To characterize radiographically the periodontal ligament thickness (PLT) and pain perception (PP) at the beginning of orthodontic treatment by activating and applying infrared laser of 810 nm each month for three months.
MethodologyIt was a quasi-experimental, descriptive and longitudinal study with a non-probabilistic sample consisting of 10 patients from the clinic of Orthodontics and Orthopedics at the Autonomous University of Sinaloa. 200 measurements were performed in teeth #11 and 12 (laser-treated); and 21 and 22 (non-treated control). To measure the PLT periapical radiographs were analyzed with Motic software 3V Advance. For PP determination, visual analog scale (VAS) was used. Descriptive statistical analysis was performed with SPSS v-19 (confidence interval of 95%).
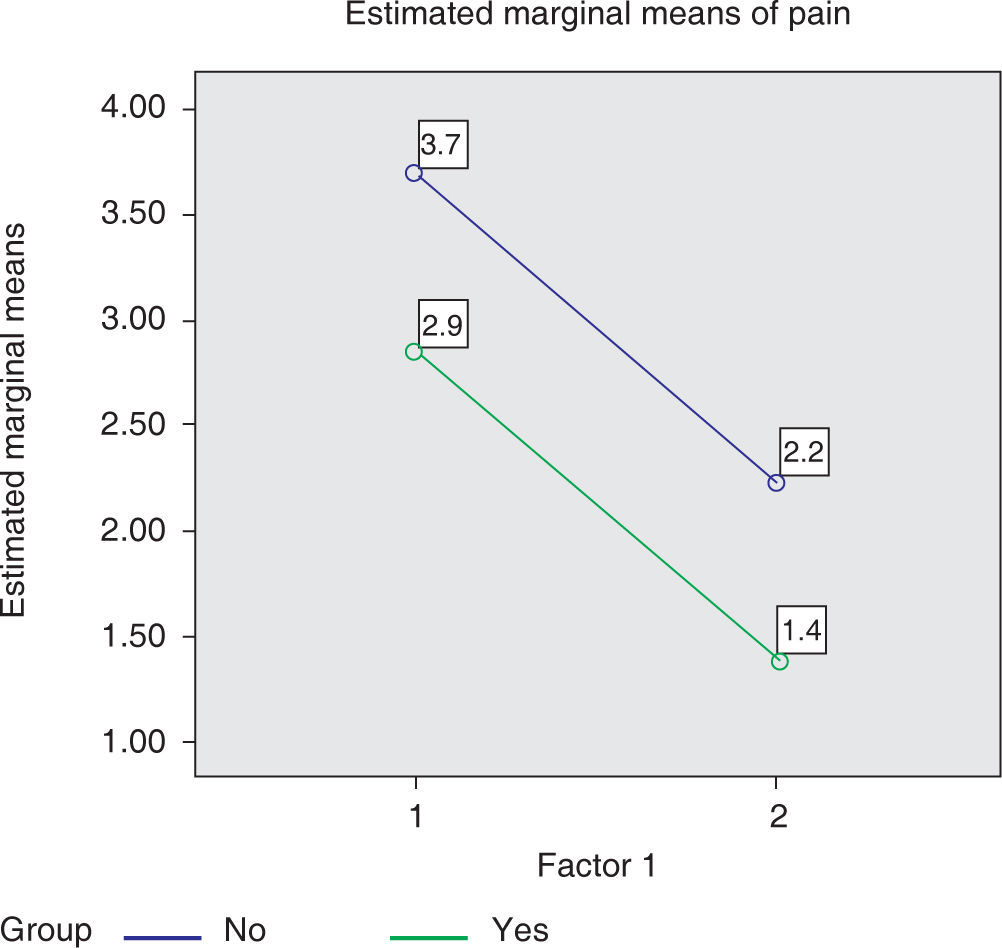
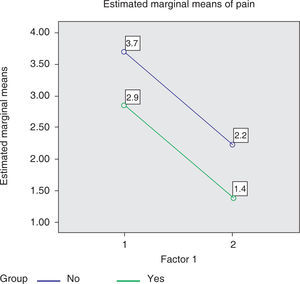
ResultsIn laser-treated teeth, PLT increased significantly 0.719 μm from the first to the second measurement and decreased 0.648 μm in the third measurement. In non-treated control teeth, PLT increased averaging 1.011 μm without significant change in the third measurement. PP in control teeth averaged 3.7 ± 3.2 on the VAS scale in the first measurement and 2.3 ± 2.3 in the second; while in the irradiated zone they averaged 2.9 ± 2.8 in the first month and 1.4 ± 1.2 in the second.
ConclusionWith laser treatment, PLT is significantly reduced in comparison to the group that did not receive the treatment. At one and two months of treatment, average of PP decreased both in teeth where the laser is applied as in those without.
Caracterizar radiográficamente el grosor del ligamento periodontal (gLPD) y la percepción dolorosa (PD) al inicio de tratamiento ortodóntico activando y aplicando láser infrarrojo de 810 nm cada mes durante tres meses.
MetodologíaEstudio cuasiexperimental, descriptivo, longitudinal, muestra no probabilística de 10 pacientes de la Clínica de Ortodoncia y Ortopedia de la Universidad Autónoma de Sinaloa. Se realizaron 200 mediciones en las piezas 11 y 12 (con tratamiento láser); y 21 y 22 (sin tratamiento). Para medir el gLPD se analizaron radiografías periapicales con el software Motic Advance 3V. Para la PD se usó la escala visual analógica (EVA). El análisis estadístico descriptivo se realizó con SPSS v-19 (intervalo de confianza de 95%).
ResultadosEn las piezas tratadas con láser, el gLPD aumentó significativamente 0.719 μm de la primera a la segunda medición, y disminuyó 0.648 μm en la tercera medición. En las piezas control, el gLPD aumentó promediando 1.011 μm sin cambio significativo en la tercera medición. La PD en las piezas control en la escala EVA promediaron 3.7 ± 3.2 en la primera medición, y 2.3 ± 2.3 en la segunda; mientras que en la zona irradiada promediaron 2.9 ± 2.8 en el primer mes y 1.4 ± 1.2 en el segundo.
ConclusiónEl gLPD disminuye significativamente al aplicar el láser con respecto al grupo que no se le aplicó tratamiento. El promedio de la PD al mes y a los dos meses de tratamiento, disminuyó tanto en las piezas donde se aplicó el láser como en las que no.
Laser radiation has been given numerous utilities in the medical area; various diseases can be treated or cured through its use. The first publications in the area of dentistry were associated with analgesic properties, where the results demonstrated that its implementation resulted in lower levels of pain in the visual analogue scale (VAS). Its application also generated a significant impact on cases of bone remodeling and anti-inflammatory effects in periodontal tissue.1–3
Among the commonly used types of laser there are the solid-state ones Er:YAG (λ = 2,940 nm), with effective absorption in water and hydroxyapatite; Er,Cr:YSGG (λ = 2780 nm), which is absorbed efficiently in hydroxyapatite; CO2 (λ = 9,400-10,600 nm), with good absorption in water; and others, such as the helium-neon (λ = 633 nm); GaAlAs (λ = 980 nm); the solid glass Nd: YAG laser (λ = 1,064 nm) and the infrared diode-laser (with l = 810 and 980 nm).4 The last-mentioned lasers with emission in the near infrared (NIR, near infrared) are characterized by being highly absorbed by the chromophores that are found in soft tissues, for example hemoglobin. This has the effect of obtaining excellent performance and efficiency in treatments of incision, ablation and coagulation, as well as antimicrobial action; that is due to the fact that tissue warming occurs in a very localized region and at a relative depth.4 On the other hand, lasers for hard tissue are highly absorbed by carbonate hydroxyapatite and chromophores in water, so it is possible to perform a hard-tissue fine ablation without heating the surrounding tissue.
Several lasers appeared in the middle of the 90, among which are those based on semiconductor diodes. The latter offered several advantages, such as their small size, price, and versatility. Diode-based lasers today represent a very important technological resource available for the dentist. Diode lasers can be used in several procedures that predominantly involve soft tissue and soft-tissue surgery,1–3 as well as therapy for the treatment of periodontal plates.4 Among the low power lasers (of the order of mW) there are the AsGa (λ = 904 nm); GaAlAs (λ = 830 nm) and He-Ne (λ = 632.8 nm) within the visible spectrum, in the red one; while Er:YAG laser that is applied on the hard tissues of the tooth, has high power –in the order of tens of watts–.4 The low-power laser has remarkable therapeutic activity in various types of pathologies, where scarring is important, and is considered as a great tissue regenerator since it increases availability of cellular ATP as well as photoelectric activity that acts over membrane polarization, re-polarizing it thus increasing its threshold of excitation. The above leads to an excellent anti-inflammatory and analgesic action.5 For its part, diode laser (λ = 904 nm), due to the specificity of photoelectric action of impulses, is a medium-power laser, which acts on the normalization of cell metabolism in inflamed tissues.6 With intense and highly focused laser beams, it is possible to cut and cauterize certain tissues in a fraction of a second, without damage to the surrounding healthy tissue.7
The analgesic effect of laser in dentistry, according to a study reported in 2008, 8 is based on the normalization of the concentration of some substances in the tissue, which interferes with the electrical message of sensory nerves. This fact has led to the application of low-intensity laser therapy seen as a method to help reduce pain induced by the orthodontic movement.9 Therefore, among several treatment alternatives to decrease pain of orthodontic origin, low-intensity laser is cited.10
In order to examine the effectiveness of low-intensity laser therapy in the reduction of pain caused by the first orthodontic archwire, Tortamano et al.11 conducted a pilot study with 60 orthodontic patients, divided into two groups, one under treatment with therapeutic application of laser and a placebo or control group. They found that the group where laser therapy was applied presented lower values in the scales of pain and pain duration was lower. In another study conducted by Turhani et al.12 with 76 orthodontic patients, divided in a control group and a group with laser therapy, the perception of pain was evaluated in the first 6, 30 and 54 hours after bonding. It was concluded that the application of low-intensity laser reduces the perception of pain in the first 6 and 30 hours. Fujiyama et al.13 performed a study with 90 patients (also divided in 2 groups: control group and low-intensity CO2 laser treatment group) in whom separator elastic modules were placed mesial and distal to the first molars. The authors concluded that the application of laser reduces pain perception according to the visual analog scale, without interfering with tooth movement.
Holmberg et al. found that laser can be effective as an adjuvant in the management of pain. However, no significant differences were found.14 In a study conducted in Brazil on 55 volunteers with fixed orthodontic appliances, divided into four groups called control, placebo, laser and LED; a visual analog scale (VAS) was applied at 2, 24, 48, 72, 96 and 120 hours after the placement of orthodontic appliances.15 The results indicated that there was no significant difference between the group treated with laser and the group treated with LED in regard to the levels of pain analyzed through the VAS. Traviesas Herrera et al.16 assessed the reduction of chronic edematous and fibro-edematous gingivitis in a group treated with helium-neon laser compared to another group treated with chlorhexidine. Their results showed a significant decrease in chronic edematous and fibro-edematous gingivitis in both groups, but with a higher percentage in those treated with laser. In a similar study conducted on 58 patients between 12 and 35 years, the effectiveness of helium-neon laser in the treatment of chronic gingivitis was compared with the conventional treatment of 0.2% chlorhexidine. It was found that the reduction of gingivitis was more successful in patients treated with laser therapy, without detecting adverse effects associated with radiation.17 There is a report in Brazil on the study of the process of bone and soft tissue repair occurred in a patient who had two extraction wounds; a wound was taken as control and on the other, laser therapy was applied at 1, 4, 8, 15 and 23 days after tooth extraction.18 There was a more rapid recovery of the tissues and lower levels of pain according to the Visual Analog Scale as given by the patient. This was attributed to the fact that laser therapy produces cell acceleration, especially in fibroblasts and epithelial and endothelial cells.
There are therapeutic applications of low-level laser focused on various effects, for example, in the values of enamel adhesion of metallic and ceramic brackets, when curing resin using laser light; or in microfiltration and sealing subsequent to laser application.19–24 There are also reports that indicate benefic results at clinical and histological level in the dental pulp of rats and humans when low-level laser is applied during tooth movements in orthodontic treatment; there even are reports that conclude that there is a reduction in treatment time.25–27
In the present investigation, the radiographic characterization of the thickness of the periodontal ligament (tPDL) and pain perception (PP) is assessed at the start of orthodontic treatment, activating and applying infrared laser of 810 nm each month for three months, in order to establish whether there are significant differences in tPDL and PP in groups of patients with and without treatment with laser light. In addition, in order to improve the quality of Service of the Orthodontics and Orthopedics Clinic of the Faculty of Dentistry of the University of Sinaloa (FOUAS) and aiming to reduce the discomfort and pathological reactions that orthodontic treatment involves during the first phase of dental movement, it was also intended in this study to provide detailed information on the methodology and parameters related to laser treatment.
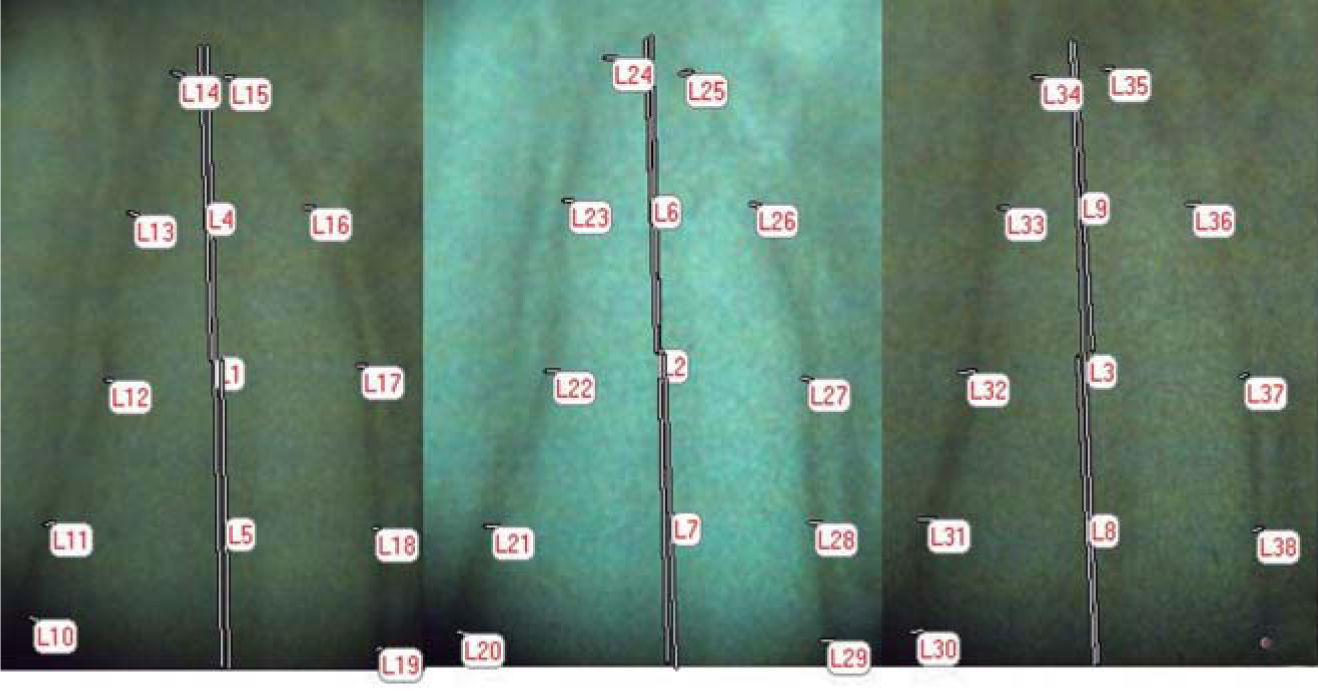
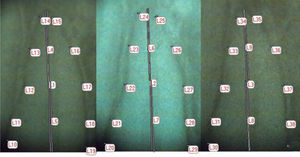
MATERIAL AND METHODSThe research was quasi-experimental and conducted in the city of Culiacán, Sinaloa. Sample description: it was a non-probabilistic sample constituted by patients who came to the Clinic of Orthodontics and Orthopedics of the FOUAS, from March to October of the same year, who agreed to participate and submit to laser therapy. The sample consisted of 200 measurements in teeth #1.1, 1.2 (with laser treatment, Quantum® GO810 emission of laser light) and teeth #2.1 and 2.2 (with usual management) of 10 patients. 10 measurements were performed on each tooth to which metal brackets were bonded. Periapical X-rays were taken to measure the thickness of the periodontal ligament (Figure 1). The measurements were performed using the Motic Advance 3V software. 810 nm Quantum laser was applied with an intensity set to 25 Hz, 100 mW, 8 J, 160 s with the scanning technique for the first three months of treatment. The measurements were obtained before and after orthodontic activation on each patient. In terms of pain, the visual analog scale (VAS)28 was applied on each side (left-control and right-laser application). Once the results from 1 to 10 were collected, the SPSS v-19 statistical software was used for descriptive statistics: frequencies, adjusted estimated means and percentages for the quantitative variables; the difference in means had a confidence interval of 95%. For the difference in the adjustment for multiple comparisons a significance level of 0.05 was contemplated.
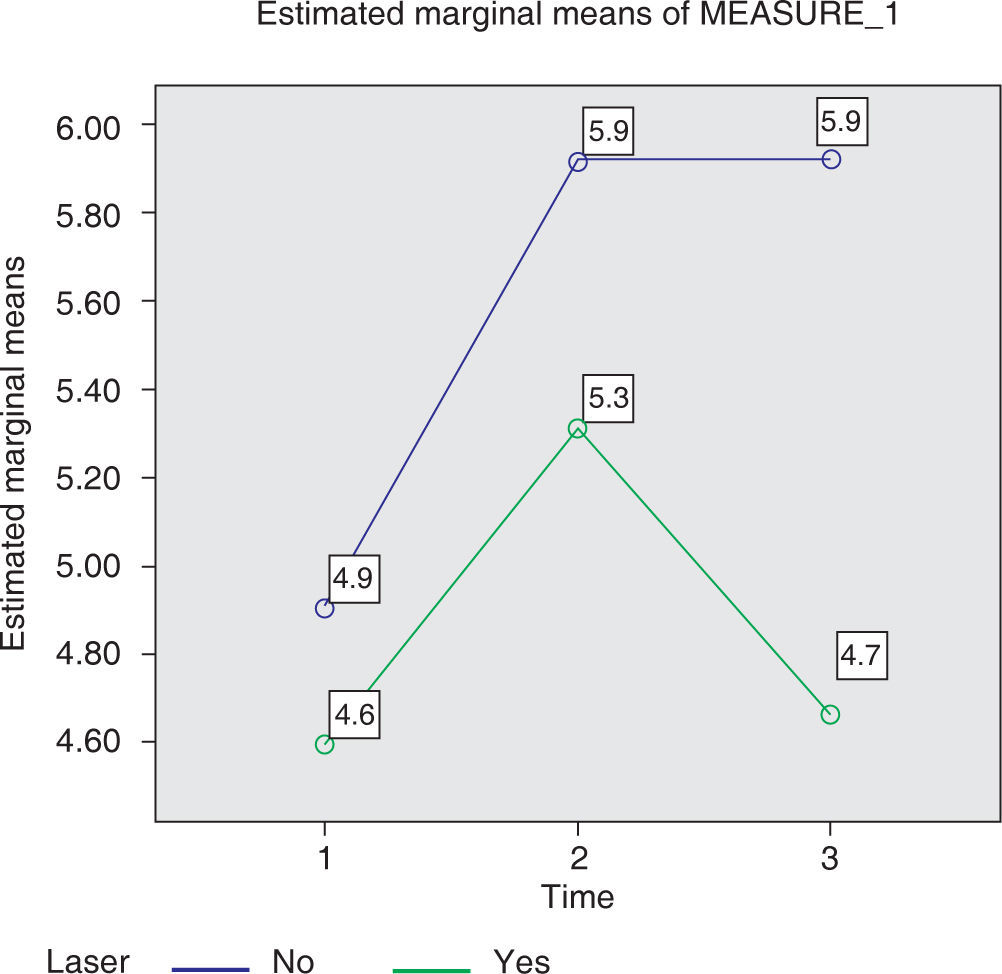
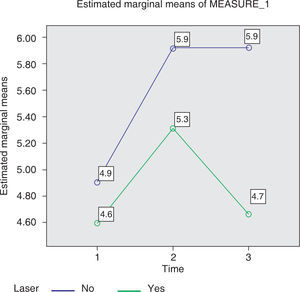
RESULTSPDL thicknessThe age of the patients was between 12 and 39 years (12, 13, 15, x 18, 19, 26, 39). The means of the measurements of the periodontal ligament around the roots at the beginning of orthodontic treatment, at one month and two months after the application or non-application of laser were: upon application 4.6 ± 1.4 μm, while for controls, it was 4.9 ± 1.2 μm. The average number of applications after the first month was 5.3 ± 1.7 um and in the control group, it was 5.9 ± 10.7 μm. After the second month, it was 4.7 ± 1.3 μm; and in controls, 5.9 ± 1.3 μm.
emspFigure 2 shows the measured changes upon laser application around the roots, during orthodontic treatment from the onset of treatment; at one month and at two months after activation of the appliances. It is shown how from the beginning, there is a possible inflammation reaction but it decreases a little, on average (0.6%) by applying laser; while during the second month, continuing with treatment, there is a more noticeable difference (1.2%).
Means obtained by measuring the periodontal ligament, at the beginning of orthodontic treatment and during first and second month of treatment in the control group and when applying laser (the results are listed before applying the ten factor to make the conversion that the measuring instrument of the microscope marks).
A total of 40 measurements taken from 10 patients were performed under the following design: prior to the activation of orthodontic appliances, each patient was given a visual analog scale (VAS) of the pain. The left side constituted the control group (with label of «No» treatment), and the right side formed the group with laser application (with label of «Yes» treatment). Outcomes were sought with values from 1 to 10, which are shown in figure 3.
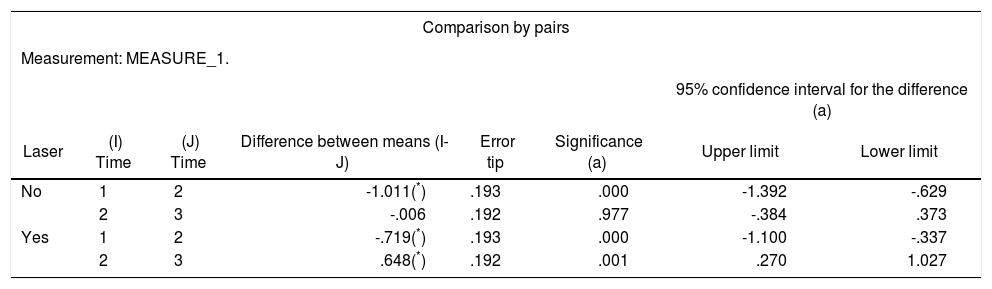
Table I shows the comparison by pairs of the measured results of the teeth in which laser was applied and those teeth that acted as a control. The results correspond to the measured times, from onset of treatment to the first month; and from the second to the third month; to show significance, with a confidence interval of 95%. The difference was not significant (p = 0.977) in the group without laser, from the second to the third month.
Estimated marginal means for the group without laser application («No» group) and the group that received treatment with laser («Yes» group) at two time intervals.
| Comparison by pairs | |||||||
|---|---|---|---|---|---|---|---|
| Measurement: MEASURE_1. | |||||||
| 95% confidence interval for the difference (a) | |||||||
| Laser | (I) Time | (J) Time | Difference between means (I-J) | Error tip | Significance (a) | Upper limit | Lower limit |
| No | 1 | 2 | -1.011(*) | .193 | .000 | -1.392 | -.629 |
| 2 | 3 | -.006 | .192 | .977 | -.384 | .373 | |
| Yes | 1 | 2 | -.719(*) | .193 | .000 | -1.100 | -.337 |
| 2 | 3 | .648(*) | .192 | .001 | .270 | 1.027 | |
Based on estimated marginal means.
The results found in this study show an apparent lower level of pain using the VAS scale, in the group that received laser treatment compared to the control group. However, statistically, no significant differences were found, hence it is considered desirable to perform a larger number of observations. The abovementioned results agree with the studies carried out by Lim et al.;1 while Xiaoting,9 Tortamano et al.,11 Turhani et al.,12 as well as Fujiyama et al.,13 did find significant differences in pain levels of orthodontic patients after the application of laser therapy. Holmberg et al.14 concluded that laser therapy might reduce the pain caused by the orthodontic treatment, but did not obtain significant results so they suggested to increase the number of cases studied, just as in this paper. Lacerda15 also reports that there are no significant Estedifferencesdocumentoin estheelaboradolevels ofporpainMedigraphicbetween the laser-treated group and the control group. The results of the present study are consistent with those from the Traviesas et al.16 and González et al.,7 which report that there is a decrease in the inflammation of gingival tissue in laser-treated groups.
Dreke Hernández et al.17 reported satisfactory results in the treatment of chronic gingivitis with helioneon laser therapy. They also highlight the fact that there were no adverse effects associated with the use of this technique; this agrees with our results on the largest decrease in periodontal ligament thickness in the irradiated group after the use of laser therapy during orthodontic movements. Several beneficial effects on gingival and pulpar fibers after using low-level laser have been documented by Baptista Pereira et al.,25 and Altan et al.26 their findings match our results, as well as the results referred by Doshi-Mehta & Bhad-Patil,27 who found a reduction in pain during orthodontic treatment.
Although in several studies it is shown that the performed measurements and the results are consistent with those in the present study, the data are not punctual in terms of the variables that need to be addressed (the brand of the equipment, the times that treatment is applied, the supplied energy, the frequency of the laser beam, the time spent at each point per session and the application technique, among others).
Although laser therapy decreases the possible inflammation as shown in this study, it cannot be said that the conditions in the use and application of therapeutic laser followed the same procedure. Possibly, the decrease in pain is due to a process of adaptation of the system, that is to say, the periodontal ligament heals by virtue of the fact that movements are not extreme, thanks to the time between activations.
CONCLUSIONSThe results show that the application of laser significantly decreases periodontal ligament thickness compared to a group treated in a conventional manner (control).
With regard to the scale of the pain, both in teeth that received laser therapy as well as in those in which it was not applied, the average pain at one month and at two months of treatment decreased. However, it is recommended to perform further studies varying the conditions of laser application and increasing the number of samples (patients).
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Professor of the Masters Program in Orthodontics and Orthopedics, Biomaterials Academy, Odontology Faculty, Autonomous University of Sinaloa
The present paper is the result of a Thesis of the Masters in Orthodontics and Orthopedics Program of the Odontology Faculty, Autonomous University of Sinaloa.
Student of the Masters Program in Orthodontics and Orthopedics, Biomaterials Academy, Odontology Faculty, Autonomous University of Sinaloa