¿ Introduction
Dry eye syndrome is a common ophthalmological problem, with a prevalence that can arise even to 73% of the patients, which has a great economic impact and generates a lot of symptoms in the patients.1-4 it can produce mild symptoms,5 but also lead to full incapacity.6,7
There are two clinical ways to determine the tear film's quantity and quality,8,9 one is the Schirmer test10,11 and the other one is the break up time test,12,13 both susceptible to do at the doctor's office with mild invasion to the patient .14
There isn't a generalized consensus nor either a standardization of these parameters11 about the Schirmer test and the break up time15 in Mexico, so some authors' don't give great importance to them,16-18 while some others base their studies on these criteria.19,20
Schirmer test consists on putting a filter paper strip inside the inferior cul-de-sac, between the external half of the inferior palpebral and bulbar conjunctiva, with part of this strip hanging from the eyelid. The expected is the wetting of the strip no more of 15 mm in the first two minutes.21 The tear film break up time is the time that takes from the first blink to the presence of the first desecation zone.13
The technique consists on putting the patient at the biomicroscope, without air drafts, with the slit lamp, and observing at approximately 10 magnifications so we can see simultaneously the whole cornea. The patient blinks and we determine how long it takes to appear the first desecation zone.22,23 The test should be repeated at least three times24 without intermediate interruptions and the three results should be written. Usually, in the same test, the three values appear at similar times, and frequently in the same spot.
Normal values are considered over 15 seconds. Mildly low values go from 11 to 15 seconds, moderately low values from 6 to 10 seconds and very low from 0 to 5 seconds.
¿ Methods
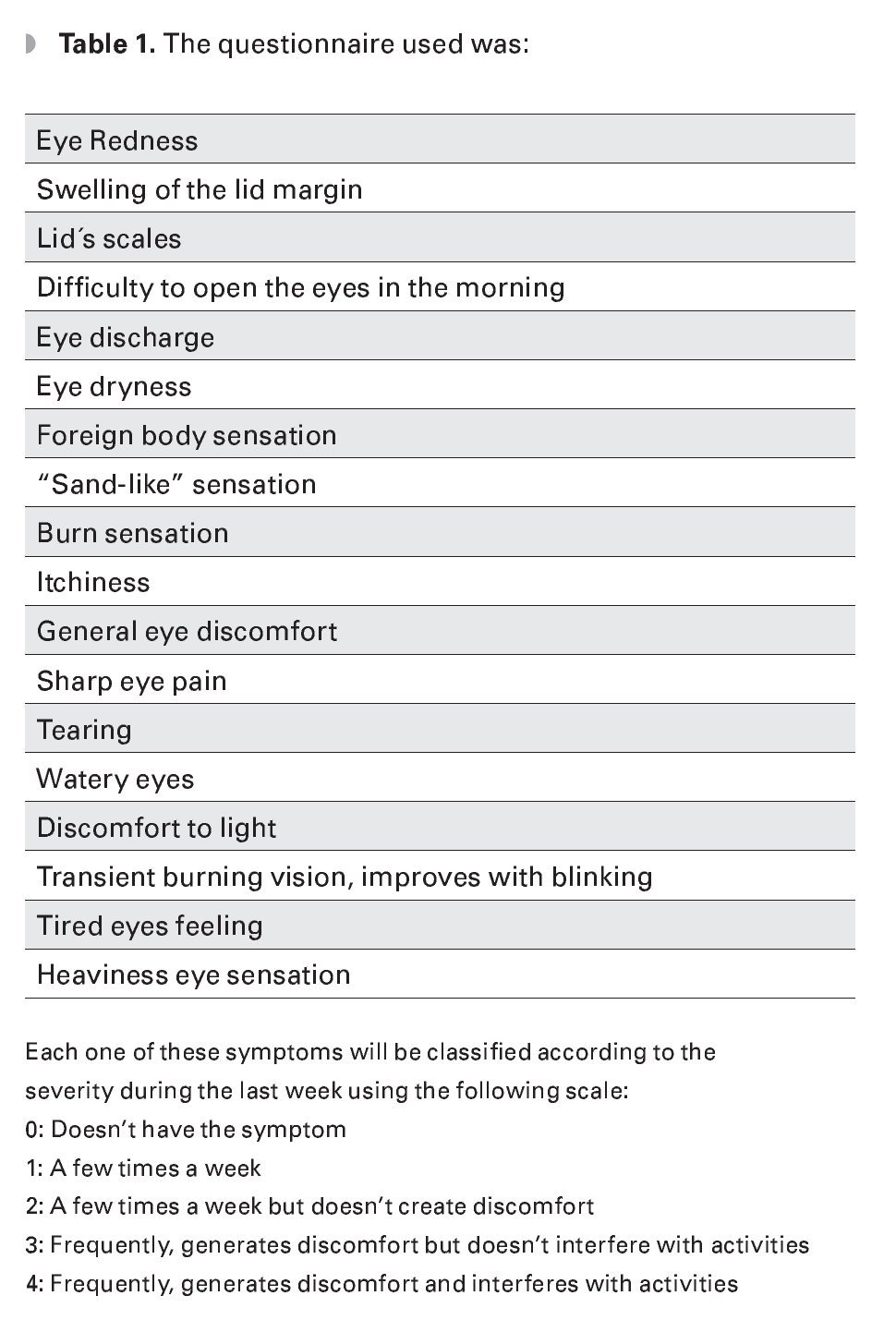
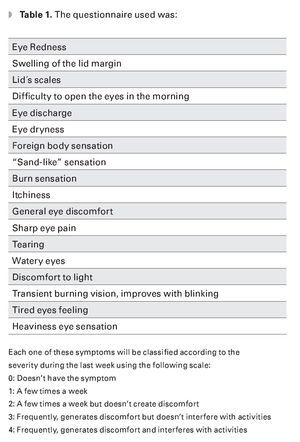
A study was done at the Instituto de Oftalmología Fundación Conde de Valenciana where we did the Schirmer type I test with topic anesthetic application and a tear film break up time to the patients from this hospital. The sample was obtained from those patients with less than 13 points in the dry eye questionnaire. The questionnaire used was the Benitez del Castillo questionnaire (Table 1).25
We included all patients without dry eye symptoms with a score lower than 13 points, with any visual acuity and any refraction, and willing to be submitted to the study. We excluded all patients with dry eye symptoms, with a score higher than 13 points, patients who were unable to submit to the Schirmers test or the break up time test, with allergic response to the fluorescein, and patients using any ocular treatment in the last month.
For the making of the Schirmer test, we anesthetized the patients with sodic propacaine, 1 drop in each inferior cul-de-sac and we did the test ten minutes later. We put the TEAR FLOTM (Rose Stone Enterprises 9622 Baseline Road, Alta Loma, CA 91701) filter paper strips in one or both eyes to the patient while he kept blinking normally for five minutes, sitting in the exploration chair without any heavy lights or air drafts. Five minutes later, we extracted the strip and wrote down the millimeters moistened in the part of the strip that wasn't inside the eye. If the 30 mm moistened before the five minutes time had passed, then we extracted the strip and wrote down how long it took.
For the tear film break up time test, we put the patient at the biomicroscope, without any air current, with the lid lamp, and looking with 10 magnifications so we could see the whole cornea simultaneously. The patient was asked to blink and we determined how long it took for the first desecation zone to appear, writing down the number in the data paper.
¿ Results
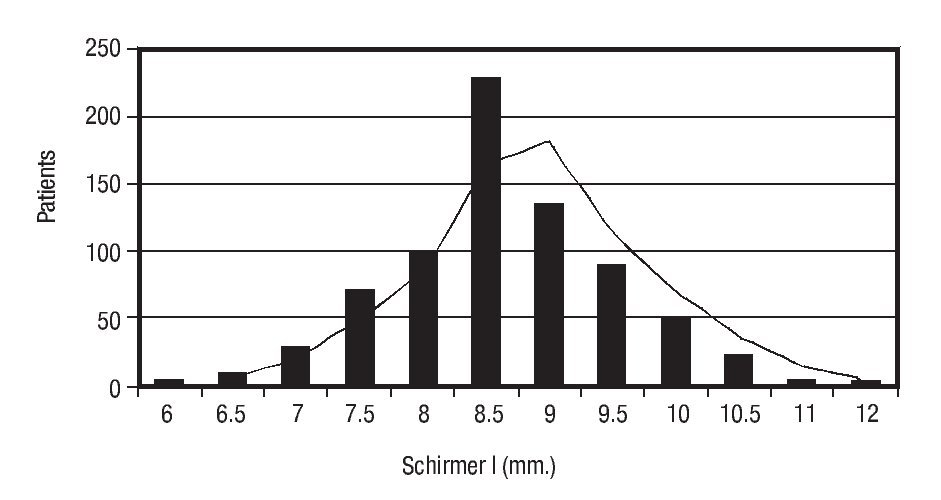
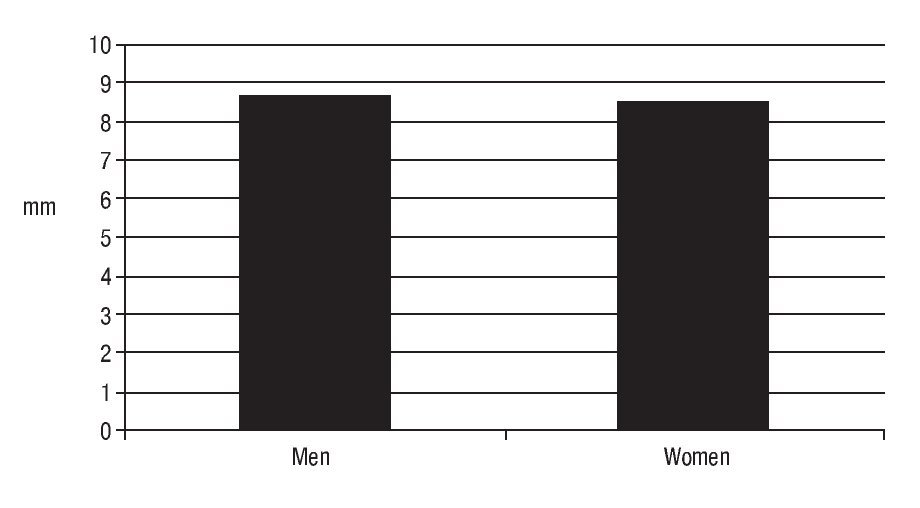
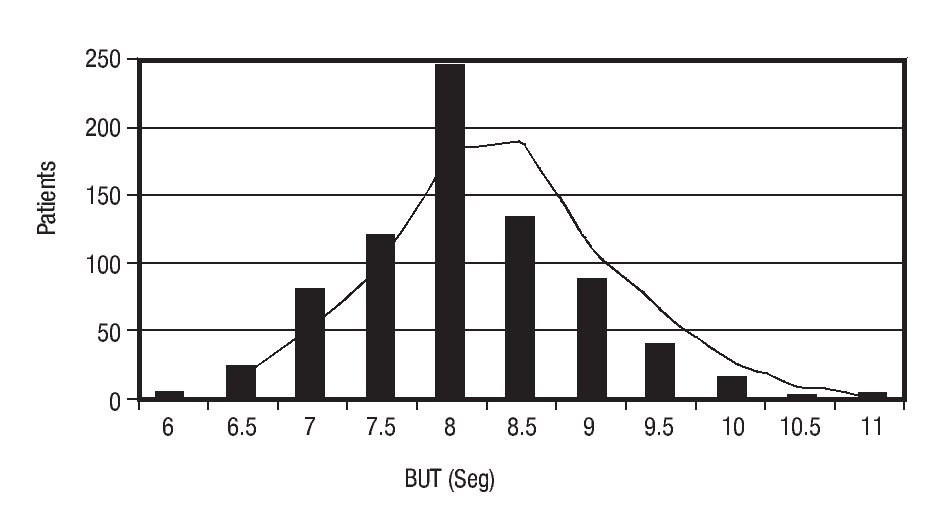
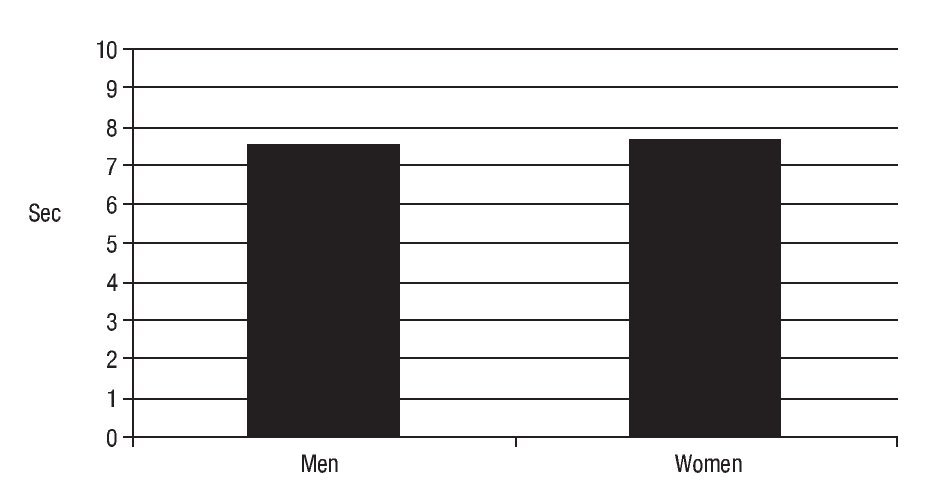
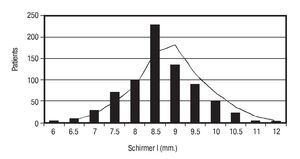
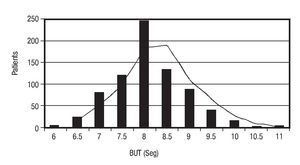
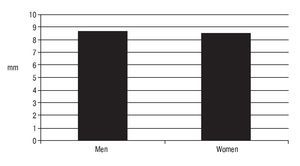
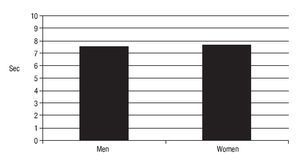
The sample obtained was from 747 patients, 381 men and 366 women, ages going from 18 to 77 years old, with an average of 34.5 years old. Regarding the Schirmer test, we obtained an average of 8.64 mm, with a standard deviation of 1.76 (6.88-10.4). In the tear film break up time test, we obtained an average of 7.60 seconds, with a standard deviation of 1.41 (6.19 - 9.01). The results obtained for women and men for the Schirmer test were an average of 8.59 mm for women and 8.71 mm for men. For the tear film break up time test, the data obtained was an average of 7.59 seconds for women and 7.63 seconds for men. As we can see here, the difference we found in the results for women and men were of no statistical significance (Figures 1-4).
¿ Figure 1. Schirmer I test.
¿ Figure 2. Tear film break-up time test.
¿ Figure 3. Schirmer test.
¿ Figure 4. Break up time test.
¿ Discussion
The best quantitative way to measure the tear production is the Schirmer test and the tear film break up time test. In this study, we chose the type I Schirmer test and the break up time test with local anesthesia, because with anesthesia we can partially isolate the basal secretion from the reflex tearing increasing the sensitivity of our study.
For a long time, the values used for the Schirmer test and the break up time test for diagnosis and for investigation purposes have been higher than those we have found in our study. Due to that in our daily practice we started noticing lower values in healthy patients, and since there isn't a consensus about what the normal values should be, we decided to perform this study.
Our study showed lower average values, on our population, than those found in the literature, so it might be interesting to perform further studies in different types of population that may suggests that our values can be related to environmental or racial factors.
The normal Gaussian distribution and the correlation between the two tests make us think that the results are statistically significant. It is also interesting to mention that we didn't find any statistical difference between the two tests, comparing men and women. The Schirmer and the break up time are very easy to test, inexpensive and do not represent any risk for the patient. Also, when made with an adequate normal standard value, the tests can provide very valuable information for the classification of our dry eye patients.
In further studies, we will look for a correlation between these non dry eye patients, the new values we found, conjunctiva cytology and tear osmolarity, so we can try to create a new qualitative, quantitative and histological classification for this group of patients.
Correspondence: Salomon Fermon.
Avenida de la Palma N°8-503. Interlomas.
Telephone: 5255 3605 1323. Fax: 5255 3605 1419.
E mail: sfermon@yahoo.com, www.cenofi.com