The extraction of first permanent molars is a viable option for the treatment of mild to moderate discrepancies of the maxillary structures in patients with open bite. The therapeutic goal is to correct the malocclusion while trying to camouflage the skeletal problem. A case report is presented of a patient who was treated with extractions of first permanent molar in order to correct the moderate skeletal open bite through mandibular rotation thus achieving a functional occlusion and favorable cosmetic results. The aim of this report is to show that after proper case selection and a good diagnosis, first molar extractions are a suitable alternative treatment for skeletal open bites.
La extracción de primeros molares permanentes es una alternativa viable para el tratamiento de discrepancias leves o moderadas de las estructuras maxilares en pacientes con mordida abierta; el objetivo terapéutico es corregir la maloclusión al tiempo que se intenta disimular el problema esquelético. Se presenta caso clínico de una paciente tratada con extracciones de primeros molares permanentes, para corrección de mordida abierta esquelética moderada, logrando rotación mandibular, una oclusión funcional y resultados estéticos favorables. El objetivo de este artículo es demostrar que después de una adecuada selección del caso, por medio de un buen diagnóstico, las extracciones de primeros molares resultan una buena alternativa de tratamiento en el caso de mordidas abiertas de origen esqueletal.
Canut defined open bite as the obvious lack of contact between the upper and lower teeth of dental or skeletal origin; the latter, due to its multifactorial etiology and consequences represents a great challenge for the orthodontist because despite the fact that extensive research has been conducted on this anomaly, there is fear in the etiology identification and in the proper treatment selection that delivers stable functional and aesthetic results.
Currently the orthodontist has a number of treatment options and/or mechanics to treat this anomaly: extra-oral appliances, bite block, intraoral anchorage appliances, mini-implants, orthognathic surgery and bicuspid or first molar extractions.
Orthodontic treatments where extractions of first permanent molars have been suggested are often considered as difficult to handle, with extended treatment time, reserved prognosis and where the final result may be affected. However there are several case reports in the literature of patients with open bites treated by means of first molar extractions. Arvystas in 1977 reported one of the first cases, followed by Vaden in 1988, and Aras in 2002, among others. These cases were treated under the principle that by eliminating posterior contact points (possible fulcrums) and moving the posterior segment mesially, a mandibular anterior rotation would occur, thus closing the anterior open bite. However, for this treatment alternative to be successful with stable functional results, it is necessary to do a proper case selection.
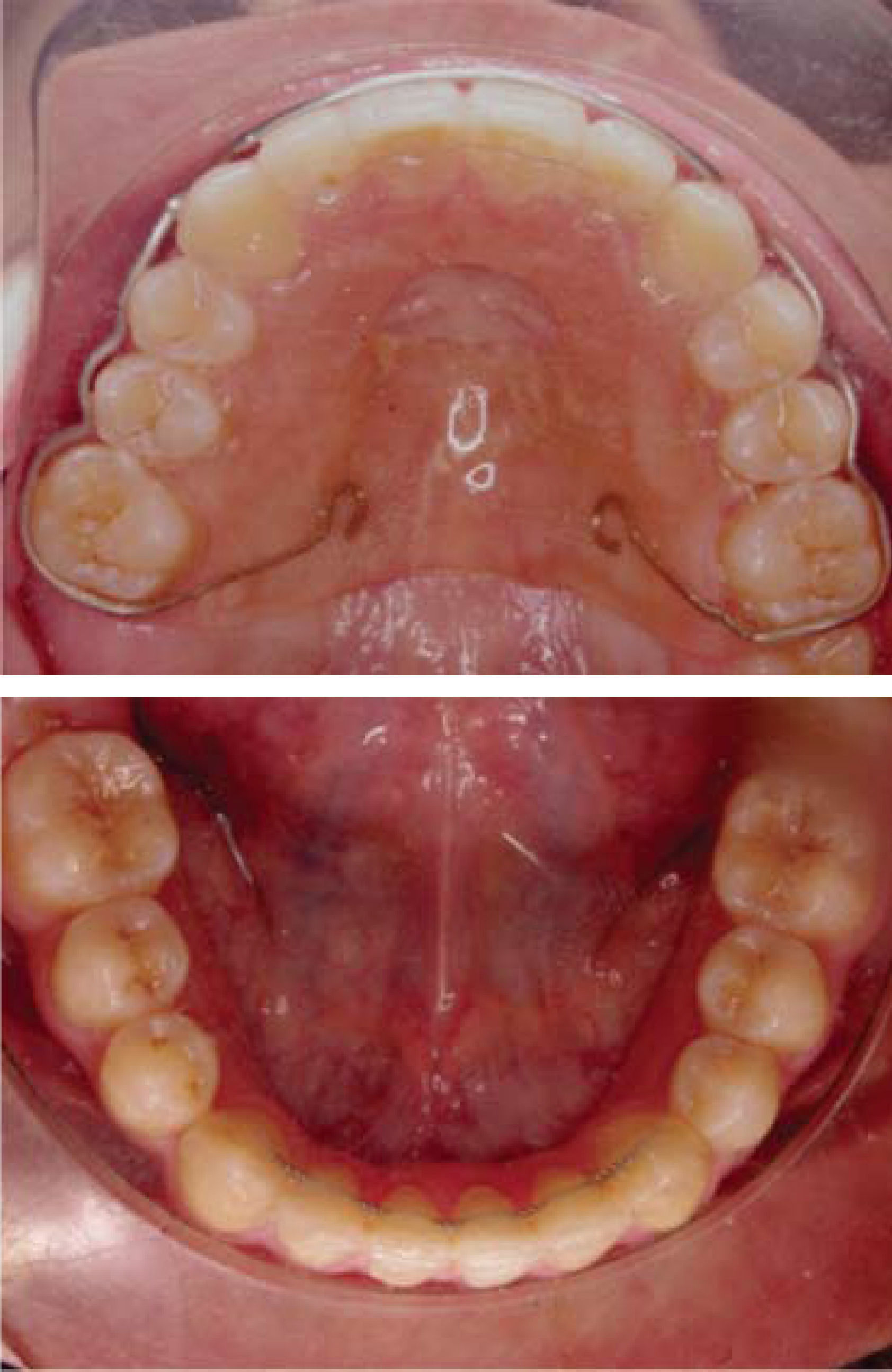
CASE REPORTDiagnosisFemale patient of 18 years 8 months of age with good overall health attends the Orthodontics Clinic at the Autonomous University of Baja California, mexicali Campus, to seek orthodontic care. On her facial analysis, a slight asymmetry, a convex profile and a retrusivechin were observed (Figure 1). On the intraoral analysis (Figure 2) an ovoid-shaped upper arch, gingival recession of the upper left lateral incisor and clinical absence of the upper left canine, a square-shaped lower dental arch with mild crowding, a -1mm overbite, bilateral molar class II, a bilateral non-assessable canine class, a 5mm overjet and a 0.5mm to the left dental midline deviation were observed.
On the functional temporomandibular joint assessment, a healthy TMJ without any apparent pathological data was noted.
Cephalometrically, a skeletal class II with mandibular rotation may be observed, with a 3° ANB angle, neutral growth, dolichofacial pattern, a 3mm interlabial distance (GAP), incisor protrusion and proclination of the upper and lower incisors and an anterior open bite (Figure 3).
On the panoramic radiograph (Figure 4) a good bone height was observed as well as a good root length and the presence of the upper left canine and upper and lower third molars.
Once the diagnosis was established and prior to the beginning of treatment, a diagnostic setup was (Figure 5) performed in order to determine whether or not by extracting the first molars, the posterior interferences would be eliminated and the anterior open bite would close.
Treatment progressA multidisciplinary treatment was performed involving orthodontics and periodontics; upper and lower molar extractions were performed.0.022” slot Roth appliances were placed with a 0.014”Nitinol archwire in both dental arches. Additionally, a transpalatalbar with a low button and a lingual arch were fitted to the second molars in order to begin the alignment and leveling (Figure 6). Upon completion of this phase an 0.017”x 0.025”stainless steel archwire was placed and the patient was referred to the Periodontics Department for the correction of the gingival recession on the upper left lateral incisor. Space closure was then initiated with 0.019”x 0.025”stainless steel double keyhole loops archwires (Figure 7) and after 6 months space closure was achieve don the upper arch. An 0.019”x 0.025”archwire with a mesialization loop was placed for the lower second molars during approximately three months (Figure 8). However it was necessary to place a mini implant as an auxiliary in the space closure of the lower right second molar. Once space closure was completed, a 0.021”x 0.025”Braided archwire was placed on the lower arch and on the upper, a 0.021”x 0.025”upper rigid archwire (Figure 9). Occlusal settlement adjustments were conducted and after 30 months the appliances were removed (Figure 10). It was decided to monitor the eruption of the third molars and continue performing occlusal adjustment so to avoid undesirable contacts.
RESULTSAfter 30 months of treatment, the facial axis increased 1°, the mandibular axis decreased 1° and the interincisal angle went from 119° to 137° (Figures 11 and 12). The profile was improved with a good chin projection (Figure 13). Bilateral molar and canine class I, a 2mm overjet and overbite and good functional guides were obtained. Additionally, root parallelism was achieved and we continued to monitor the eruption of the upper third molar (Figure 14). Occlusal adjustments will be conducted until they finish their eruption.
RETENTIONA circumferential removable retainer was placed on the upper arch and in the lower, a fixed retainer from canine to canine (Figure 15).
DISCUSSIONOrthodontic treatment with first molar extractions is a therapeutic option that nowadays causes controversy due to the fact that these teeth are considered fundamental keys to the occlusion. However, in the papers by Arvystas in 1977, Vaden in 1988, Sulaiman in 2001 and Aras in 2002 among other authors it has been stated that skeletal open bite treatment with first molar extractions provides functional results with more stability than those obtained in non-extraction treatments.
This treatment option will be successful only if the clinician has the clinical ability and experience to select the case properly and have good control over the biomechanics. It is important to consider that according to Seddon (2004) treatments with first molar extractions may last 7 to 9 months more than conventional treatments.
CONCLUSIONSFirst molar extractions are a good treatment option that provides stable, functional and esthetic results for skeletal open bite cases. It is important to consider that this therapeutic alternative demands an adequate case selection and a high level of clinical expertise and skill in order not to compromise the treatment results and expectations.
Clinical consultant.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia.