Objetivo: Describir los resultados quirúrgicos y visuales después de vitrectomía pars plana (VPP), en la cirugía de facoemulsificación complicada con fragmentos del cristalino retenidos.
Métodos: Se revisaron retrospectivamente los registros de 46 ojos y se describieron los hallazgos con una media de seguimiento de 13.5 ± 6 meses.
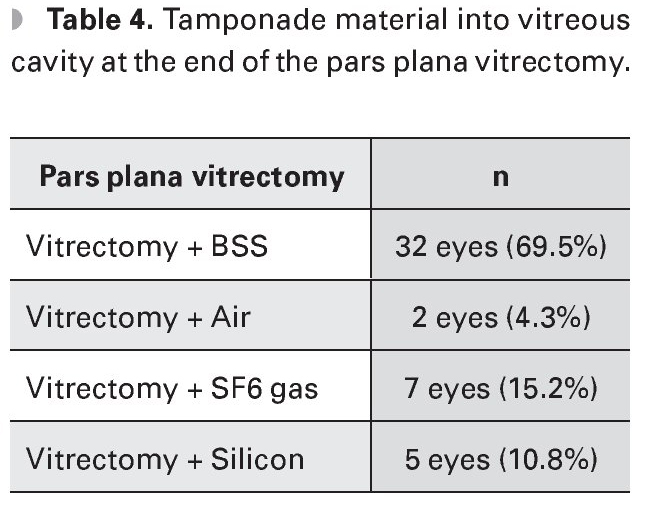
Resultados: La agudeza visual mejor corregida (AVMC) mejoró 0.27 logMAR y la presión intraocular (PIO) disminuyó 2.3 mmHg de la basal. La mayor mejora de la AVMC se observó cuando la VPP se llevó a cabo durante la primera semana (10.8%), y cuando se dejó solución salina balanceada (SSB) en cavidad vítrea (69.5%).
Conclusión: Los pacientes tienen mejores resultados visuales si son reintervenidos quirúrgicamente en la primera semana después de la complicación de la catarata y si se deja SSB en cavidad vítrea.
Objective: To describe surgical and visual outcomes after pars plana vitrectomy (PPV) in complicated phacoemulsification cataract surgery with retained lens fragments.
Methods: We retrospectively reviewed records of 46 eyes and described the findings with an average follow-up time of 13.5±6 months.
Results: The best corrected visual acuity (BCVA) improved 0.27 logMAR and IOP diminished 2.3mmHg from baseline. The greater improvement of BCVA was observed when PPV was performed within the first week (10.8%) and when balanced saline solution (BSS) was left in the vitreous cavity (69.5%).
Conclusion: Patients have better visual outcomes if they are surgically reintervened within the first week after cataract complication and if BSS is placed in vitreous cavity.
Introduction
Phacoemulsification is currently the preferred technique for cataract surgery. Continuous advances in technique and technology have made cataract surgery more efficient and safer than it was previously possible.
While phacoemulsification of cataract has many advantages over traditional techniques, the dislocation of lens material and/or intraocular lens into vitreous cavity remains a rare but potentially devastating complication. Successful surgical removal results in a satisfactory visual acuity.1
Current management for displacement of lens material and/or intraocular lens into vitreous cavity requires a pars plana vitrectomy (PPV) performed by a vitreous and retina surgeon. However, this is controversial and the debate continues about the optimal time for the PPV realization, as it depends of the individual characteristics of each patient. Ching-Long and colleagues suggest that a PPV performed immediately, leads to better visual results and lower percentage of complications.2 Lawrence and colleagues recommend PPV within the first seven days of the complication to reduce the risk of developing secondary glaucoma.3 Similarly, other authors prefer the early realization of PPV (less than two weeks after the complication), once the corneal edema and swelling have decreased, avoiding the cycle of inflammation induced by lens particles.1
A successful conservative management with topical and systemic treatment has been reported, with no significant differences in visual acuity, intraocular pressure (IOP) and complications compared to patients undergoing vitrectomy.4
The incidence of dislocation of lens particles into vitreous cavity in a teaching hospital is 0.8% (10 of 1 250 cases), of which 0.3% occur in experienced surgeons. The result informed for surgeons in training is 1.23%.1
Justus and colleagues reported that after the first VPP, the best corrected visual acuty (BCVA) improved from 0.15 ± 0.24 to 0.37 ± 0.33 log-MAR, and improved to 0.39 ± 0.32 logMAR with additional interventions.5
Anterior vitrectomy is clearly associated with a lower incidence of elevated IOP. Some authors recommend the performance of this procedure in all cases of luxated lens nucleus.5 Secondary glaucoma has been reported in 5-41% of cases when PPV is delayed.
Early recognition and appropriate management of this complication can minimize the extent of damage without compromising the pseudophakic condition or visual prognosis. Once this complication, it can be treated by a single surgical procedure in 25% of cases. Additional interventions have no statistical effect on the incidence of cystoid macular edema, secondary glaucoma, optic nerve atrophy or choroidal hemorrhage.5
The most common complication after the VPP is rhegmatogenous retinal detachment (RD-R) observed in 8.8%. There is a higher incidence of RD in eyes that received delayed PPV. This suggests that early PPV prevents or reduces the risk of DR.2
Eighty-five percent of patients who developed DR-R had vitreous prolapse during phacoemulsification which was not treated with anterior vitrectomy. Therefore they recommend this technique in complicated phacoemulsification surgery to avoid vitreoretinal traction.2
Methods
A retrospective, longitudinal, observational and descriptive study was realized.
Data were obtained from patients who underwent cataract surgery, and had lens material and/or intraocular lens retained into the vitreous cavity. They were treated with PPV from January to December 2008 at Asociación para Evitar la Ceguera en México, Dr. Luis Sánchez Bulnes Hospital. The information collected included the initial and final BCVA, measured by the Snellen chart and converted to numerical values: the logarithm of the minimum angle of resolution (log-MAR). The initial and final IOP was also included and measured with Goldman tonometer. Phacoemulsification surgery, implant of intraocular lens and whether or not anterior vitrectomy was realized, were data included in the study. The interval of time between phacoemulsification and the realization of PPV, the characteristics of posterior vitrectomy such the use of triamcinolone, ultrasound fragmentation of lens particles and use of heavy liquids were detailed. Finally, the complications that arose during the period immediately after the PPV and during follow-up were described.
Inclusion criteria were patients undergoing cataract surgery who and had lens material and / or retained intraocular lens into the vitreous cavity and were treated with PPV.
Exclusion criteria were traumatic cataract, spontaneous lens dislocation, corneoscleral wound, intraocular foreign body, previous retinal, glaucoma or cornea surgery, as well as patients with diagnosis of uveitis.
Results
Of a total of 2723 phacoemulsification surgeries performed from January to December 2008, 60 eyes had lens material and/or retained intraocular lens into vitreous cavity and were treated with PPV (incidence 2.2%). A total of 46 eyes for 45 patients were included in our study. The average follow up period was 13.5 ± 6 months (range six to 20 months).
The patient´s mean age was 68 years (range 56 to 84 years). Twelve eyes belonged to male patients (26%) and 34 to female patients (73.9%). The right eye was affected in 41.3% and the left eye in 58.6%.
The logMAR BCVA initial average was -1.52 (range -3.7 to -0.1). The final BCVA average was -1.25 logMAR (range 4.75-0).
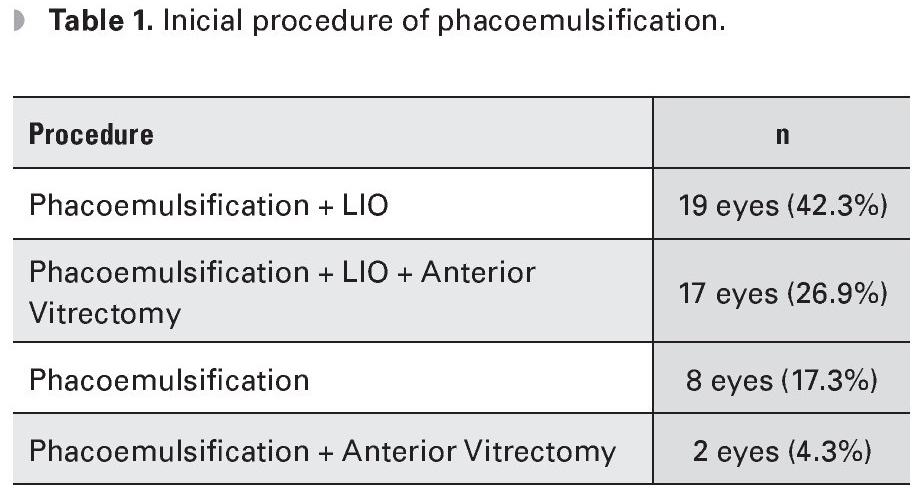
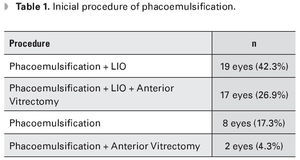
The average baseline IOP was 15.8 mmHg (range 0-44). The mean final IOP averaged was 13.5 (range 0-19). The most frequently performed procedure was phacoemulsification with intraocular lens implant (IOL) in 42.3% of cases, followed by phacoemulsification with IOL plus anterior vitrectomy in 26.9% of cases (Table 1).
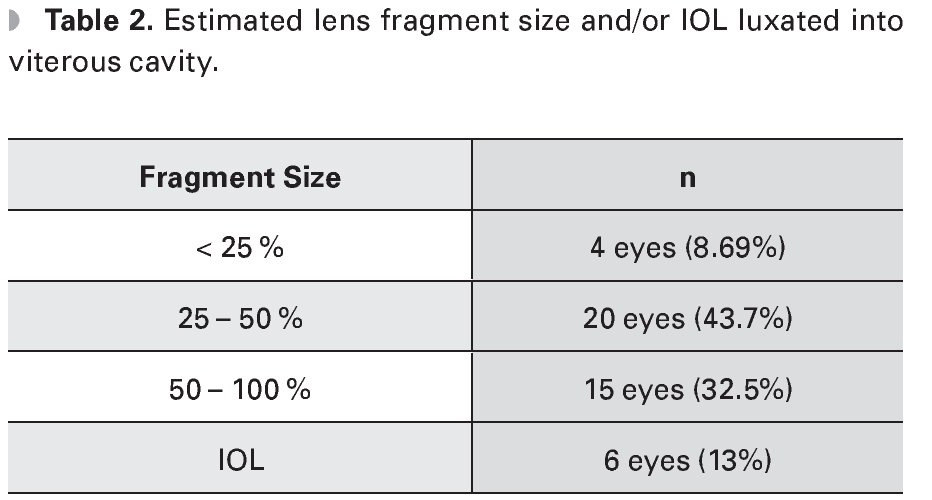
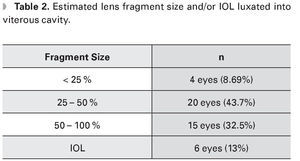
Dislocated fragment size was estimated by the anterior segment surgeon, being 25 - 50% in most cases (43.7%) (Table 2).
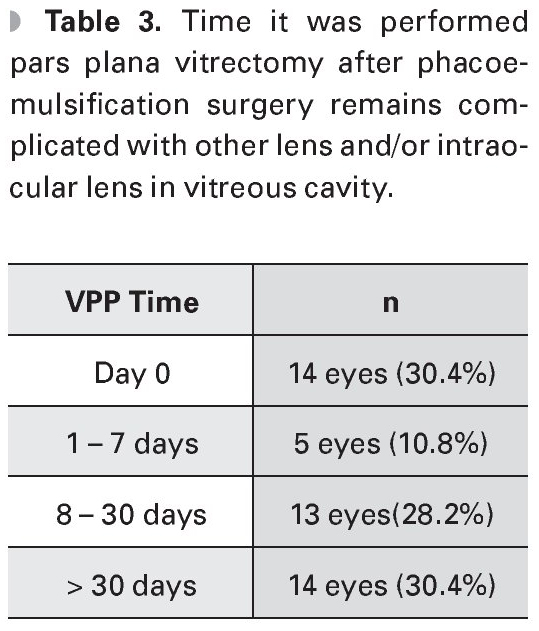
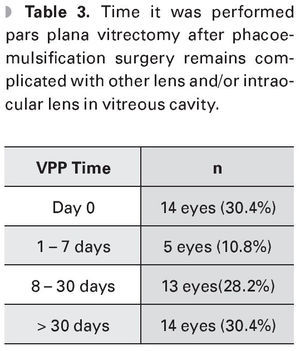
Regarding the time the PPV was performed, 30.4% of cases were intervened on day 0, 30.4% in the first week and rest of patients were treated after this time (Table 3).
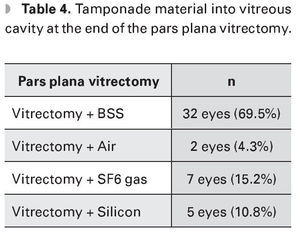
At the end of the PPV balanced salt solution (BSS) was left in vitreous cavity in 32 eyes (69.5%), air in two eyes (4.3%), gas sulfur hexafluoride (SF6) in seven eyes (15.2%), and silicone in five eyes (10.8%) (Table 4).
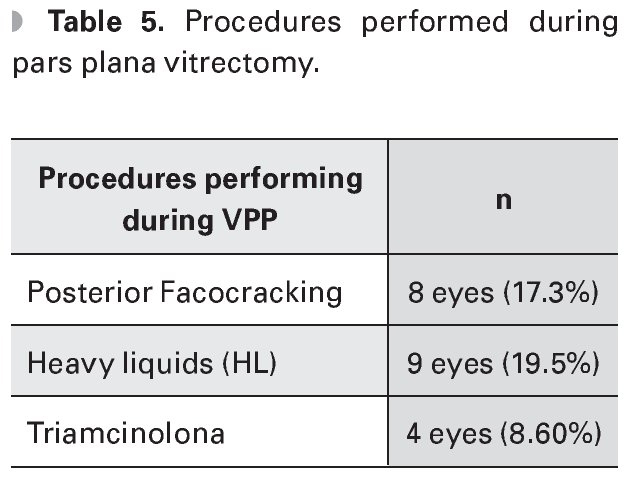
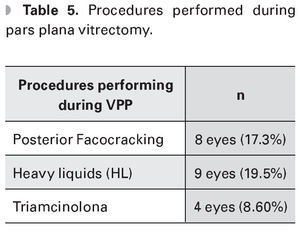
During the PPV posterior phaco-cracking was performed in eight eyes (17.3%), heavy liquids were used in 9 eyes (19.5%) and triamcinolone acetonide application in four eyes (8.69%) (Table 5).
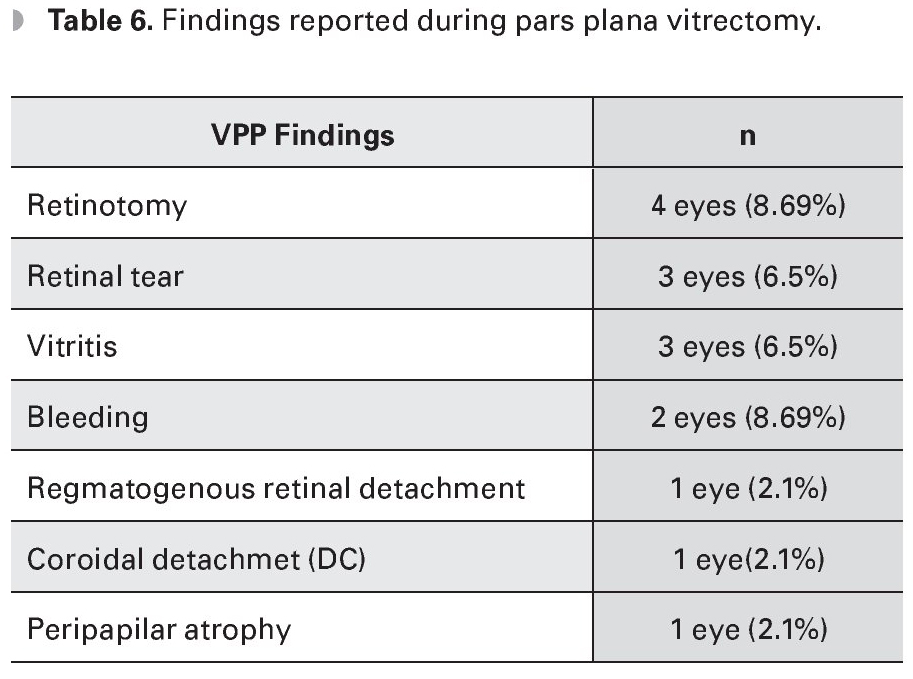
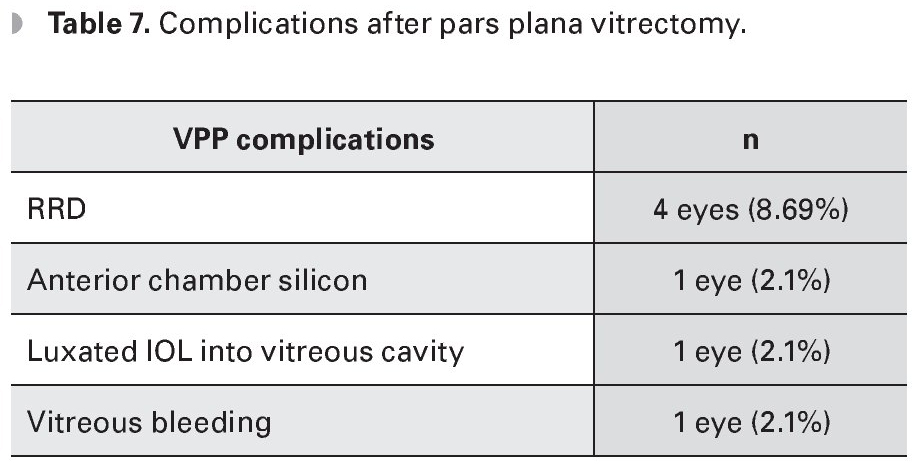
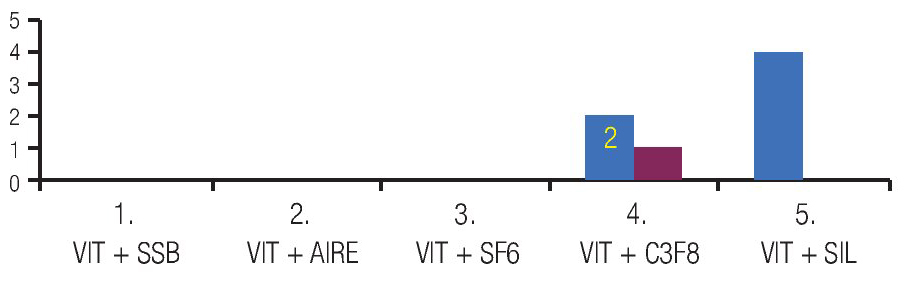
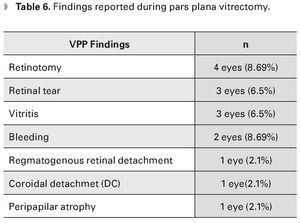
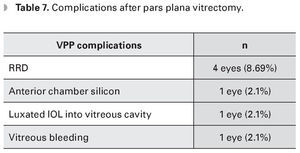
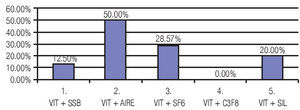
The findings reported during PPV were retinotomy in four eyes (8.69%), vitreal hemorrhage in two eyes (4.3%), retinal tear in three eyes (6.5%), rhegmatogenous retinal detachment (RRD) in one eye (2.1%), peripapillary atrophy in one eye (2.1%), vitritis in three eyes (6.5%) and choroidal detachment in one eye (2.1%) (Table 6). Complications after the PPV were RRD in four eyes (8.69%), anterior chamber silicone in one eye (2.1%), vitreous hemorrhage one eye (2.1%) and dislocated IOL into vitreous cavity in one eye (2.1%). In the latter case the patient underwent water/air exchange plus IOL removal, with no further complications (Table 7) (Figure 1).
Figure 1. First PPV.
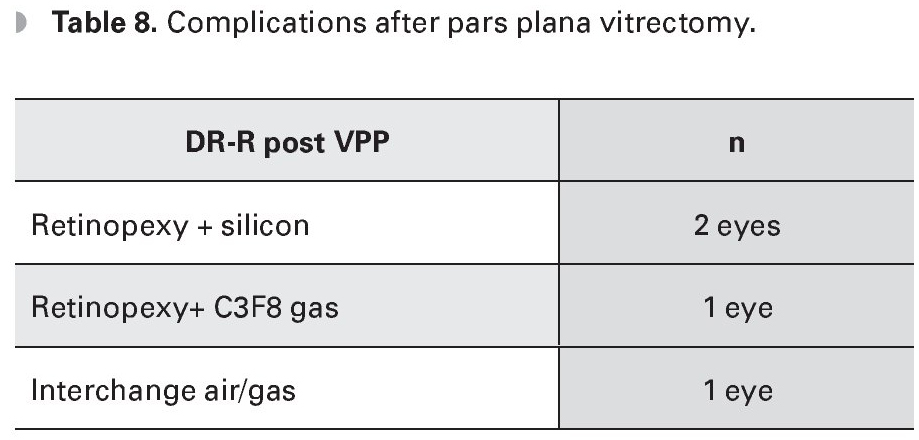
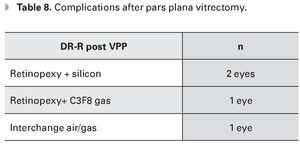
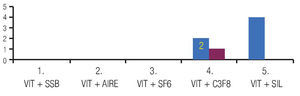
The four patients with RRD underwent a third surgery: water/gas exchange in one eye; escleral buckle plus water/silicone exchange in two eyes; and escleral buckle plus water/gas exchange in one eye; this latter patient had recurrent RRD and needed furter surgycal procedures (Table 8) (Figure 2).
Figure 2. Second PPV.
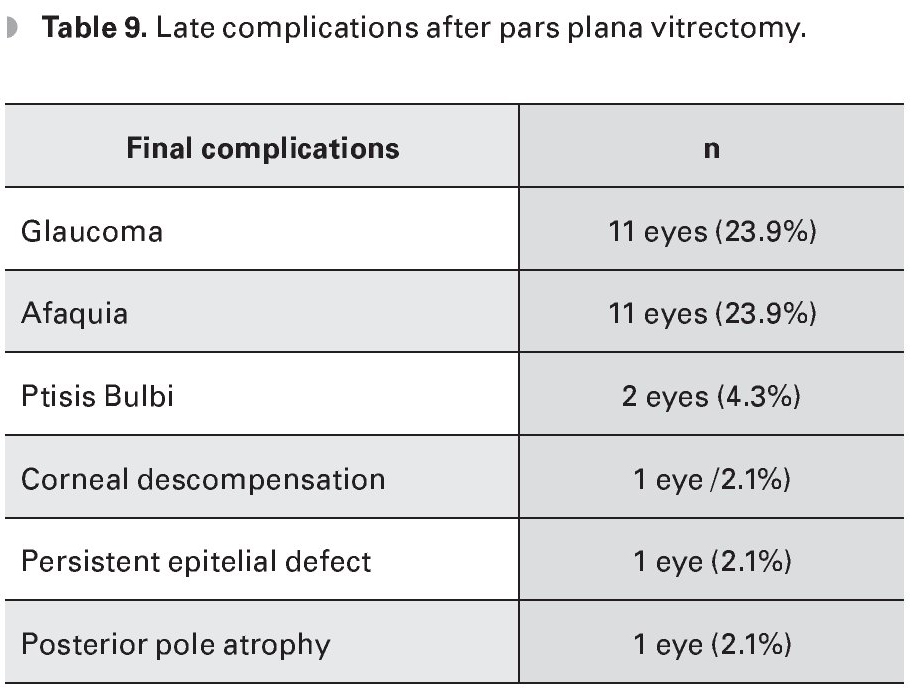
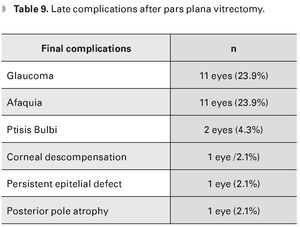
The late complications were glaucoma (23.9%), phthisis bulbi (4.3%), aphakia (23.9%), corneal decompensation (2.1%), persistent epithelial defect (2.1%), and posterior pole atrophy (2.1%) (Table 9).
Discussion
In most cases reported in our study, anterior vitrectomy was not performed to release vitreoretinal traction. This increases the risk of RRD which is the most common complication. Lawrence states that the performance of anterior vitrectomy and IOL sulcus placement is associated with less probability of obtaining a poor visual final prognosis.3
The chosen surgical technique to manage dislocated lens fragment depends on its size and hardness. If the fragment is soft and less than 25%, it can be removed by PPV without the use of additional instruments such as heavy liquids (HL) or posterior phacocracking. When the lens fragment is of grater lenticular hardness and has a larger size, the HL will effectively prevent the retinal trauma.6 In this study, the anterior segment surgeon reported in most cases a dislocated fragment size of 25-50%. During the PPV, posterior phacocracking was performed in 17.3% of cases, HL in 19.5% and application of triamcinolone acetonide in 8.69% of cases.
The IOL can be implanted during complicated phacoemulsification surgery in selected cases. It is preferable to assess the secondary IOL implantation during the VPP in cases with smooth or small dislocated lens fragment.6 In our series, IOL were implanted during phacoemulsification in 78% of cases. The ciliary sulcus was the most common site of implantation (60.8%).
Dislocation of lens material and/or IOL complicating phacoemulsification surgery represents a potentially devastating complication. Recent advances in both phacoemulsification and PPV techniques, as well as detection and treatment of complications have improved the visual prognosis in recent series compared with past literature.
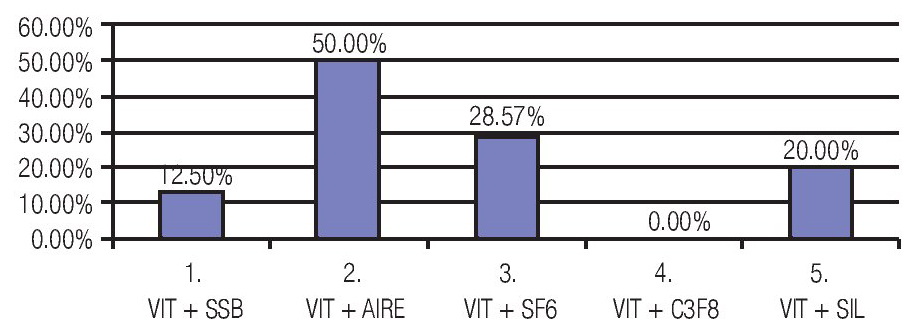
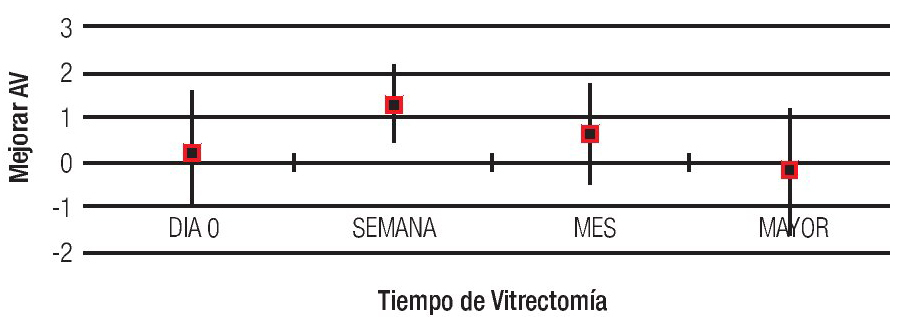
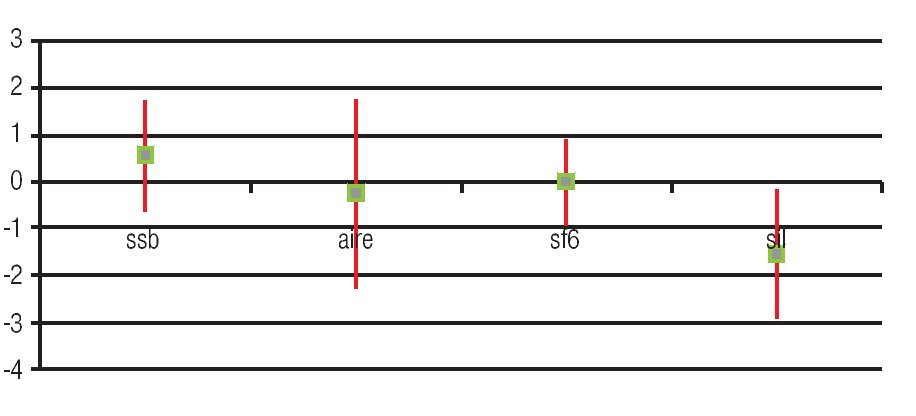
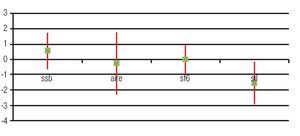
The best final visual acuity was observed in those patients undergoing PPV during the first week after complication (41.2%). It should be noted that the cases in which BSS was left in vitreous cavity were the less complicated too (Figures 3 and 4).
Figure 3. Improved of BVA for PPV time.
Figure 4. Box and Whisker plot graphic which shows the improvement in visual acuity by type of tamponade used during pars plana vitrectomy. Green Dot: average improvement of VA (log-MAR) (median). Line: standard deviation of 95% of patient.
Conclusions
Patients who underwent PPV after complicated phacoemulsification with lens fragments or IOL luxated into vitreous cavity, have better visual outcome if the surgical procedure is performed during the first week after complication. The most common complications that must be considered include retinal detachment, glaucoma and surgical aphakia.
Correspondencia:
Dra. Olivia Baldivieso.
Asociación para Evitar la Ceguera en México.
Vicente García Torres 46, Colonia San Lucas, Delegación Coyoacán,
C.P. 04030. México D.F., México.
Phone: 1084 1400.
E-mail: oli_baldivieso@hotmail.com