (.002) | <.001 |
| Median (range) | .116 (.102–.119) | .091 (.088–.095) | |||
| 6.E | Mean (SD) | .107 (.002) | .104 (.001) | −.003 (.002) | <.001 |
| Median (range) | .107 (.095–.120) | .103 (.101–.106) | |||
| 7. | Mean (SD) | .108 (.003) | .053 (.001) | −.055 (.003) | <.001 |
| Median (range) | .107 (.105–.123) | .053 (.051–.055) | |||
| 8. | Mean (SD) | .067 (.002) | .082 (.001) | .015 (.001) | <.001 |
| Median (range) | .067 (.061–.071) | .082 (.082–.086) | |||
| 9.E | Mean (SD) | .109 (.002) | .109 (.001) | −.001 (.002) | .250 |
| Median (range) | .109 (.107–.122) | .109 (.108–.110) | |||
| 10. | Mean (SD) | .121 (.001) | .122 (.001) | .001 (.001) | <.001 |
| Median (range) | .121 (.117–.124) | .122 (.120–125) |
IOP and corneal displacement measurements averaged across the 7 remaining corneas before and after CXL treatment.
| Cornea | Before CXL | After CXL | Mean difference | P values* |
|---|---|---|---|---|
| IOP | ||||
| Mean (SD) | 4.36 (1.60) | 4.37 (1.32) | .01 (.80) | .99 |
| Median (range) | 4.54 (.59–6.72) | 4.49 (.68–4.92) | .05 (.09–1.80) | |
| Displacement | ||||
| Mean (SD) | .706 (.007) | .622 (.014) | −.084 (.014) | <.001 |
| Median (range) | .704 (.684–.732) | .615 (.597–.664) | −.09 (.87–.68) | |
In the current study, we demonstrated an increase in mechanical stability by the reduction on corneal displacement of ex vivo human corneas after treatment with riboflavin and UVA. The CDU provides reproducible displacement values of the cornea with minimal damage to the tissue. This new technique may potentially validate and compare new treatment strategies by evaluating changes in corneal stiffness caused by CXL.
CXL has emerged as a promising alternative to intra-stromal implants, penetrating or lamellar keratoplasty in the treatment of keratoconus and post-refractive ectasia.5–7 Therefore, new technologies to assess the effects of CXL are needed. The majority of experimental studies3,4,8 used tensile measurements in order to assess stress–strain properties after CXL. Although these techniques provide important biomechanical data, they require the cornea to be sectioned, which alters the properties of the corneal button functioning as an entire unit. Some of these experimental problems include the following: the collagen fibers at the edge of these sliced samples are fragmented, thus reducing the predictability of the measurements; the segmentation of the corneal buttons leaves them susceptible to changes in hydration that can further modify the biomechanical properties of the tissue. Furthermore, because these samples must be clamped in the jaws of the device, the edges are submitted to compressive tension that may alter the final results. In contrast, the CDU, used in the present study, allows us to analyze the response of the whole cornea as a unit. There is no need for segmenting the tissue since the whole button is mounted on the artificial chamber where it stays in place during the whole experiment. This also allows us to maintain constant pressure behind the cornea during the time between measurements. Characteristics of this CDU may optimize biomechanical measurements and serve as a model for further applications.
Corneal biomechanical analysis has enhanced our understanding of the CXL process. In 2003, Wollensak3 first described the results of mechanical measurements of human corneal strips after CXL. An increase in rigidity of 328.9% was observed after treatment, with a corresponding increase of 4.5 in Young's modulus. The same biomaterial measuring device was used by Kohlhaaset et al.4 to evaluate stress strain characteristics of the anterior and posterior portions of the cornea. Their results provided further evidence that the effect of CXL is greater in the anterior stroma.9–13 Recently, this type of measurements was also used to evaluate the CXL effect after modifications of the standard CXL technique. Rigidity analysis was used to compare CXL effects on corneas with and without de-epithelialization14 and it was demonstrated that corneas with intact epithelium had a decreased stiffening effect. Similar studies were performed by McCall et al.,8 but in all of these studies, and in contradistinction with the CDU described in the present manuscript, cutting the corneas into segments was necessary to allow for the measurement of biomechanical data.
The need for a non-destructive technique to assess corneal stiffness and biomechanical properties is soaring; therefore other investigators, including Duppset et al.15 and Mattson et al.16 have explored other potential techniques that may allow the analysis of corneal rigidity in whole corneal buttons. A technique named Globe Expansion Method (GEM)16 was tested in rabbit eyes with the purpose of measuring the behavior of cross-linked tissue to elevated intra-ocular pressure; in this study, corneas submitted to riboflavin and UVA had a reduced expansion compared with control corneas. Another non-invasive technique named Surface Wave Elastometry15,17 attempts to assess biomechanical properties by measuring the velocity of the wave propagation along the long axes of the collagen fibrils. The authors tested, in vitro, the changes in corneal elasticity after CXL and found that surface wave velocity increased after treatment, thus assuming that the cornea was strengthened by increased stiffness. Although using different techniques from the one described in our paper, the results obtained by these non-destructive techniques seem to concur with our findings.
In conclusion, we demonstrated a significant increase in the mechanical rigidity of human corneas after CXL, providing further evidence of the effect of riboflavin/UVA on corneal tissue. We have developed novel equipment, which we named the Corneal Displacement Unit, to quantify the mechanical strength of whole corneal buttons ex vivo with minimal damage to the tissue. This new device could be helpful in comparing different CXL protocols, new riboflavin formulations and delivery methods of cross-linking components. We believe this and other related devices could further expand our knowledge within this developing field of cross-linking.
Ethical responsibilitiesProtection of people and animalsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
FundingNo endorsement of any kind received to conduct this study/article.
Conflict of interestThe authors declare no conflict of interest.