Different type of anesthesia has been implicated in the exacerbation of multiple sclerosis. Moreover, dental anesthesia is related to ophthalmologic complications such as diplopia due to oculomotor nerves palsy. Various pathophysiologic mechanisms are discussed: intravascular (arterial/vein) injection of anesthetic, reflex vasospasm and diffusion of local anesthetic.
Case reportA 36-year-old woman who presented an horizontal left gaze palsy, bilateral nystagmus in extreme gaze and left peripheral facial palsy after dental anesthesia. The patient recovered peripheral facial palsy within 3h after the injection. As a result of the magnetic resonance, it was initiated high doses systemic corticosteroid treatment and the gaze palsy resolved within three weeks. The patient was diagnosed with peripheral facial palsy secondary to dental anesthesia and multiple sclerosis.
ConclusionThe concomitance of symptoms with local anesthesia complicates the etiological diagnosis of pathology, so exhaustive and detailed exam taking into consideration all factors is necessary for a proper diagnosis and treatment.
Diferentes tipo de anestesia han sido relacionados con la exacerbación de la esclerosis múltiple. Así mismo, la anestesia dental está relacionada con complicaciones oftalmológicas tales como diplopía debido a parálisis de los nervios oculomotores. Se discuten diversos mecanismos fisiopatológicos: una inyección intravascular (arterial/venosa) de anestésico, un vasoespasmo reflejo o una difusión del anestésico local.
Caso clínicoMujer de 36 años de edad que presenta un nistagmus bilateral en la mirada extrema, parálisis en la mirada horizontal izquierda y parálisis facial periférica izquierda después de una anestesia dental. La paciente se recuperó de la parálisis facial periférica transcurridas 3 horas de la inyección anestésica. Debido al resultado de la resonancia magnética, se inicia tratamiento con dosis altas de corticosteroides sistémicos resolviéndose la parálisis de la mirada en tres semanas. La paciente fue diagnosticado de parálisis facial periférica secundaria a anestesia dental y esclerosis múltiple.
ConclusiónLa concomitancia de los síntomas con la anestesia local complica el diagnóstico etiológico de la patología, por lo que un examen exhaustivo y detallado teniendo en cuenta todos los factores es necesario para un diagnóstico y tratamiento adecuados.
For many years, dental literature describes signs and symptoms at the ophthalmic level following injection of anesthesia into the superior level oral cavity. Typical ophthalmology complications after intraoral anesthesia include: temporary diplopia, transitory unilateral amaurosis, strabismus due to paralysis of the extrinsic muscles of the eyes and palpebral ptosis. Paralyzes of the lateral rectus muscle or anesthesia of the abducens nerve have been reported. The ocular alterations are quite uncommon, representing approximately 0.1% of the complications.1 Generally, the ophthalmologic complications have an immediate to short onset.2
Various pathophysiologic mechanisms of ophthalmologic complications after local anesthesia are discussed in the literature1,2: Intra-arterial injection by medial meningeal artery or aberrant arterial patterns, autonomic dysregulation (vasospastic impulse), deep injection and diffusion across the pterygo-palatine fossa to the inferior orbital fissure or intravenous injection (cavernous sinus). The abducens nerve is the most vulnerable in the region of the orbital apex, the anesthetic could have diffused across the pterygp-palatine fossa and researched the abducens nerve by direct contact of the solution with the nerve.3,4
Spinal, general, epidural anesthesia and mandibular block have been implicated in the exacerbation of multiple sclerosis; these may precipitate multiple sclerosis onset or attack.5
Ocular motor syndromes are extremely common in multiple sclerosis. The high predilection for these abnormalities may relate to the close proximity of the ocular motor apparatus to the brainstem periventricular zone, including the forth ventricle. Other pathology secondary to damage in that area is a horizontal gaze palsy result from lesions of paramedian pontine reticular formation (PPRF), the abducens nucleus or/and medial longitudinal fasciculus (MLF).6 Limitations of eye movements in multiple sclerosis is commonly associated with saccadic instability, manifested clinically as involuntary movements such as nystagmus.6,7
Case reportA 36 year-old healthy woman was referred to the Department of Ophthalmology for diplopia and “bouncing images”. Previously, the patient was submitted to maxillary left third molar removal with intraoral local anesthesia. The examination revealed left peripheral facial palsy and eye movement disorders; horizontal left gaze palsy: minimal left eye abduction associated with right eye mild delay on adduction (Fig. 1), bilateral nystagmus occurs only when the eyes are moved into eccentric gaze, especially in lateral and up gaze, with quick phases opposite to the direction of the prior eccentric gaze. Convergence and vertical gaze movements were preserved. The visual acuity was 20/20 bilaterally with full visual fields, Isihara plate color testing and funduscopic exam were normal. There was no dilatation of the pupil and all the vital signs were checked to be normal. The patient recovered peripheral facial palsy within 3h after the injection.
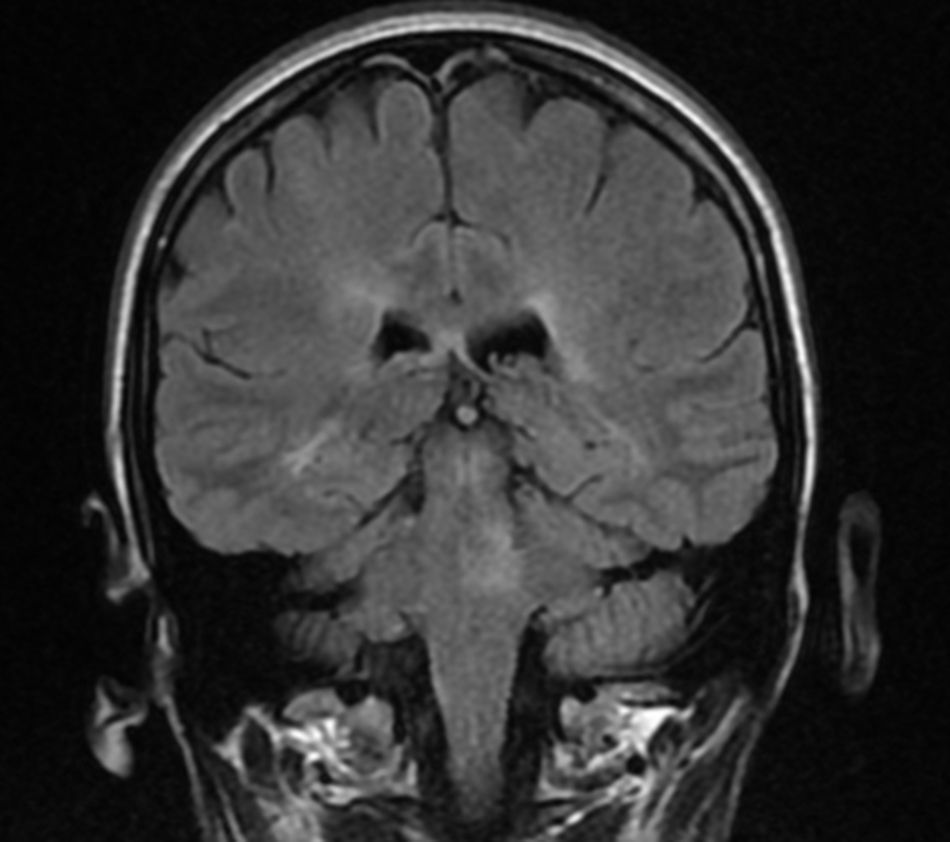
A magnetic resonance imaging was performed showing demyelinated plaques on the pons and hyperintense lesions located in the periventricular white matter and several subcortical e infratentorial injuries (Fig. 2).
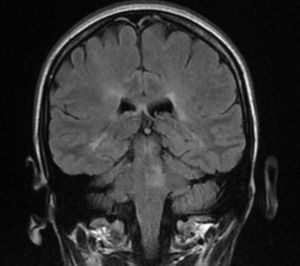
The patient was diagnosed with peripheral facial palsy secondary to dental anesthesia and multiple sclerosis. After initiating high dose systemic corticosteroid treatment by the Department of Neurology, the gaze palsy resolved within three weeks (Fig. 3).
DiscussionThis report describes an unusual multiple sclerosis case in a young woman, characterized by left peripheral facial palsy, unilateral gaze palsy and nystagmus, apparently associated with local anesthesia. The concomitance of all the symptoms complicates the diagnosis because as we have explained previously, the local anesthesia may produce a sixth and seven nerve palsies. While the presence of pathologic nystagmus and horizontal gaze palsy lead us to consider a demyelination disease, the simultaneity of symptoms with dental surgery could confuse our diagnosis. The patient had not been previously diagnosed with multiple sclerosis so, it could be that the dental intervention and/or anesthesia local may precipitate multiple sclerosis onset or attack. Following treatment with corticosteroids, the ocular motor syndrome completely resolved.
The magnetic resonance subsequently confirmed the diagnosis and corroborated the clinical localization. The lesion in this patient involves the abducens nucleus on the right and may be components of the medial longitudinal fasciculus.
Generically, the most frequent symptoms of onset are sensory problems (45%), followed by motor weakness. Visual disturbances are more common in the course of the disease but a symptom of onset represent only 20%.8 Optic neuritis is one of the most usual manifestations of multiple sclerosis, occurring in 14 to 23% of cases and approximately 2–4% of patients with multiple sclerosis develop pendular nystagmus.8
Isolated gaze palsies do occasionally occur in multiple sclerosis, but are more commonly associated with other such as an internuclear ophthalomoplegia.6
The VI nucleus is anatomically very closely related to the VII cranial nerve fibers, therefore, lesions in the VI nucleus are usually accompanied by ipsilateral facial paresis. The fact that the present cases reports an abduction limitation and facial paresis could be provoked an incorrect diagnosis whether you do not recognized that the palsy is peripheral secondary to dental anesthesia (spontaneous resolution within 3h of local anesthetic injection).
In conclusion, a good clinical examination and a proper assessment of all the symptoms are necessary to guide the appropriate tests in order to get a correct diagnosis. This case indicates that dentist, neuro-ophthalmologist and neurologist may be alerted to oculomotor palsy as a possible adverse effect of maxillary block anesthesia or secondary to neurological disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNon-financial support was received.
Conflict of interestNo conflicting relationship exists for any author.