Keratoconus is an idiopathic and progressive disease, where the cornea develops an irregular and conical shape, being the most common form of dystrophy or corneal ectasia, developing between the age of 12 and 20. In Mexico, the epidemiological information about the pathology is scarce.
PurposeTo explore the epidemiology of keratoconus in Mexico among adolescents, and to compare the prevalence with international literature reports. This study identified associated pathologies and examined the management of patients.
MethodsA retrospective study was conducted in an ophthalmology clinic; 500 charts were randomly selected from patients between 10 and 20 years of age in order to acquire information about the identification of the patient; the patient's gender, birthday, and age; three principal diagnoses at the first visit; as well as refraction and visual acuity in both eyes. After this, statistical analysis of the information was done.
ResultsThe prevalence rate of keratoconus was 1.8%, affecting 66% of females and 33.3% of males. The mean age of presentation was 16.1 years. The most frequently associated refractive error was compound myopic astigmatism (44.4%); 88.8% presented with bilateralism. The majority of patients were being managed conservatively.
ConclusionThrough this study, we found that our statistics matched those of internationally published reports concerning the early age of onset of the disease and its corresponding bilateralism. However, contrary to the international reports, it was evident that this condition was more prevalent among the females in our study sample, and no other associated pathologies were found.
El queratocono es una enfermedad idiopática y progresiva, donde la cornea adquiere una forma irregular y cónica, siendo la forma más común de distrofia o ectasia corneal desarrollándose entre los 12 y 20 años de edad. En México no se cuenta con suficiente información epidemiológica en cuanto a la patología.
ObjetivoExplorar la epidemiología del queratocono en México en adolescentes y comparar la prevalencia con reportes internacionales. Este estudio identifico patologías asociadas y evaluó el manejo de estos pacientes.
MétodosEstudio retrospectivo en una clínica oftalmológica; 500 expedientes fueron aleatoriamente seleccionados de pacientes entre 10 y 20 años de edad, obteniendo: identificación del paciente, sexo, fecha de nacimiento y edad, tres diagnósticos principales en su primer visita, refracción y agudeza visual en ambos ojos. Posterior a la captura de datos, se realizo el análisis estadístico.
ResultadosLa tasa de prevalencia de queratocono fue de 1.8%, afectando al 66% de las mujeres y el 33% de hombres. La edad media de presentación fue de 16.1 años de edad. El error refractivo asociado a queratocono más común fue astigmatismo miópico compuesto (44.4%); 88.8% se presentó con bilateralidad. La mayoría de los pacientes se trato de manera conservadora.
ConclusiónA través de este estudio, encontramos que nuestros resultados concuerdan con lo publicado internacionalmente en referencia al inicio temprano del queratocono y la bilateralidad. Pero, contrario a lo reportado, fue evidente que esta condición es más prevalente entre las mujeres de nuestra muestra, además no se encontraron patologías asociadas a queratocono.
Keratoconus is a progressive and idiopathic disease in which the cornea develops into an irregular and conic shape. The clinical signs include thinning of the cornea in its central or paracentral region, an apical protrusion, or an elevation of the central zone with an irregular astigmatism, and this condition can progress to the point of corneal perforation in extreme cases1; all of these issues can make it difficult to achieve adequate visual correction with the simple use of glasses.2 Keratoconus is a rare disease, as classified by the Office of Rare Diseases of the National Institute of Health. Despite this, keratoconus is the most common form of dystrophy or corneal ectasia, with an incidence of 50–230 per 100,000 persons.3
Some initial studies revealed a greater prevalence of keratoconus among women than men. Today, studies have not been able to find a significant difference between genders, and some studies have even found higher prevalence rate among males.4,5
Some reports have documented the age of onset as being as early as birth and up to 51 years of age. However, the vast majority of patients develop the disease between 12 and 20 years of age (it is diagnosed in adolescence and reaches its most severe form between the second and fourth decades of life).4,5 Based on these reports, we find the need to study this age population in order to define future strategies for diagnosis and treatment.
Keratoconus is a disease that is almost exclusively bilateral, yet asymmetric, as it begins in one eye and after 2–6 years it affects the contralateral eye. It is rare to find a purely unilateral disease. Hall reported that from a total of 288 patients, eight cases were unilateral, while Tuft reported that 4.3% of his sample exhibited unilateral keratoconus.6,7
In Mexico, the research on keratoconus is scarce; the articles published show statistics that are similar to those in international literature, which indicates a higher prevalence in male patients with a mean age of 24.5 years.8 This study will examine a specific population – adolescents. There is debate concerning the prevalence of keratoconus in the general population, but our focus is on the prevalence of keratoconus in the adolescent population visiting an ophthalmology concentration clinic.
ObjectiveTo explore the epidemiology of keratoconus in Mexico among an adolescent population, and to compare the prevalence rates of this condition with international literature reports.
MethodsThis study is a retrospective clinical study, which will examine the prevalence rates of keratoconus, for which 500 records were randomly selected. The calculated sample was 221 patients, using Raosoft®, with a 5% margin of error, a 90% confidence interval, and a population of 1200 patients. The patient records used were from patients between the ages of 10–20 years. A database was developed using Microsoft® Excel in which patients’ identification, gender, age, three main diagnoses at fist clinic visit, as well as refraction and visual acuity for both eyes were documented. After this, descriptive statistical analysis was performed for prevalence and means. All of the refractions that were documented were performed via skiascopy under cycloplegia. Since this was a general study about the prevalence of keratoconus in a specific population, no exclusion criteria were developed for this study. Before initiating, we received approval from the ethics committee, and the study adheres to the tenets of the Declaration of Helsinki.
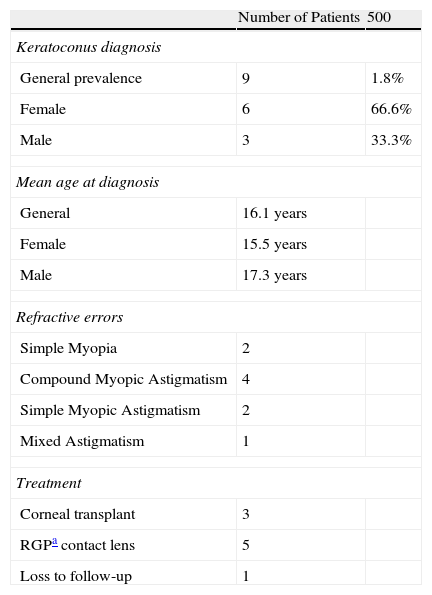
ResultsOf the 500 records that were examined, keratoconus was diagnosed in 9 patients, with a prevalence rate of 1.8% (Table 1). The proportion of keratoconus per gender was 6 (66.6%) females and 3 (33.3%) males. The mean age at diagnosis was 16.1 years, with 17.3 years of age for males and 15.5 years of age for females.
Data concentrate for diagnosis of keratoconus.
| Number of Patients | 500 | |
| Keratoconus diagnosis | ||
| General prevalence | 9 | 1.8% |
| Female | 6 | 66.6% |
| Male | 3 | 33.3% |
| Mean age at diagnosis | ||
| General | 16.1 years | |
| Female | 15.5 years | |
| Male | 17.3 years | |
| Refractive errors | ||
| Simple Myopia | 2 | |
| Compound Myopic Astigmatism | 4 | |
| Simple Myopic Astigmatism | 2 | |
| Mixed Astigmatism | 1 | |
| Treatment | ||
| Corneal transplant | 3 | |
| RGPa contact lens | 5 | |
| Loss to follow-up | 1 | |
The refractive errors detected were 2 patients with simple myopia, 2 with simple myopic astigmatism, 4 with compound myopic astigmatism, and 1 with mixed astigmatism. Of the detected patients, 3 (33.3%) had a penetrating keratoplasty and 5 (55.5%) were managed conservatively with rigid gas permeable contact lenses, with periodic adjustments. There was loss to follow-up of 1 (11.1%) patient, after the second visit and no management was appropriately delivered.
DiscussionOur study on keratoconus cannot be compared to an equally designed study from Mexico because no other studies use a similar population. Our 1.8% prevalence rate compares to that of Jonas et al. in India, where they obtained a 2.7% prevalence rate, sample of 4711 subjects, and in a study conducted in Jerusalem by Millodot et al., who reported a prevalence rate of 2.34% in a sample of 981 volunteers.9,10 Even though these studies exhibit slightly higher prevalence rates, our results can be regarded as being somewhat similar to those reported in these studies, especially if we compare our prevalence rates to those found by Ihalainen (0.03%).11
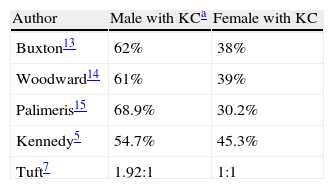
In relation to gender, we found prevalence rates of 66.6% and 33.3% for women and men, respectively. When we compare these results to those of the study conducted in Cuba by Diaz et al. – who reported similar prevalence rates per gender at 66% for females and 34% for males, had a sample of 73 patients – it is evident that these results are in contrast to those observed in several studies from the United States (Table 2).5,7,12–15
The mean age at diagnosis noted in our study was 16.1 years, which can be compared to the mean age at diagnosis found by Olivares and Guerrero, which was 15.39±3.95 years, which had a sample of 74 patients. Even though the mean age reported in our study indicated a younger age, we obtained results that were similar to those found in the general population.2 When comparing our study's results with those reported by Ruiz-Morales et al., they obtained an age at diagnosis of 24.5 years, study with a sample of 166 patients. While this indicates an older age at diagnosis, it should be considered that the study was conducted on post-transplant patients.8
Bilaterality is an important aspect to consider when analyzing a patient with suspected keratoconus. Our study demonstrated bilaterality in 8 (88.8%) patients, although it was asymmetric. Kennedy et al. found an incidence of bilateral involvement to be in 38 (59%) patients at the time of diagnosis.5 Our results obtained, could indicate a late approach to these patients in our clinic
Theories surrounding the diseases associated with keratoconus can be found in the literature. Some of these theories are based on the effects of hormonal stimulation as the genesis of this pathology. Also, keratoconus is associated with Trisomy 21 and allergic processes, but in our study, no relationships with other diseases were detected.2
The relevance of the management of these patients is important to note, as 33.3% of patients ended their treatment in penetrating keratoplasty in our study, clearly indicating that patients are being subjected to radical treatments. The reason behind this is based on the fact that patients at our clinic have already been to other clinics, and they are referred to us (a concentration clinic). Other factors include the fact that this is a population of low socioeconomic status and poor education level; these factors are often seen in the records in which patients’ visual acuity has been significantly affected, and where keratoconus is present and cannot be treated by noninvasive methods.
As the first study using the inclusion criteria specified above, we should highlight the need to perform additional studies. Our study was conducted with a calculated sample of 221 patients. The results are supported by our data, but in order to better compare and extrapolate our epidemiological data, a study that involves a higher number of subjects needs to be performed. In addition to having a larger sample size, other variables should be included such as family history, data concerning atopy, and factors concerning environmental exposure.
The importance of performing similar protocols in populations of this age group is necessary to establish statistics that can help identify the incidence and prevalence of keratoconus in populations of similar geographic areas (this study was conducted in the north of Mexico). Importantly, we can use these studies to establish etiologies, assess proper characteristics, and develop guidelines for the treatment of keratoconus.
ConclusionKeratoconus identification, diagnosis and treatment are of high importance for primary care physicians, optometrist and ophthalmologist when screening patients in this age group. The incorporation of epidemiology and public health organizations into a future project to identify probable causes can help us understand risk factors for our population, and the best method for detection and timely management.
FundingThe authors received no sponsorship to carry out this article.
Conflict of interestThe authors declare no conflict of interest.