Excessive mandibular growth, an underdeveloped maxilla or the combination of both may cause class III malocclusions. Treatment success in this kind of cases depends largely on the age of the patient since if not treated timely, the only alternative is a surgical-orthodontic treatment. Hereunder, the case of a 12-year-old patient, skeletal CIII with anterior crossbite treated with a facemask anchored to mini-implants is presented.
La maloclusión clase III puede ser causada por un crecimiento mandibular excesivo, un maxilar poco desarrollado o ambos. El éxito del tratamiento para este tipo de casos, depende en gran parte de la edad del paciente, ya que al no ser tratado a tiempo, la única alternativa es un tratamiento ortodóntico-quirúrgico. A continuación, se presenta el caso de un paciente de 12 años de edad CIII esquelética con mordida cruzada anterior tratado con máscara facial anclada a miniimplantes.
Maxillary protraction with use of facemask has favorable orthopedic results. Previously it was thought that it was impossible to perform a pure maxillary advancement until Delaire used the facemask in patients from an early age. Prior to this, only upper incisor proclination was accomplished as a result. Today, it is established that it is possible to obtain a maxillary advancement with the use of the facemask in patients aged 8 years or younger.1 The age limit to obtain favorable outcomes is 10 years.2
In older patients the result is almost null, obtaining only tooth movement and a rotation down and rearward of the mandible that may cause an increase in the vertical dimension. Hyperdivergency may also be increased if the dental anchorage causes undesirable movements such as extrusion. The use of mini-implants as a basis for anchorage with the facemask could favor achieving an orthopedic movement of the maxilla in patients with permanent dentition.
CASE REPORTMale patient of 12 years and nine months of age attended the orthodontics clinic with the following reason for consultation: «my upper teeth are inward and my lower teeth are outward». The medical history showed no apparent pathological data. Upon the facial examination, the patient presented a convex profile, with an increased lower third, positive smile as well as coincident dental and facial midlines (Figure 1).
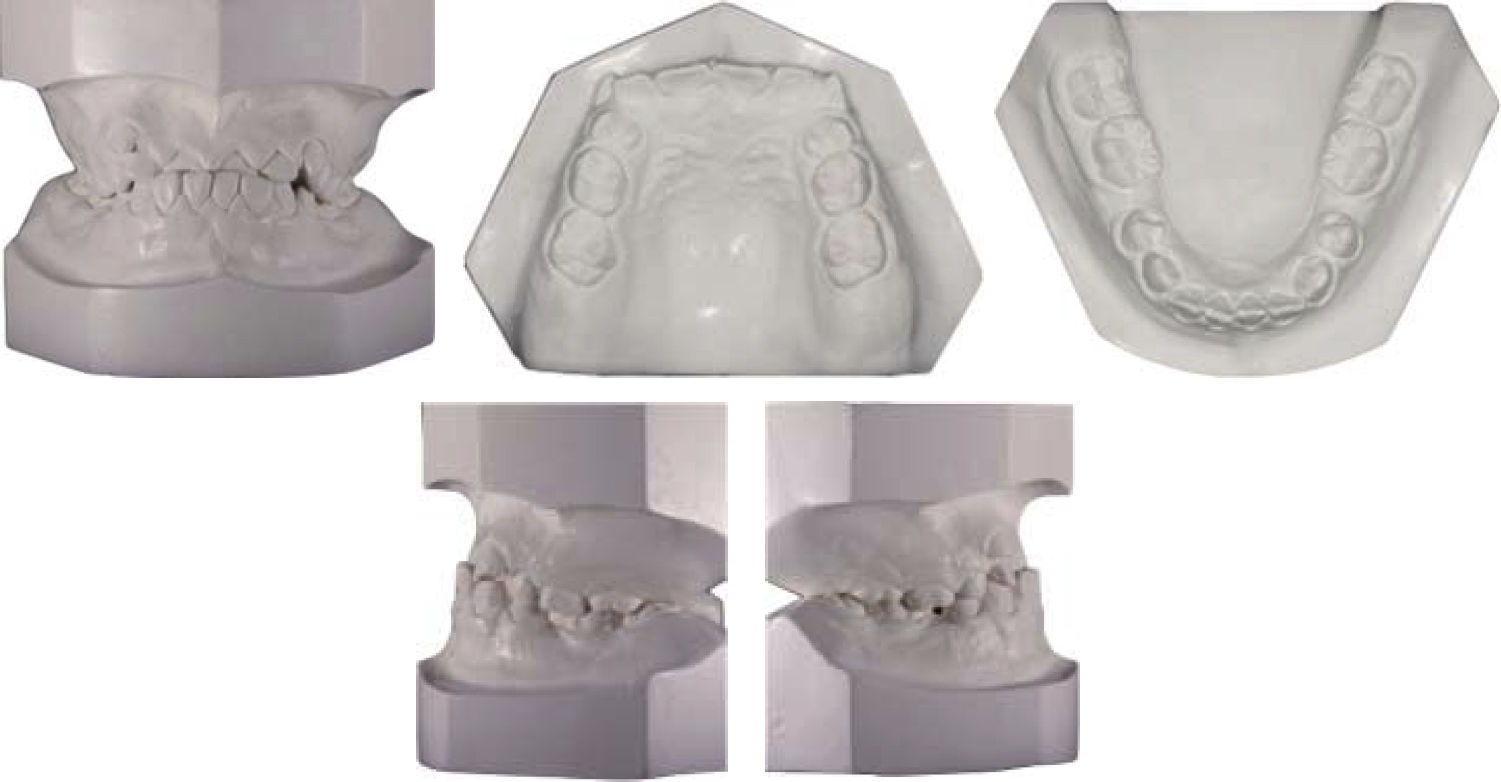
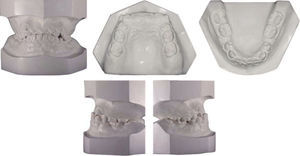
The intraoral inspection showed the upper dental arch with mixed dentition, an occlusal relationship with anterior crossbite, canines in supraoclusion, bilateral class III molar, severe crowding in the upper arch and coincident upper and lower dental midlines (Figures 2 and 3).
The panoramic radiograph shows the presence of deciduous teeth 5.5 and 6.5, retained upper second premolars and erupting lower second premolars. Dental germs from teeth 1.8, 2.8, 3.8 and 4.8 were also observed, as well as a: 2:1 crown-root ratio in a generalized form as well as a homogeneous trabecular bone (Figure 4).
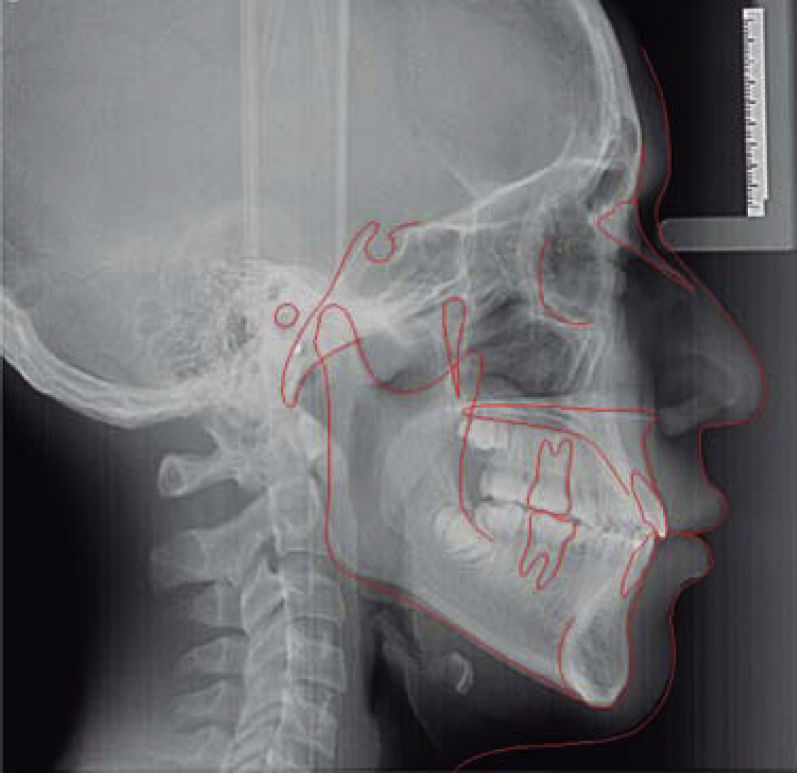
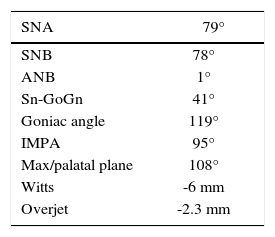
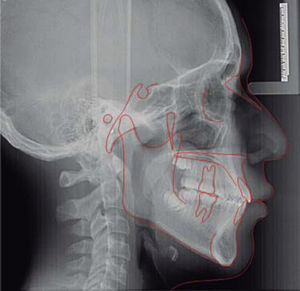
The cephalometric analysis performed in the lateral headfilm showed a skeletal CIII patient due to maxillary retrusion, anterior crossbite with negative overjet, upper incisor retroclination and a relative protrusion of the lower incisor. Vertically the patient had a dolichofacial pattern (Figure 5andTable I).
The main objective was the correction of the skeletal CIII using a facemask anchored to mini-implants to achieve a pure maxillary orthopedic advancement and correct the crossbite considering the possibility that the patient may still have remaining mandibular growth. Dental objectives were: to correct incisor inclination, improve the profile, maintain stability and condylar health as well as to achieve bilateral molar and canine class I, eliminate crowding and obtain a functional occlusion.
Treatment alternativesA possibility of treatment was decompensation of dental inclinations through orthodontic treatment to subsequently perform a surgical treatment once growth had completed. Within the disadvantages of this treatment alternative were the surgical risk, a considerable increase in costs as well as the fact that the patient would have to face a long waiting time, probably six years, for surgery.
Another option was the extraction of first premolars and the retraction of the anterior segment with skeletal anchorage. However, if there was any remnant of growth the degree of dental inclination of the lower incisors could be compromised biologically. This would mean that it might be necessary to decompensate again the incisor inclinations for subsequently performing a surgical approach.
Finally, the treatment selected for this case was to use a face mask with skeletal anchorage through the use of mini-implants, remove upper and lower second premolars, advance orthopedically the maxilla in a horizontal sense, to compensate for the possible remnant growth of the mandible and dental compensation to correct the anterior crossbite.
Treatment progressTwo 8mm implants were placed in the center of the palate and an impression was obtained for fabricating an acrylic plate (Figure 6). Subsequently, the acrylic plate was cemented and the facemask with 16 oz extraoral elastics was placed. Treatment continued with the placement of 4 x 2 0.022 MBT appliances and leveling was begun with a 0.016 NiTi archwire. Four months later, lower appliances were placed and the use of the facemask was continued with the placement of 4 x 2 0.022 MBT appliances and leveling was begun with a 0.016 NiTi archwire. Four months later, lower appliances were placed and the use of the facemask was continued.
Extractions of the deciduous second molars and enucleation of the second upper premolars was performed. So brackets were placed in the remaining teeth and bands in second molars for leveling. After 17 months of facemask use the acrylic plate was removed as well as the screws. 0.019 x 0.025 stainless steel archwires were placed to continue with the closure of the remaining spaces in addition to the use of CIII elastics. A panoramic radiograph was taken as well as impressions for bracket repositioning and tipping correction. The arches were consolidated and the bite settled. A lower fixed retainer was placed as well as a circumferential plate with screen in upper arch (Figure 7).
The treatment lasted for two years and six months. At the end, surgical extraction of third molars was exhorted. (Figure 8)
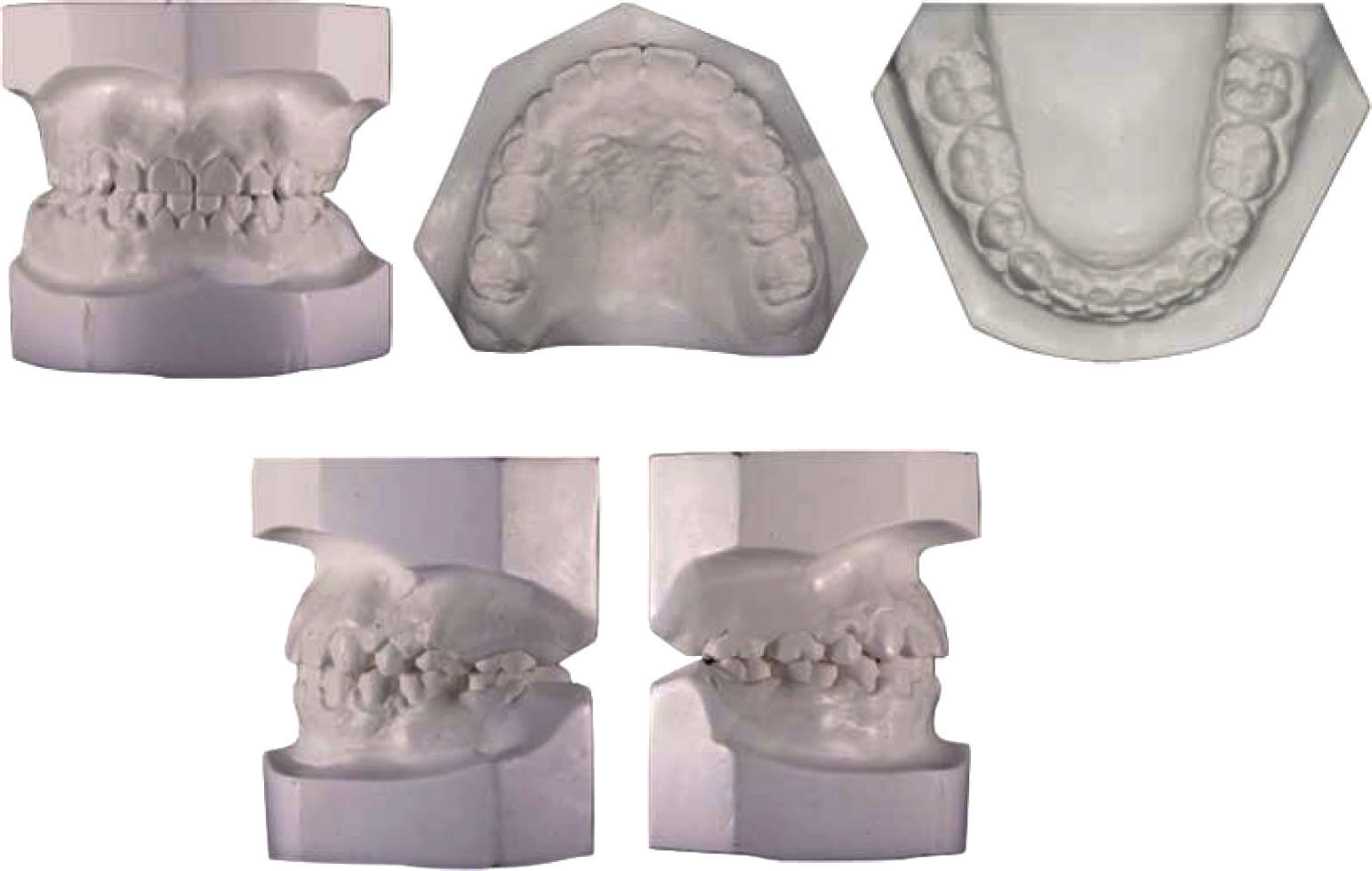
RESULTSBoth the dental and skeletal objectives were met despite the late age of the patient. The facial results were favorable with an improved labial support and nasolabial angle (Figure 9). Proper occlusion was achieved by obtaining bilateral molar and canine class I, posterior settling and centered dental midlines. As a result of correcting the anterior crossbite through an anterior projection of the maxilla (Figure 10) a positive overjet and overbite was obtained as well. The final panoramic x-ray shows root parallelism (Figure 8).
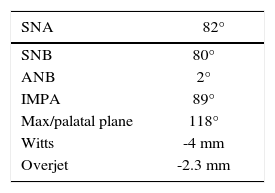
To correct the anterior crossbite a number of dental and skeletal changes took place. The first was to change the lower incisor inclination, which was 98 degrees to a near-optimal retroclination of 89 degrees. At the same time, the upper incisor that had an inclination with respect to the palatal plane of 108 degrees was proclined to 118 degrees. From having a -2.3mm overjet, a final overjet of 2.3cm was obtained at the end. A maxillary advancement was achieved: initially the patient had a SNA of 79 degrees and it was changed to 82 degrees. There was also a modification of the Witts: -6 to -4mm, which allowed compensation for a significant remnant growth of the mandible (Figure 11andTable II).
DISCUSSIONWhen diagnosing a class III malocclusion the age of the patient is extremely important because the type of treatment will depend on the expected growth that may occur. By performing the diagnosis at the optimum moment-during the final phase of the primary dentition or in early mixed dentition-treatment may include a facemask, chin cup or functional appliances. This intervention will increase treatment time, but it may also make it easier to obtain the desired results.3
In the case hereby presented, the patient was in a semi-late stage since his skeletal development had almost concluded. For this reason, we had to opt for a combination of various ways of dealing with the malocclusion.
The facemask therapy produces one or more of the following effects: correction of the discrepancy between centric relation and centric occlusion, maxillary protraction, anterior movement of upper teeth and lingual inclination of the lower incisors. The effects of this procedure have a greater impact on patients from an early age. However, they must be monitored throughout their growth.4
According to Ghiz AM et al, after six to nine months of use of the facial mask, a complete correction of the overjet is achieved. But 25 percent of these patients tend to present a decrease with the passing of the years. The excess of mandibular growth produced a negative result and they noted that these patients had not been dentally compensated.5 In our case, the use of the facemask anchored with orthopedic implants allowed the correction of the maxilla and to overcompensate the remnant mandibular growth that, in addition to the dental compensation produced a favorable outcome.
Anchorage in orthodontics has evolutioned from transpalatal arches, extraoral anchorage, lingual arches, Nance button among others. Many of these appliances require patient cooperation and do not prevent dental movement completely. In order to not having to continue to rely on the collaboration of the child, different devices and techniques have been introduced. An alternative is skeletal anchorage such as conventional dental implants, special intraoral implants, on plants, wires in the zygoma, intentionally anchylosed teeth and mini-implants.6
In this particular case we opted for the use of mini-implants. These may be placed temporarily in the maxilla and the mandible as a stationary anchorage.7 In recent years, titanium implants have been used for orthodontic treatment mainly, to provide an anchorage without the need for patient cooperation as these allow immediate loading due to the fact that Osseo integration is not a prerequisite and the cost is lower than conventional implants. In addition, classic problems related to the correction of a collapsed or retrusive maxilla may be solved and they help to reduce the unwanted movement of the teeth that are used as anchorage-molar tipping, which increases the risk of traumatic occlusion.8,9 By using skeletal anchorage in this case, a vertical growth control was achieved.
Recently Clerck and Proffit, reported several attempts to change the skeletal proportions during growth and that favorable results in these would avoid dental compensation. They established that a few millimeters changes have been possible in growing class III patients using mini-plates and elastics.10 The mini-plates were placed in the region of the infrazygomatic crest in the maxilla and the canine region in the mandible. The success of the same is related in large part with the surgical process and the thickness and quality of the bone. In young patients this bone may still be deficient and does not create an ideal mechanical retention. In addition to that the use of these plaques can be more expensive. So in this case, it was decided to place mini-implants on the palate and perform the traction from this location. The palate in its medial and paramedical portion is probably the most ideal placement site for a variety of reasons: it is easy to access, there is little risk of damage to anatomical structures, and is lined by keratinized gingiva. Therefore, it is less susceptible to inflammation. The medial area of the palate contains a good cortical bone, which contributes to the retention of the mini-implants.11,12
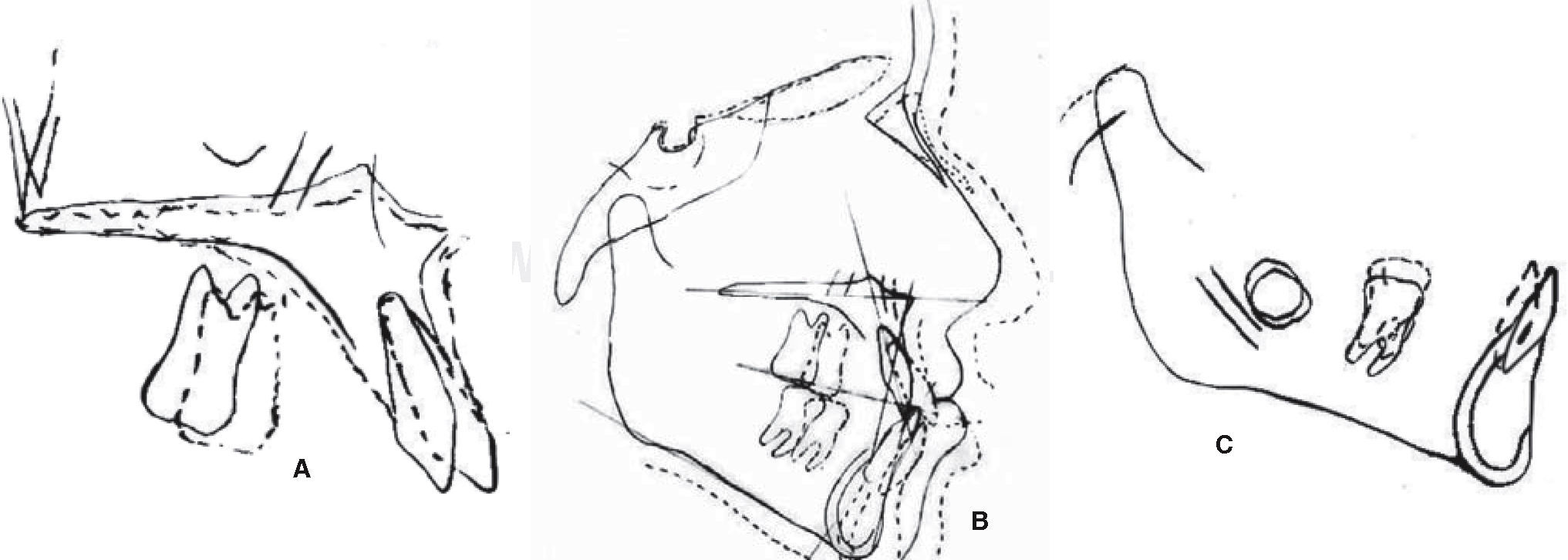
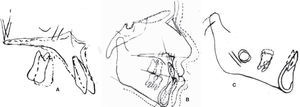
Tracing was performed using the superimposition technique of Bjork, Buschang and Nielsen (ABO).13–16 It may be observed that there was an orthopedic modification by obtaining a pure maxillary advancement of 2mm (Figure 12A). Also, a 7mm mandibular growth may be noted (Figures 12B and 12C). There was a dental modification as well: a 5 mm mesialization of the upper first molar to the extraction site of the second premolar. If we observe figure 12A, we may see that the horizontal movement that occurred was only 1mm, thus maintaining the vertical dimension of the patient. In this case, it was not desirable any extrusion movement since the patient had a hyperdivergent growth pattern. By using a skeletal fixation instead of a dental one, predictable forces and vectors were caused thus preventing unwanted movements.
It may be observed that, in addition to the skeletal changes and the ones in dental positions, there was also a dental compensation in both the upper and lower incisors. The upper incisor was proclined to 118 degrees with respect to the palatal plate and the lower incisor was retroclined to 89 degrees with respect to the base of the mandible, leaving it with an ideal inclination (Figure 11andTable II).
CONCLUSIONSIn view of the results obtained in this particular case, we may conclude that when treating a patient we should not confine ourselves to combine different therapeutic options. Probably a simple dental compensation would not be sufficient to leave the patient in optimal conditions. Neither a pure orthopedic treatment would have been enough given the age of the patient and the already present dental conditions. By adding the orthopedic modification, the use of absolute anchorage and the change in the incisor inclinations, very satisfactory dental, facial and skeletal conditions were obtained. These include class I molar and canine relationship, a good occlusion and an improvement in the soft tissues and profile.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia