Relapse is an unavoidable challenge for the specialist; in orthodontic practice several recommendations have been stated to prevent it: maintain the original arch form, particularly the lower; do not modify inter-canine width, do not modify the bucco-lingual incisor inclination, achieve a good intercuspation, perform circumferential supracrestal fiberotomy and overcorrect rotated teeth. A case report is hereby presented. The patient was 25-year-old and had had a previous orthodontic treatment with four first premolar extractions. He presented moderate upper and lower crowding, gingivitis, no temporomandibular joint symptoms, and dental anatomy abnormalities in teeth 3.4 and 4.4.
ObjectivesPreparation for referral to restorative dentistry, obtain a normal overbite and overjet, maintain arch form, match dental midlines, achieve good intercuspation, root parallelism and improve periodontal health.
MethodsNon-extraction case treated with fixed appliances: InOvation® 0.022” x 0.028” Roth Thermo-activated Palatal Expander® to obtain space on the upper arch.
ResultsAll the objectives were achieved despite the dental anatomy abnormalities, except for root parallelism due to anomalies in root form.
ConclusionsThe case was treated following the established orthodontic recommendations to prevent a second episode of relapse and at the same time obtain a good prognosis for referral to restorative dentistry.
La recidiva es un escenario ineludible para el especialista; en la práctica ortodóncica varias recomendaciones han sido establecidas para prevenirla, mencionando entre éstas: mantener la forma de arco original, de manera particular la forma de arco inferior, no modificar la distancia intercanina, no modificar la inclinación buco-lingual de los incisivos, obtener un buen engranaje oclusal, realizar fibrotomía circunferencial supracrestal y sobrecorregir dientes rotados. El presente caso clínico corresponde al de una paciente de 25 años de edad, tratamiento ortodóncico previo con extracción de cuatro primeros premolares, moderado apiñamiento superior, moderado apiñamiento inferior, gingivitis, ningún síntoma de trastorno temporomandibular y anormalidades anatómicas en órganos dentales 3.4 y 4.4.
ObjetivosPreparar el caso clínico para remisión a odontología restauradora, establecer una correcta sobremordida horizontal y vertical, no modificar la forma de arco original, coincidir líneas medias, obtener un correcto ajuste oclusal, conseguir paralelismo radicular y mejorar salud periodontal.
MétodosTratamiento a realizar sin extracciones, aparatología fija Roth In-Ovation® 0.022” x 0.028”, uso de expansor Palatino Termo Activado® para obtención de espacio en la arcada superior.
ResultadosTodos los objetivos fueron conseguidos a pesar de las anormalidades anatómicas dentales, salvo el paralelismo radicular en todas las piezas por anormalidades de forma también en la porción radicular.
ConclusionesEl caso clínico se llevó de acuerdo con las recomendaciones ortodóncicas para evitar un segundo episodio de recidiva y al mismo tiempo obtener un buen pronóstico para su remisión al departamento de odontología restauradora.
Relapse in orthodontics is presented as an unavoidable scenario for the specialist.1 It is frequent to find patients who require a new treatment for presenting current signs of crowding, mainly in those cases where teeth were rotated quickly and in a considerable amount of degrees.2 It is the responsibility of the professional to base his or her practice on evidence-based recommendations to minimize the possibility of inconveniences.
Some of these recommendations are:
- •
Do not modify the original arch shape, particularly the shape of the lower jaw and intercanine distance.3–6 The initial position of the teeth has developed between the muscular strength of the tongue in its inner part and the muscular resistance that the cheeks and the orbicular muscle in the external part offer.4
- •
All dental inclination tends to be unstable so if proclination is part of the final objectives, indefinite retention must be considered.1
- •
A correct occlusal intercuspation prevents transverse relapse.6
- •
Overcorrect teeth that are severely rotated.2,7,8
- •
Perform circumferential supracrestal fiberotomy.8,9
- •
Alignment and root parallelism; must be taken into consideration in cases of incisors outside the archline with individual torque to bring the root into the basal bone and with an adequate amount of bone between neighboring roots.6
- •
Interproximal wear from canine to canine to create a contact area instead of a contact point.1,9
- •
Elimination of harmful habits.10
Long-term stability is possible with a correct diagnosis and clear objectives; however, the patient must assimilate the possibility of change that occurs with growth and development, understanding the difference between relapse and natural changes of the age.
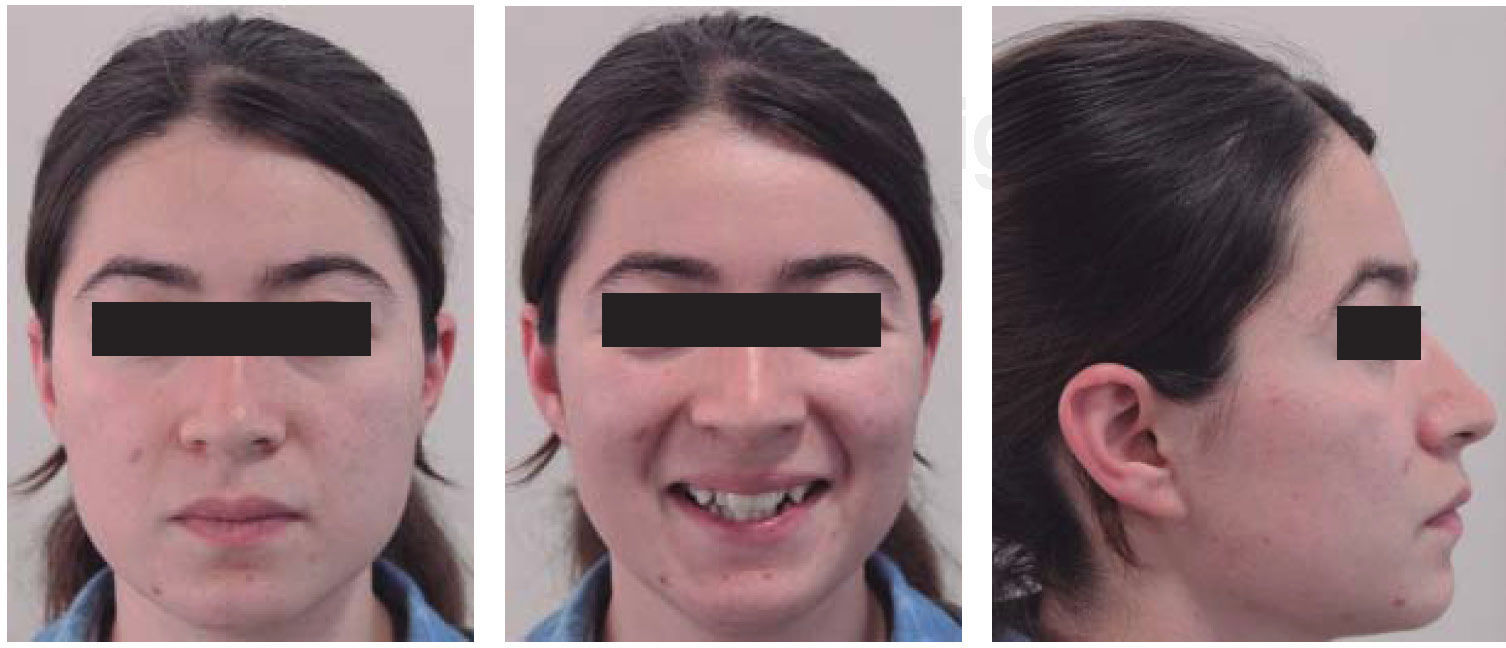
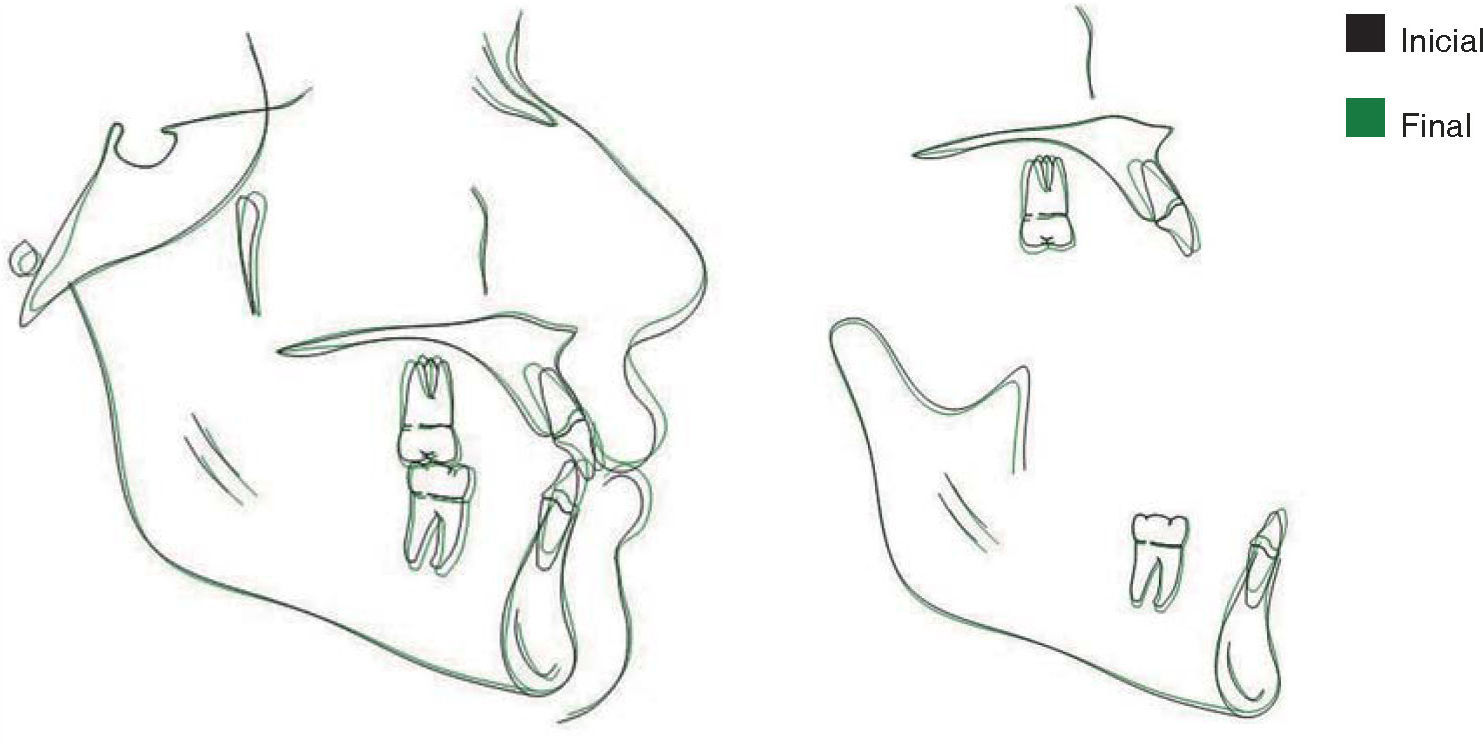
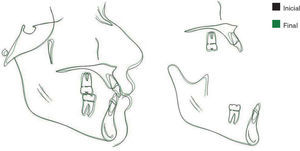
METHODSThe present article presents the case of a female patient of 25 years and 2 months of age, with a prior orthodontic treatment, in which the extraction of 4 first premolars was performed (Figure 1).
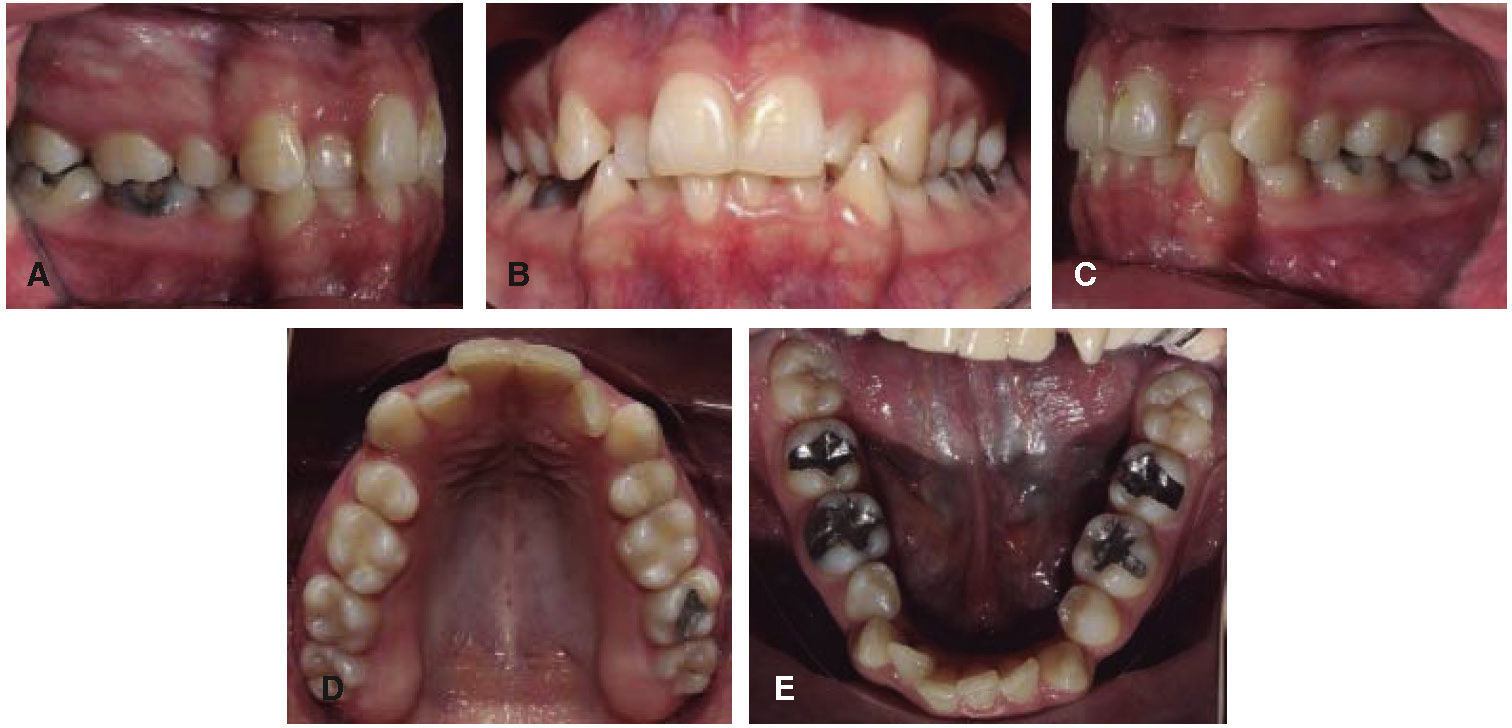
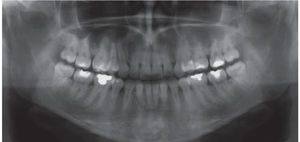
Clinical setting at the beginning of treatment: no symptoms of temporomandibular joint disorder, gingivitis associated with plaque, crossbite of upper left lateral incisor, moderate upper and lower crowding, caries between 2.5 and 2.6, no dental mobility, no endodontic treatments, anatomic abnormalities in the size and shape of second lower premolars (Figures 2A-2E).
ObjectivesPrepare the case for referral to restorative dentistry.
Establish a correct overjet and overbite.
Do not modify the original arch shape.
Match dental midlines.
Obtain a correct occlusal relationship.
Achieve root parallelism.
Improve periodontal health.
Treatment plan:Placement of In-Ovation® 0.022” x 0.028”, Roth prescription appliances.
Thermo-active Palatal Expander® for obtaining space in the upper arch (Figure 3).
Phase I:0.014” CuNiTi for a minimum of 3 months, maximum 6 months.
0.016” Nitinol, correction of dental midlines.
0.018” Nitinol assessment of leveling, alignment and molar class.
Phase II: Space closure (elastomeric chains and cinched closing archwires).0.018” S.S.
0.019” x 0.025” S.S.
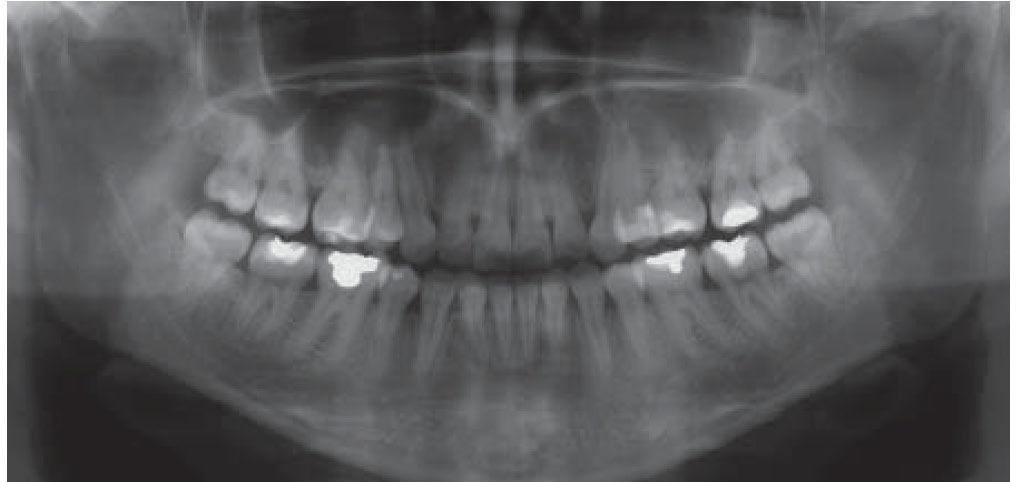
Panoramic X-ray for repositioning.
0.018” NiTi.
0.017” x 0.025” Braided S.S. (short elastics).
Phase III: Detailing and occlusal adjustment.0.019” x 0.025” Braided (short elastics).
Circumferential supracrestal fiberotomy.
RetentionFixed retainer from canine to canine in the lower arch.
Circumferential retainer on the upper arch.
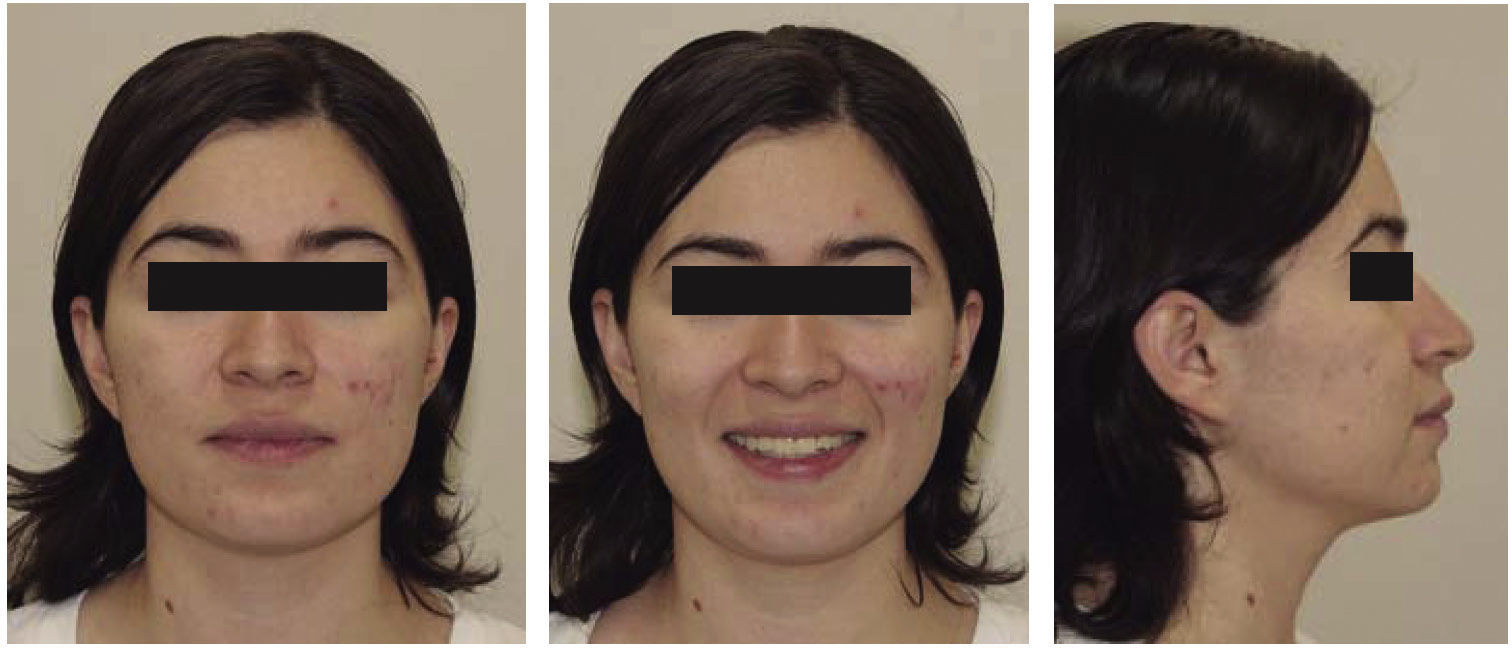
RESULTSAt the end of treatment, molar class I was obtained, as well as a canine class I; dental alignment with complete occlusal adjustment, matching dental midlines, normal overjet and overbite, good radicular parallelism except in the lower right incisor and in the upper lateral incisors.
The occlusal characteristics at the end of treatment seek to avoid a second episode of relapse while achieving an orthodontic good result, as well as a good long-term prognosis. The patient was referred to the Department of Restorative Dentistry for the final aesthetic remodeling of the patient (Figures 4 to 7).
DISCUSSIONLong-term stability may fall into controversy when trying to determine the responsibility of success; the only path to follow is evidence based dentistry. Retention has been defined by Moyers1 as «the maintenance of teeth after orthodontic treatment for a period of time necessary to maintain results» and by Riedel4 as the «maintenance in a ideal position of aesthetics and function». These definitions leave a very wide gap in common themes such as: the necessary time for teeth to acquire stability and changes inherent to growth and development. All this leads us to the understanding that living organisms are subject to a wide variability.
In the case hereby presented it was pursued to follow recommendations based on evidence: the follow recommendations based on evidence: the non-modification of the original arch shape was planned through the use of coordinated stainless steel archwires since the middle stages of treatment. Intercanine width remained unchanged by choosing the correct archwire form, although a transverse increase was noted at the level of the upper and lower molars, a fact that was in accordance with the use of the thermo-activated Palatal Expander®. The crowding could have been resolved through dental proclination but it was controlled by interproximal recontouring from canine to canine in compliance with the recommendations of Artun5 and the principles of Boese.9 The circumferential supracrestal fiberotomy was performed in the anterior teeth from canine to canine to allow the reorganization of the connective tissue fibers thus contributing to the stability of the case as has been corroborated by Edwards8 and by Boese8,9 two decades later.
The improvement in the patient's profile was not significant due to the initial retroclination and the slight proclination achieved with the appliances. The choice of a fixed retainer with rigid 0.018” wire bonded to the lower canines was manufactured in a working model to ensure close proximity and attachment to the lingual surfaces of the teeth and decrease the likelihood of activating it during bonding. Considering what was mentioned in the systematic review of Yu et al, 2013, this choice was made based more on clinical experience than on any verifiable advantage.11
CONCLUSIONSThe use of preadjusted appliances in combination with the correct choice of arch forms, a sequence that allows leveling and alignment in a progressive manner and the recommendation of circumferential supracrestal fiberotomy with interproximal recontouring, provided the fulfillment of the standards for long-term stability in patients who have had previous orthodontic treatment.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia