Cleft lip and palate is one the most common congenital malformations that affect human faces in all ethnic, economic level, and educational groups. It may cause speech and psychological problems. This study presents the skeletal and dental characteristics of cleft lip and palate patients treated with maxillary orthopedics, orthodontics and surgery during their infant and adolescence years.
MethodA retrospective cephalometric analysis study was performed in 2013 using the Dolphin Imaging System of 26 lateral head films and 26 posteroanterior X-rays of cleft lip and palate adult patients who received orthopedic, orthodontic and/or surgical treatment during their infancy and adolescence between 1969 and 1985. All X-rays were taken during 1995-2002.
ResultMost of the subjects presented a mesofacial growth pattern, a skeletal Class III maxilomandibular relation, a large mandibular body length, an increase in the vertical growth of the maxilla, and an increase in the facial, maxillary, nasal, intermolar and intercanine width, with a normal Overjet and Overbite and retroclined upper incisors.
De las malformaciones congénitas que afectan la cara del ser humano, la fisura labio-palatina es la más común, ya que se presenta en cualquier nivel socioeconómico, educativo, en todas las razas y causan gran repercusión psicológica por estar localizadas en la cara y pueden afectar el lenguaje del individuo. Este estudio define las características cefalométricas significativas en los patrones de crecimiento craneofacial y las características dentales de los adultos con fisuras labiopalatinas que recibieron tratamientos quirúrgicos y ortodónticos durante la infancia y adolescencia.
MétodoEstudio cefalométrico retrospectivo para analizar en 2013 por medio del Programa de Dolphin Imaging System 26 radiografías laterales de cráneo y 26 radiografías posteroanteriores de pacientes adultos con fisuras de labio y paladar hendido que recibieron tratamiento ortopédico, ortodóntico y/o quirúrgico durante su infancia y adolescencia desde 1969 hasta 1985. Todas las radiografías fueron tomadas de 1995 a 2002.
ResultadoLa mayoría de los pacientes presentan: patrón de crecimiento mesofacial, relación maxilomandibular clase III, longitud mandibular larga, aumento del crecimiento vertical maxilar, aumento de la anchura facial, maxilar, nasal, intermolar e intercanina, sobremordida horizontal y vertical adecuada, y los incisivos superiores retroinclonados.
In each individual, specific characteristics of anideal pattern about his or her physical configuration may be found; this «primitive underlying form», is frequently altered since the very moment of conception when the conflicts generated between the varied influences of genetic loads and those acquired by multiple intrinsic and extrinsic environmental factors become manifest in the preand postnatal periods. When an omission, error or neglect of the nature occurs, he possibility of balance and ideal harmony that is inherent in all life processes is becomes substantially changed by this primary circumstance. All these variables interrelate secondarily in determining the conditions that form the characteristic attributes of this individual.
In Mexico, we have the data provided by the RYVEMCE (Registration and Epidemiological Surveillance of External Congenital Malformations by its initials in Spanish), that indicates a rate of 1:1,200 live newborns and it increases to 1:800 when considering abortions and deaths.1 The cleft lip and palate represents one of the most common malformations and is susceptible to structural correction, and functional rehabilitation through the work of a medical (Genetics, Pediatrics, Plastic Surgery, Otolaryngology, Speech Therapy, etcetera) and dental (Pediatric dentistry, Orthodontist, Prosthetist, etcetera) interdisciplinary team.
The cleft lip may be unilateral or bilateral; when unilateral it is most commonly seen on the left side (70%). Approximately 85% of bilateral fissures and 70% of the unilateral ones are associated with a cleft palate. The cleft lip associated with cleft palate is more common in men, while the isolated cleft palate is more frequent in women. In general, the bigger the defect, the higher is the proportion in males. The isolated palatal fissure is a completely different entity to the cleft lip associated with cleft palate. The cleft palate may be complete of soft palate or secondary and incomplete of primary palate. The submucosal is an incomplete form of cleft palate difficult to detect visually during the immediate postnatal review, its frequency is 5 to 10% of all the palatal fissures.2 When minimal, it may go unnoticed, especially when language is considered to be adequate or normal, and when it is not compensated by a pharyngeal constriction mechanism.
It has been shown that siblings born from parents with cleft lip and cleft palate have a higher prevalence of the same anomaly, but not of isolated cleft palate. In 60% of children with cleft palate it is associated with another congenital malformation.3 Complete cleft palate is more frequent than a soft palate cleft.4
Green and col. observed that the age of the parents has an impact on the presence of cleft lip and palate.5 They reported that the parents of patients with this malformation are older than the parents of healthy children.
Saavedra, Yudovich and col. have demonstrated a probable relationship between patients with clefts and a facial morphology with an increased facial width of the parents.6
Ochoa and Vinageras in 1987, mentioned that on the basis of anatomical cleft lip-palate studies performed in corpses of children with these congenital malformations, it has been possible to obtain information about the anomalies of the muscular, nerve and bony structures.7-10
In the presence of a cleft lip, the muscle fibers of the orbicularis muscle do not intertwine on the maxilla, but continue in parallel with the margin of the cleft lip and in this way its integrity is divided causing the sphincter mutilated by the division to be unable to avoid the traction of the antagonistic muscles that insert into the commissure and produce lifting and distortion of the lip elements.
Fara in 1965,8 dissected and described the anatomy of the orbicularis muscle of lips that was later corroborated by other authors.9 He stated that the muscle at philtrum level on the cleft side is hypoplasic and does not extend to the entire length of the lip margin as it happens in the opposite side; this suggests a limitation of the muscle fibers to grow towards the midline.
Novoselov and Lavrentiev10 pointed out that they had found less differentiated, wide and large muscles in the superficial layers and narrow in the deep; the division of the orbicularis of the lips was due to the shift in its fiber's direction and to the lack of union of its main bundles in the deep surface. The most powerful bundle inserts on the base of the nose wing and plays an important role in the movement of the base of the nose wing of the cleft side, as well as the nasal septum on the healthy nasal side.
Many studies have been conducted to understand the anatomy of the velopharyngeal are ain normal conditions as well as in palatal clefts.11-16 These structures are involved in the production of language in such a way that when an alteration of their anatomy exists dysfunction and abnormal language occur. In normal anatomy, the muscular structures of the velopharyngeal area form a ring that is found to be broken in the cleft palate; the muscle fibers are directed from its lateral insertion towards the palate bone in the shape of a fan and form a raphe when they join in the middle portion.
In the cleft palate there are alterations in their insertion, distribution and muscle insertion; these are located and directed along the margins of the fissure, eventually finding sites for insertion in the posterior margin of the bony palate and may become hypoplasic.11
The pioneer work of Ortiz Monasterio in 1959 about the cephalometric evaluation of facial growth patterns in adult non-surgically treated individuals with cleft lip and palate, showed facial patterns with skeletal and dental distortions caused by the fissure, but no significant restrictions in growth patterns, indicating that the characteristic stigmas of the patient with cleft lip and palate were the result of the kind of surgical techniques used.17
In 1990, Yudovich, Ortiz Monasterio, Diaz Gonzalez et al. corroborate din a Mexican population there are significant changes in the cranial base of individuals with cleft lip and palate who did not undergo surgery. They described that their values are higher in all the linear and angular dimensions than in healthy individuals, probably because in the studied Mexican population there was a tendency for skeletal biprotrusion. The size of the mandibular body and ramus, as well as the Overjet, was found to be within normal parameters; this was due to the fact that the mandible was found in a normal position with respect to the craniofacial complex.18
The maxillary midline was diverted toward the affected side invariably as a result of the tendency of continuity of the maxillary arch, a finding that not been described previously.
Khoo Boo-Chai evaluated patients with bilateral cleft lip and palate surgery and reported varying degrees of maxillary collapse in approximately half of the cases. In those cases where the lip had been closed, the restoration of the musculature brought a favorable effect on the maxillary arch.19
Hagerty and Hill in 1963 made a comparative growth analysis between surgically-treated patients and nonsurgically treated patients, their report did not present a significant difference in bone growth between the two groups. As far as the dental analysis is concerned, it describes a lingual version of the incisors due to the post-closure lip pressure, as well as a posterior displacement because of the lack of support.20
Shaw WC, Dahl E, et al in 1992 reported the methodology used and the conclusions obtained in comparative studies between six different international institutions.16 To achieve the accepted results we depend on several factors, such as complexity, cost and need for treatment. Standardization, centralization of the institutions and the involvement of operators which includes good organization and coordination in implementing adequate time, sequence, and also balance during treatment may provide the best results. This study showed good results with the vomerian fl ap procedure for palatal closure. However, it presented inadequate effects in primary bone graft with presurgical orthopedic treatment.
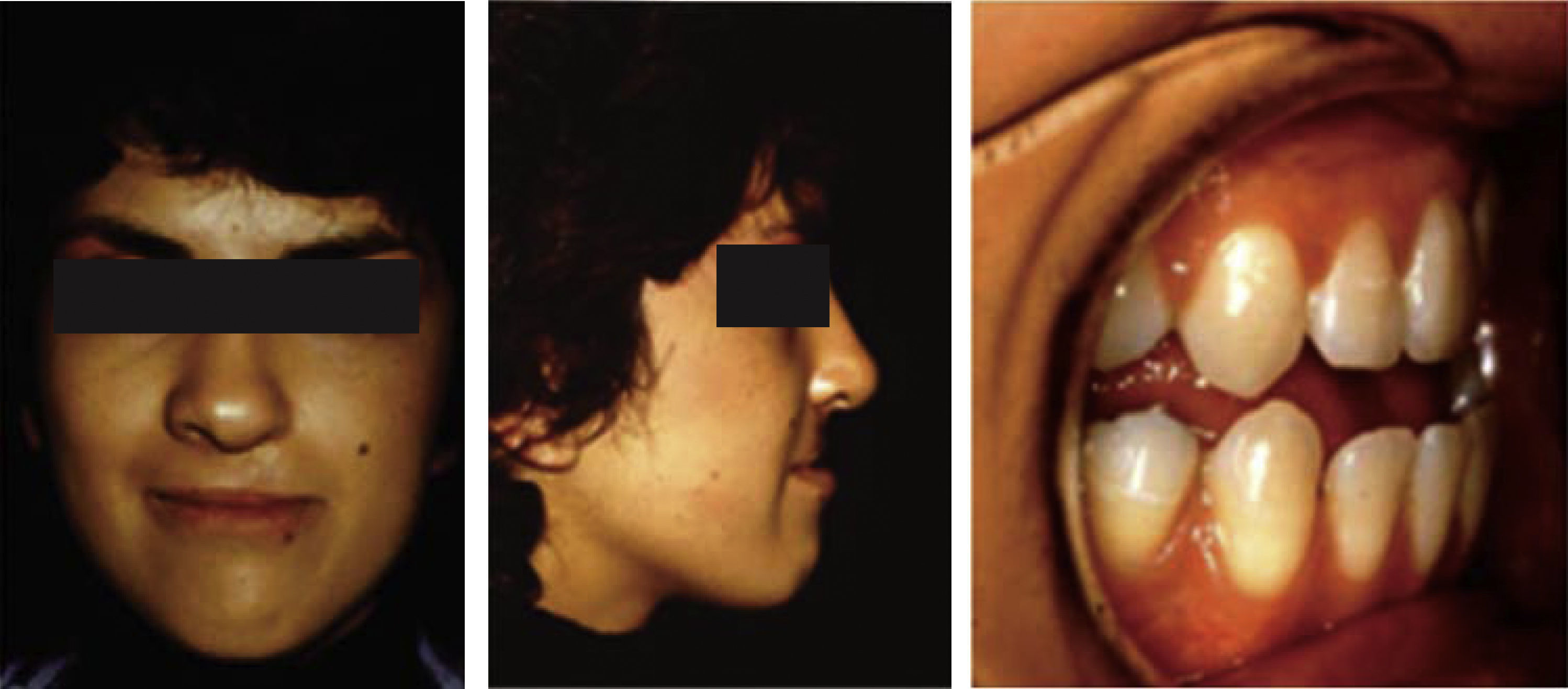
Given that in Mexico, there is a care center for children with cleft lip and palate in the Hospital «Dr. Manuel Gea Gonzalez» in Mexico City, where comprehensive, multi-disciplinary and avant-garde care is provided, in order to lead them to develop their optimum potential it is necessary to know the growth characteristics of adults with cleft lip and palate that received orthopedic, orthodontic or surgical treatment during childhood and adolescence (Figures 1 to 8).
Twenty-six lateral head films and 26 posteroanterior (pa) radiographs of adult patients (18 years of age and older) with cleft lip and palate that ended their orthopedic, orthodontic and/or surgical treatment during childhood and adolescence from the year 1969 to 1985 were traced and their cephalometric values, assessed. The X-rays were taken between the years 1995 to 2002. The following cephalometric measurements were analyzed:
LATERAL CEPHALOMETRIC MEASUREMENTS- •
SNA angle
- •
SNB angle
- •
ANB angle
- •
Go-Gn -SN angle
- •
Facial depth
- •
Facial axis
- •
Facial cone
- •
Mandibular plane angle
- •
Maxillary depth
- •
Maxillary height
- •
Palatal plane
- •
Cranial deflection
- •
Anterior cranial length
- •
Posterior facial height
- •
Ramus position
- •
Porion location
- •
Body length
- •
Facial convexity
- •
Lower facial height
- •
Upper molar position
- •
Lower incisor protrusion
- •
Upper incisor protrusion
- •
Lower incisor proclination
- •
Upper incisor inclination
- •
Overjet
- •
Overbite
- •
Interincisal angle
- •
Occlusal plane inclination
(Appendix 1. Definition of the lateral headiflm cephalometric points).
POSTEROANTERIOR (PA) CEPHALOMETRIC MEASUREMENTS- •
Maxillary intermolar width
- •
Intercanine width
- •
Dental midline
- •
Maxillo-mandibular width
- •
Nasal width
- •
Maxillary width
- •
Mandibular width
- •
Facial width
- •
Dental midline to maxillo-mandibular midline
- •
Occlusal plane inclination
- •
Molar relationship to maxilla and mandible
- •
Maxillo-mandibular midline
(Appendix 2. Definition of posteroanterior(pa) cephalometric points).
RESULTSOf the 26 patients who received orthopedic, orthodontic and surgical treatment during their childhood and adolescence, 13 were male and 13 female, with an age range from 19 years 7 months to 39 years of age and an average of 29 years 1 month. Eight of them showed a complete unilateral right cleft lip and palate, 12 a complete unilateral left cleft lip and palate and 6 showed complete bilateral cleft.
LATERAL HEAD FILM ANALYSISAt the end of treatment, 15 out of 26 patients showed a normal or mesofacial growth pattern, with an adequate facial axis (57.69%, average 88.61o) and a normal mandibular plane angle (55.17%, average 26.42o) and 11 patients exhibited a dolichofacial growth pattern by a decrease of the facial axis (42.30%, average 80.8o) and an open mandibular plane angle (41.38%, average 36.62o). Eighteen patients presented maxillary retrusion (average maxillary depth 82.83o) and in 8 patients the position was adequate (average maxillary depth 89.56o). The anterior cranial length was normal in most patients (51.72%, average of 73.2mm).
The majority of the patients (93.10%, average maxillary height 64.69o) showed excessive vertical growth of the naso-maxillary complex and 82.76% (average of palatal plane 10.55o) of the patients presented a backward rotation of this complex in the counter-clockwise direction. However, this increase in the vertical dimension did not affect the lower face height so 57.69% (average 49o) of the patients presented an adequate lower facial height. In 9 of the 26 patients an increased lower facial height was found (34.61%, average 54.5o).
57.69% (average of ANB is -1o) of the patients presented a skeletal class III maxillomandibular relationship as a consequence of the predominant maxillary retrusion (42.31%, average maxillary depth 82.83o) and an increase of the mandibular body length (82.76%, average 88.36o). 57.69% (average ANB 4.9o) of the patients had skeletal class II maxillomandibular relationship.
In addition, most patients (72.14%, average of 17.27mm) showed a good position of the upper first molars and in 82.76% of them Overjet was obtained (average 1mm). 51.72% of the patients obtained an overbite (average of 1.5mm) within normal parameters. 65.51% of the patients (average upper incisor inclination 17.26o) presented retroclined incisors and 55.17% (average lower incisor inclination 21.63o) had a normal lower incisor inclination so the interincisal relationship was retroclined (51.72%, average interincisal angle 144.31o).
FRONTAL ANALYSISOf the 26 patients, 10 maintained (average 128.9mm), 7 patients showed an increased facial width (average of 134.5mm) and 9 patients a decreased facial width (average of 119mm). 46.15% of the cases presented a correct maxillary width (average 72.22mm) which indicates that there was an adequate transverse development of the maxilla, while only 19.23% of the patients presented a decreased width (average 59.2mm).
The increase in the maxillomandibular width values shown by the majority of patients (73.08%, average of 13.65mm) indicates a tendency towards skeletal cross bite, however it is contrasted by an increase in the maxillary intermolar width observed in 16 cases (61.54%, average of 59.09mm).
In regard to the mandibular width, 61.54% of the sample presented an increase at molar level (average of 86.44mm) and 50%, an increase in intercanine width (average of 32.15mm). In most patients (65.38%) an increased nasal width was found (average of 34.73mm).
30.76% (average 0.5mm) of the patients had the maxillary and mandibular midlines within normal values showing that an adequate intermaxillary symmetry was accomplished, which coincides with a good symmetry in the dental midlines in most cases (61.54%, average of -0.7mm). Additionally, in 80.77% of the patients an adequate occlusal plane inclination was achieved (average of -0.5o).
DISCUSSIONCranial base length: In 1965, Ross described that children with cleft lip and palate had a shorter cranial base length than children without fissures.14,21,22 Grayson and col in 1987 found an eleven percent reduction of the cranial length in patients with cleft lip and palate.23
Ross in 1965, Krogman and col in 1990 and other authors found that patients with cleft lip and palate have a longer cranial base length than normal parameters and explained that this length is composed of a long anterior cranial base length and a long anterior posterior base length.15,22
In 2010 Gonzalez and Velazquez studied 12 patients (8 males and 4 females), with cleft lip and palate, with a range of age of 6-8 years who had previously received some kind of treatment. The patients were Mexicans native from the State of Mexico. Patients of both sexes showed alteration in the posterior cranial length.24
In our study of 29 patients, 55.72% of them had a normal anterior cranial length.
Maxilla position: It has been theorized that patients with cleft lip and palate have a delay in maxillary growth that causes maxillary retrusion.22,25-28 Many authors agreed that the delay was actually an inherent consequence of the fissure.22,25-28 In support of this argument, Dahl, Bishara and Nakamura and col. found no differences in the sagittal dimension of patients with cleft lip and palate that underwent surgery compared with those who did not.21,29,30 It was also suggested that the maxillary deficiency was caused by the initial malformation and not by the surgeries.
There is abundant evidence that the maxillary complex grows properly when a child with cleft lip and palate does not have the palate surgicallyrepaired.31,32 The evidence is overwhelming: the cleft lip and palate repair with any popular surgical technique translates into growth inhibition of the maxillary complex.33-36
Donoso F, Pantoja F. (2007) demonstrated in a comparative study of sagittal maxillary growth in unilateral cleft lip and palate surgically-treated patients who did not receive presurgical-orthopedic treatment. The size of the study group was 10 children and 10 controls with an average age of 8.3 years. The sagittal maxillary growth of children with cleft lip and palate in this study did not differ significantly from the group of non-affected children with similar age range and a direct relationship of consanguinity.37
G. Schultes and col. (2000) performed a study on 30 patients with complete unilateral cleft lip and palate and 30 patients with cleft lip and palate who received orthodontic and surgical treatment with an average age of 18.9 years. In the cephalometric radiographs of patients with complete fissure an average of 76.8o SNA was shown indicating maxillary retrusion and the anterior facial height decreased which implies a deficiency of the vertical dimension of the middle third.38 In our study, we looked at patients who received orthopedic, orthodontic and surgical treatment during their childhood and adolescence. The average age was 29.2 years and only 27.59% of the 29 patients achieved an adequate position of maxilla: 68.97% presented maxillary retrusion.
We can summarize that the total result of maxillary growth and position depends on many factors such as the genetic load and severity of the cleft lip and palate, the power of individual growth, scar formation, the orthopedic, orthodontic and surgical management, patient cooperation, etcetera.
Mandibular length and growth pattern: In 1973, Chierici and col. published a study in which they described how the formation of cleft palate in Rhesus monkeys was induced. The results indicate that each monkey with palate constriction due to a «mechanical compensation» influenced a backward rotation of the mandible and an increase of the mandibularangle.39
Few studies have reported if the severity of the cleft has some connection with the speed of growth or the size or shape of the mandible. One of the previous studies observed that patients with more extensive fissures had a significantly shorter mandibular length.40
Another study found a significant inverse association between an increase in the palatal fissure size and a decrease of the mandibular body length.41 Liao and Marte tried to explain this association with a functional compensation of the mandible in response to the decrease in the permeability of the nasal airways; they explained that, as the fissure becomes larger nasal permeability decreases, causing the mandible to compensate and rotate backwards opening the mandibular angle. This leads to a short mandibular body length.42 However, in 1982 Long and col. suggested that patients with cleft lip and palate and severe maxillary retrusion may be considered as a result of a more severe fissure and in order to compensate for the maxillary deficiency, the mandibular size increases.42 In our study, 82.76% of the patients had an increase of the mandibular body length. However, the majority of them had a normal mandibular rotation or a mesofacial growth pattern (58.62%) and 41.38%, a posterior or dolichofacial mandibularrotation.
Dental inclination: Several authors such as Ortiz M. and col in 1958 and Bishara S. in 1973 conducted studies on dentofacial relationships in non-surgically treated patients with cleft lip and palate. They found that the upper incisor inclination of the patients with cleft palate and cleft lip and palate does not significantly differ from that with the group without fissures. Patients with cleft palate presented retroclined upper incisors and patients with cleft lip and palate had proclined upper incisors.17,29
In 1969, Ross mentioned that there is a distortion of the dentoalveolar structure, i.e. the teeth and the alveolar bone support. We compared the eruption of the upper incisors in patients with and without cleft lip and palate and differences in relation to the basal bone were shown; that in patients with clefts, the upper incisor proclination was caused by the palatal scar.27 In our study, it was also found an upper incisor retroinclination (65.51%) and a normal inclination of the lower incisors (55.75%).
Noother studies have been found that analyze skeletal and dental features of cleft lip palate patients through a posteroanterior radiograph to observe the facial, maxillary and nose widthand the deviation of the dental and the maxilla-mandibular midline so we cannot compare our study with other researchers.
CONCLUSIONAdult patients with cleft-lip-palate who received orthopedic, orthodontic and surgical treatment during their childhood and adolescence, have similar skeletal and dental features:
- 1.
Mesofacial growth pattern with a dolichofacial tendency.
- 2.
Skeletal Class III caused mainly by maxillary retrusion.
- 3.
Long mandibular body length.
- 4.
Increased vertical maxillary growth.
- 5.
Lingual inclination of the upper incisors.
- 6.
Increased facial, maxillary and nasal width.
- 7.
Increased intercanine and intermolar width.
- 8.
Although there is an adequate development of the maxilla, there is a tendency towards a skeletal crossbite that is compensated by an increase in the intermolar width.
- 9.
Through combined orthopaedic, orthodontic and surgical treatment of these patients it was possible to obtain a proper dental and skeletal symmetry.
The cephalometric analysis of the skeletal and dental characteristics of adult patients with cleft lip and palate who received orthopaedic, orthodontic and surgical treatment during their childhood and adolescence will be useful to refine future treatment protocols and, therefore, contribute to obtain the best possible function and aesthetics to improve the quality of life of patients with cleft lip and palate, their families and society.
The cephalometric analysis of the skeletal and dental characteristics that present the adult patients with cleft lip and palate that received orthodontic treatment and surgical orthopaedic during their childhood and adolescence, it will be useful to refine future treatment protocols and, therefore, contribute to obtain the best possible function and aesthetics to improve the quality of life of patients with cleft lip and palate, their families and society.
Definition of lateral cephalometric points.
Na: anterior point of the frontonasal suture. Ba: posterior-inferior point the occipital bone in the anterior margin of the foramen magnum. Po: higher point of the ear canal meatus. Or: lowest point of the orbital rim. Pt: intersection of the upper and posterior walls of the pterygomaxillary fissure. ANS: front end of the anterior nasal spine. PNS: back end of the posterior nasal spine. A: deepest point of the curve of the maxilla between ANS and the edge of the dental alveolus. Pm: point where the curvature of the anterior border of the symphysis changes from concave to convex. Pg: most anterior point of the symphysis. Gn: more anterior and inferior point of the contour of the chin between Pg and Me. Go: formed by the intersection of the mandibular plane with a tangent to the posterior margin of the ramus. Me: lowest point of the contour of the symphysis. Xi: point located in the center of the ascending ramus of the mandible. Cf: point located at the intersection of the Frankfort plane and its perpendicular tangent to the posterior wall of the pterygomaxillary fissure. Cc: cephalometric point formed by the intersection of the Ba-Na and the Pt-Gn line. DC: point that represents the center of the condyle on the Ba-Na plane. Ai: incisal edge of the upper incisor. Ar: radicular apex of the upper incisor. Bi: the incisal edge of the lower incisor. Br: radicular apex of the lower incisor. A6: point on the occlusal plane determined by a perpendicular tangent to the distal surface of the upper first molar. B6: point on the occlusal plane determined by a perpendicular tangent to the distal surface of the lower first molar.
Definition of the posteroanterior cephalometric points.
ZL/ZR: more internal pointof the fronto-zygomatic suture at the outer margin of the orbital rim. ZA/AZ: center of the root of the zygomatic arc. ANS: center of the anterior nasal spine located in the intermaxillary suture. JL/JR: deepest point of the zygomatic-alveolarcrest. AG/GA: deepest point of the antegoniac notch. Me: mid-point of the bottom margin of the symphysis. Posteroanterior cephalometric planes: Midsagittal: line that passes through the center of the crista galli apophysis and ANS. Frontal dental: line of JL-AG and JR-GA. Frontal Facial: line of ZL-AG and ZR-GA. Occlusal plane: passes through the line of occlusion of the molars. Z plane: joins ZL-ZR points.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia.