A large number of adult patients who need orthodontic treatment have dental absences or periodontal disease sequelae which often compromise the required anchorage. The use of mini implants greatly facilitates orthodontic biomechanics however the amount of necessary inter-radicular bone for their placement in patients with a mutilated dentition has not yet been assessed.
AimTo provide the clinician an anatomic guide that will help to locate the safer areas with more quantity of bone for inter-radicular mini-implant placement in the maxillary buccal cortical of patients with mutilated dentition.
MethodologyThe mean and standard deviation of the values at the intersection of the sagittal plane at 2, 5, 8 and 11mm from the alveolar crest with the transverse plane at 2, 5 and 8mm from the buccal cortical in images obtained from 50 maxillary cone-beam computerized tomographies (CBCTs) of periodontally compromised patients were assessed.
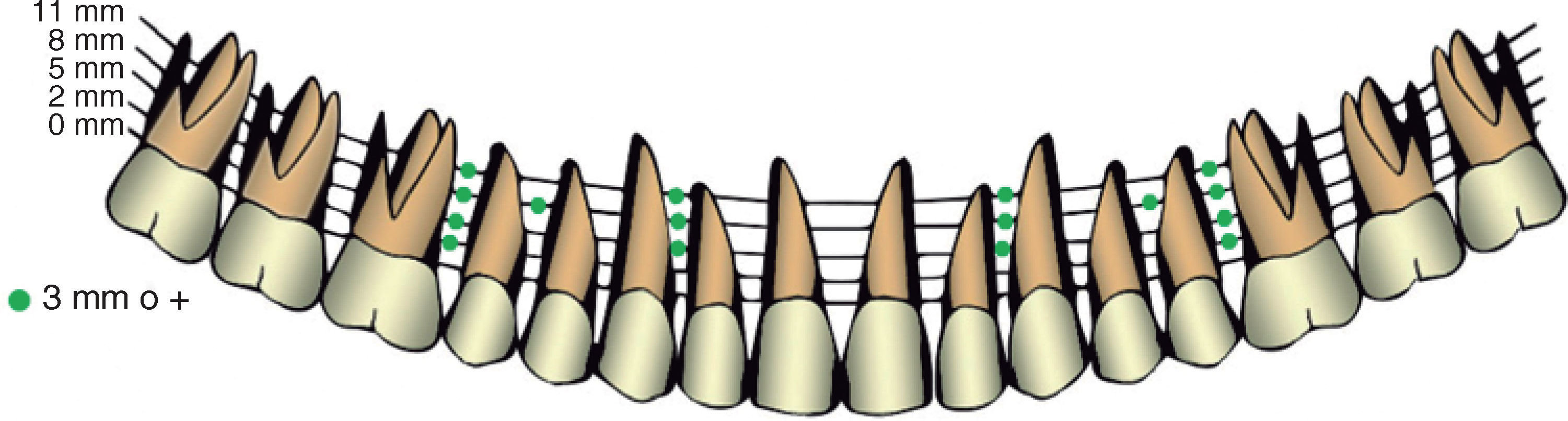
ResultsConsidering that for the insertion of a mini-implant at least 3mm of inter-radicular bone is required, the possible safe placement areas are between the second premolar and the first molar at 2, 5, 8 and 11mm from the alveolar crest, between premolars at 8mm and between canine and lateral incisor at 8 and 11mm from the alveolar crest.
ConclusionIt is recommended as a possible safe area for mini implant placement in the posterior segment between second premolar and first molar and in the anterior region, between canine and lateral incisor.
Una gran parte de los pacientes adultos que requieren ortodoncia presentan pérdidas dentales o secuelas de enfermedad periodontal comprometiendo muchas veces el anclaje requerido. El uso de mini implantes facilita considerablemente la biomecánica ortodóncica, sin embargo, la cantidad de hueso interradicular necesario para la colocación de los mismos en pacientes con dentición mutilada aún no ha sido evaluada.
ObjetivoProveer al clínico una guía anatómica que ayude a localizar las zonas más seguras y de mayor cantidad ósea para la colocación de mini implantes interradiculares en cortical vestibular en maxilares de pacientes con dentición mutilada.
MetodologíaSe determinó el promedio y la desviación estándar de los valores en la intersección del plano sagital a los 2, 5, 8 y 11mm desde la cresta alveolar, con el plano transversal a los 2, 5 y 8mm desde la cortical vestibular en imágenes obtenidas de 50 tomografías maxilares de pacientes periodontalmente comprometidos.
ResultadosConsiderando que para la colocación de mini implantes se requieren mínimo 3mm de hueso interradicular, las posibles zonas seguras para la inserción del mismo son entre segundo premolar y primer molar a los 2, 5, 8 y 11mm, entre premolares a los 8mm, entre canino y lateral a los 8 y 11mm desde la cresta alveolar.
ConclusiónSe recomienda como posible zona segura para la colocación del mini implante en posterior entre el segundo premolar y el primer molar; en anterior entre el canino y el lateral.
In recent years the use of mini implants as an alternative for absolute anchorage has become a frequently performed procedure in the clinical practice of the orthodontist. Their low cost, easy placement and removal, as well as the immediate loading are part of the reported mini-implant's benefits.1,2
It is important to consider that the age of patients who undergo orthodontic treatment has increased in recent years. Many of these patients are periodontally compromised and absolute anchorage is often required.
It has been found in previous studies that the upper maxillary alveolar cortical is significantly less compact and less thick than the mandibular cortical.3 The study conducted by Samrit et al shows that the density of the alveolar cortical has a mean value of 929.2 Hounsfield Units (HU) in the maxilla while in the mandible it has a mean value of 1116.2 HU. With respect to the density of the cancellous bone the authors report a mean value of 450.9 HU in the maxilla and 561.87 HU in the mandible.4 This pattern justifies greater anchorage loss and therefore a greater need for anchorage control devices in the maxilla.
The amount of inter-radicular bone has been assessed in CT scans by different authors whose studies were conducted in patients with minimal malocclusion or ideal occlusions but no similar studies in periodontally compromised patients have been performed.
Chaimanee et al recommend a free space of 1mm around the mini implant to preserve periodontal health, therefore, a minimum space of 3mm is considered necessary for its placement.5
The primary stability of skeletal anchorage depends on the quality and quantity of bone at insertion site. One of the most accessible sites for mini implant insertion in the maxillary alveolar process is the buccal surface.5
The aim of this study was to provide a clinical anatomical guide to help locate the safer and with more amount of bone areas for inter-radicular miniimplant placement in the buccal cortical in the maxilla of periodontally compromised patients.
MATERIAL AND METHODSFifty 0.4 mm-thickness CBCT scans were obtained from periodontally compromised patients. Linear measurements were taken to determine the amount of bone present in the inter-radicular space of the maxillary teeth.
The inclusion criteria were: patients with permanent teeth, tooth absence and radiographic signs of having suffered periodontal disease. The sample was obtained without distinction of ethnic group, gender or age.
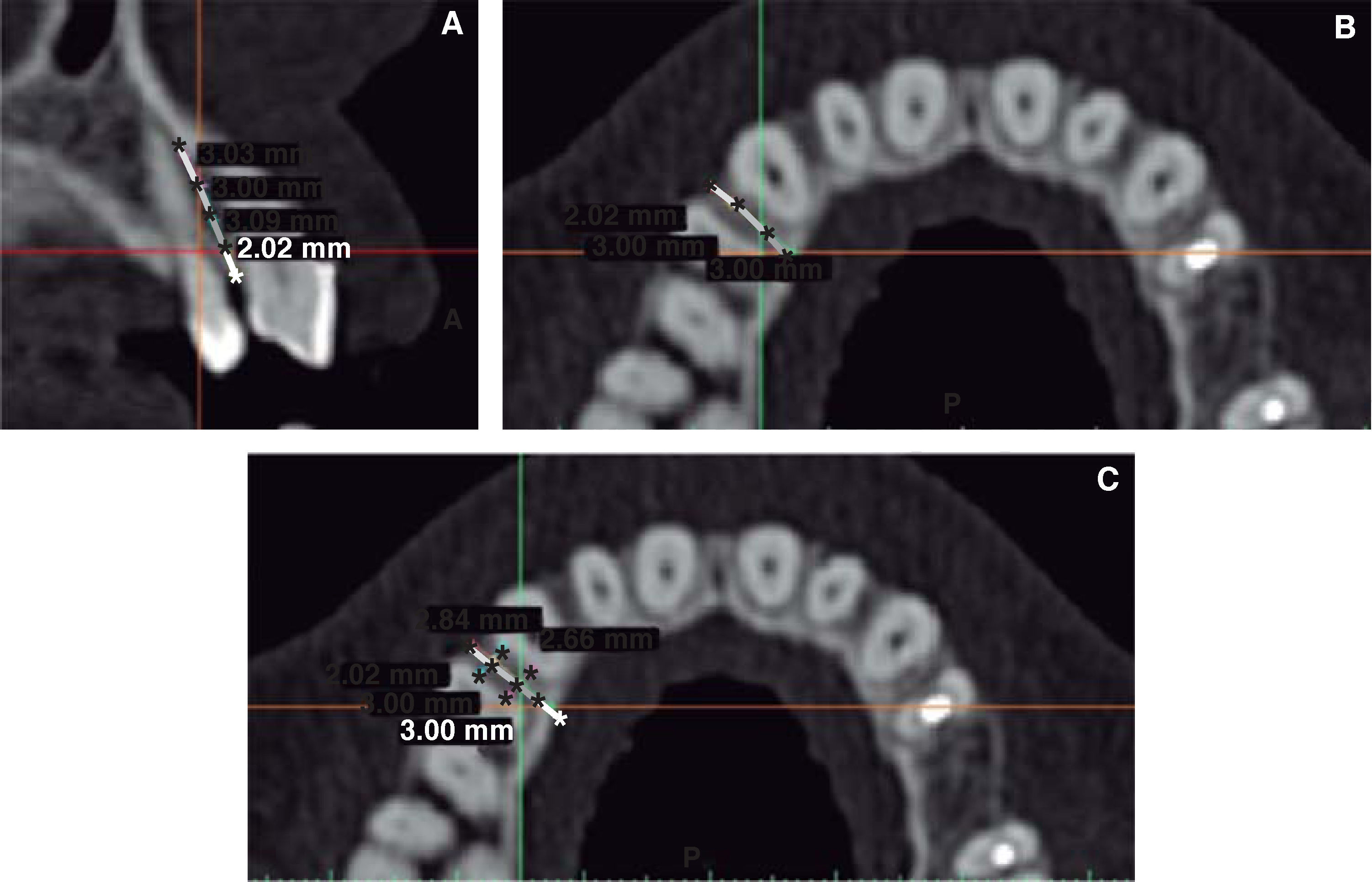
In order to determine the amount of inter-radicular bone, the measurement of the sagittal plane at 2, 5, 8 and 11mm from the alveolar crest with the intersection of the transverse plane at 2, 5 and 8mm from the buccal cortical was obtained from maxillary CT scan images of periodontally compromised patients (Figure 1).1,2
Example to the measurements taken to determine the amount of inter-radicular alveolar bone between the left first premolar and canine. A. Sagittal plane: 2, 5, 8 and 11mm from the alveolar crest. B. Transverse plane: 2, 5 and 8mm from the buccal cortical. C. Measurement of the intersection of the sagittal plane at 2mm with the transverse plane at 2 and 5mm.
The data were obtained by a single operator who in order to achieve reproducible measurements measured 10 scans on two occasions. In specific cases in which in the intersection of both planes no roots were present or only one of the roots was present, the data was not taken, since it was not recognized as an inter-radicular space. In the same way, data was omitted in those cases in which there was no presence of alveolar bone, either because the maxillary sinus was in its place or for some other reason.
The Microsoft Excel program was used to analyze the data. For each point of intersection of the sagittal plane with the transverse plane the mean value, the standard deviation and error were calculated. Data were collected and organized in tables for analysis.
RESULTSFor periodontally compromised patients the possible safe areas were established as those with inter-radicular bone of more than 3mm; between the first molar and the second premolar at 2, 5, 8 and 11mm, between the first and second premolar at 8mm, between the canine and lateral incisor at 5, 8 and 11mm from the alveolar crest (Figure 2).
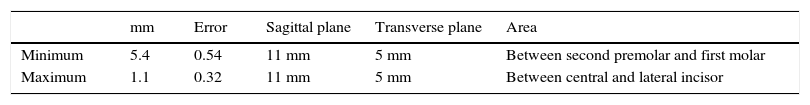
In the maxillary arch, the area with the greatest amount of inter-radicular bone was located between the second premolar and first molar (5.4mm ± 0.54) at the intersection of the 11mm sagittal with the 5mm transverse. The area with the least amount of inter-radicular bone was found between the central and lateral incisors (1.1mm ± 0.32) at the intersection of the 11mm sagittal with the 5mm transverse (Table I).
At 2mm from the alveolar crest, the greatest amount of inter-radicular bone was located in the anterior region between canine and lateral incisor (5mm ± 0.47) at the 8mm intersection with the transverse plane. In the posterior region, it was located between the second premolar and first molar (3.9mm ± 0.34) at the 8mm intersection with the transverse plane. The area with the least amount of inter-radicular bone in in the anterior region was located between the central and lateral incisors (2.1mm ± 0.12) at the 2mm intersection with the transverse plane. In the posterior region, the area with the least amount of inter-radicular bone was located between the second and third molar (1.8mm ± 0.44) at the 5mm intersection with the transverse plane.
At 5mm from the alveolar crest, the greatest amount of inter-radicular bone was located in the anterior area between the central incisors (5.3mm ± 0.32) at the 8mm intersection with the transverse plane. In the posterior region the greatest amount of inter-radicular bone was located between the first molar and the second premolar (3.8mm ± 0.46) at the 8mm intersection with the transverse plane. The area with the least amount of inter-radicular bone was located in the anterior region between the central and lateral incisors (2.3mm ± 0.18) at the 5mm intersection with the transverse plane. In the posterior region it was located between the second and the third molar (1.8mm ± 0.50) at the 5mm intersection with the transverse plane.
At 8mm from the alveolar crest, the greatest amount of inter-radicular bone was located in the anterior zone between the central incisors (5.3mm ± 1.61) at the 8mm intersection with the transverse plane; in the posterior area it was located between the second premolar and first molar (5.3mm ± 0.92) at the 8mm intersection with the transverse plane. The area with the least amount of inter-radicular bone was located in the anterior region between the central and lateral incisors (2.2mm ± 0.24) at the 5mm intersection with the transverse plane; in the posterior area, it was located between the second and the third molar (1.4mm ± 0.47) at the 2mm intersection with the transverse plane.
At 11mm from the alveolar crest, the greatest amount of inter-radicular bone was located in the anterior area between the central incisors (4.8mm ± 0.45) at the 5mm intersection with the transverse plane; in the posterior area, it was found between the second premolar and first molar (5.4mm ± 0.54) at the 5mm intersection with the transverse plane respectively. The area with the least amount of inter-radicular bone was located in the anterior zone between the central and lateral incisors (1.1mm ± 0.32). At the 5mm intersection with the transverse plane, in the posterior area, it was located between the first and the second molar (1.2mm ± 0.61) at the 2mm intersection with the transverse plane (Table II).
Mean values, minimum and maximum, of the amount of inter-radicular bone (in mm.) in each sagittal plane. Average, minimum and maximum of the inter-radicular bone amount.
| Sagital | Mean in mm | Error | Transverse plane | Area | ||
|---|---|---|---|---|---|---|
| 2 mm | Maximum | Anterior | 5 | 0.47 | 8 mm | Between lateral incisor and canine |
| Posterior | 3.9 | 0.34 | 8 mm | Between second premolar and first molar | ||
| Minimum | Anterior | 2.1 | 0.22 | 2 mm | Between central and lateral incisors | |
| Posterior | 1.8 | 0.44 | 5 mm | Between second and third molar | ||
| 5 mm | Maximum | Anterior | 5.3 | 0.32 | 8 mm | Between the central and lateral incisors |
| Posterior | 3.8 | 0.46 | 8 mm | Between the second premolar and first molar | ||
| Minimum | Anterior | 2.3 | 0.18 | 5 mm | Between central and lateral incisors | |
| Posterior | 1.8 | 0.50 | 5 mm | Between the second and third molar | ||
| 8 mm | Maximum | Anterior | 5.3 | 1.61 | 8 mm | Between the central incisors |
| Posterior | 5.3 | 0.92 | 8 mm | Between the second premolar and first molar | ||
| Minimum | Anterior | 2.2 | 0.24 | 5 mm | Between the central y el lateral incisors | |
| Posterior | 1.4 | 0.47 | 2 mm | Between the second and third molars | ||
| 11 mm | Maximum | Anterior | 4.8 | 0.45 | 5 mm | Between the central incisors |
| Posterior | 5.4 | 0.54 | 5 mm | Between the second premolar and first molar | ||
| Minimum | Anterior | 1.1 | 0.80 | 2 mm | Between central and lateral incisors | |
| Posterior | 1.2 | 0.61 | 2 mm | Between the first and second molar |
The aim of this study was to locate, by means of cone-beam tomographies, adequate inter-radicular spaces for mini-implant placement in the maxilla of periodontally compromised patients.
It is important to compare the amount of available alveolar inter-radicular bone with the diameter of the mini implant in order to place them without affecting periodontal health and mini-implant stability. Most straight mini-implants have diameters ranging from 1.2 to 2mm as well as tapered mini-implants that have an initial 1.5mm diameter which decreases until it reaches the tip with a 1.2 to 1.1mm diameter.5
Currently there is not enough data on the amount of bone necessary between mini-implant and dental roots. Taking into consideration that the width of the periodontal ligament is approximately 0.25mm, it is assumed that a free space of at least 1mm of alveolar bone around the mini implant is sufficient to preserve periodontal health. Pablo Echarri et al recommend a minimum space of 3mm between the roots when using tapered devices of 1.6mm. Other authors mention as safe areas those that have values greater than 3.1mm for the placement of mini-implants with a maximum diameter between 1.2-1.3mm. Finally, miniimplants with a diameter of 1.5mm require at least an inter-radicular space of 3.5mm. 1.6 Therefore the safe areas for mini-implant placement were established as those that transversely assessed have at least 3mm of cortical bone at 2, 5 and 8mm.
Studies performed in patients with ideal occlusions show that it is possible to obtain a 3-mm space between the roots of the first and second molar at 8mm, between the second premolar and first molar at 3mm, between the first and second premolar at 2mm, between the canine and the first premolar at 7mm, between the lateral incisor and canine at 8mm and between the central and lateral incisor at 7mm.6 Poggio et al mentioned in patients with ideal occlusion as safe areas for mini-implant placement the following: from the alveolar crest, between the first and second premolar and between the first premolar and canine at 11mm; between the first molar and second premolar at 5 and 8mm.2 Other authors recommend between 6 and 9mm from the alveolar crest between the second premolar and first molar in patients with ideal occlusion.1
With the obtained results the selected biomechanics for certain types of treatment may be affected so alternative biomechanics should be considered in nonrecommended areas for mini-implant placement. For example, instead of placing the mini-implant in the area between central and lateral incisor for deep overbite correction, the area between canine and lateral incisor with an indirect anchorage could be an option.
Likewise, mini-implant placement at 2mm from the alveolar crest could facilitate anchorage for anteroposterior dental movements but it could hinder other biomechanics such as dental intrusion for absolute vertical anchorage.
Other authors state that the mini-implant head may be placed above or under the mucogingival junction depending on the desired biomechanics. If intrusion forces are required, the mini-implant should be placed ideally above the mucogingival line bearing in mind that the mini-implant head might invaginate into the gingival mucosa. If the necessary movement vector is anteroposterior such as distalization, it is recommended to insert the mini-implant at the mucogingival junction level or underneath it since this location improves the horizontal force component.1,7,8 Keratinized gingiva presents better clinical conditions for miniimplant placement such as diminished possibility of inflammation and hyperplasia development than the alveolar mucosa and at the same time, promotes longterm stability.9
The mini-implant insertion site will depend on the selected biomechanics as well as the patient's anatomy since in some cases the alveolar vestibule depth, the mucogingival junction, the palatine foramen or the degree of alveolar bone loss may interfere with the treatment plan.
The maxillary sinus in the posterior region must be considered since periodontally compromised patients may present a pneumatized sinus. Kim established the mean distances between the root apex of maxillary teeth and the lower maxillary sinus wall in patients with an ideal dentition. For the first premolar it was stablished at 6mm, for the second premolar, 5mm; first molar, 4mm; second molar, 3mm.5 These distances have not yet been studied in periodontally compromised patients, but some authors have mentioned that in most cases of periodontally compromised dentitions there is no risk of perforation of the maxillary sinus. However, there is a 20% chance that the mini-implant might enter the maxillary sinus when inserted from the buccal side. A 30 to 60° inclination is recommended to obtain more interradicular space during mini-implant insertion and also, to introduce it in a more horizontal manner to avoid maxillary sinus perforation when the mini-implant is planned to be placed more apically.6
Nasal fossae do not usually pose a risk for miniimplant insertion due to the broad distance between the root apex of the incisors and the floor of the nasal cavity, however, the deeper the insertion is into the vestibule, the more horizontal the mini-implant has to be placed in order to avoid perforation.6
Mini-implant placement between the maxillary incisors is not recommended due to the presence of the labial frenum thus, even though there is enough inter-radicular space, it is not considered a safe area because a lot of mobile soft tissue may cause pain and inflammation.6
Buccal alveolar cortical depth ranges between 1 and 1.5mm until the distal portion of the second molar. In this area, the cortical becomes thinner which may be a contraindication for mini-implant placement between molars since cortical depth is considered a determining factor for its retention.
The buccal free gingival has approximately a 2mm depth and the attached gingiva, 1.5mm. It has been suggested that mini-implants should enter the bony tissue between 4 and 5mm so 6-8mm-length mini-implants are recommended to increase stability bearing in mind that the external cortical plate is their main source of retention.6
Alveolar crest height was a limitation for this study since it varies among patients. Even though this research attempts to provide an anatomical guide of areas with more inter-radicular bone for mini-implant insertion, mini-implant success or failure involves many factors. It is necessary for the orthodontist to clinically and radiographically assess the patient carefully considering the anatomy and the intended biomechanics. Therefore, this study merely provides a clinician's guide for mini-implant placement in periodontally compromised patients. It is suggested to perform similar studies for mini-implant placement in the mandible.
CONCLUSIONSConsidering the values obtained from the CBCT's and the anatomical recommendations for mini-implant placement as an absolute orthodontic anchorage, the recommended safe areas are for mini-implant placement in the buccal cortical of the maxillary arch of periodontally compromised patients are interradicular areas larger than 3mm from the alveolar crest in the posterior region; between the first molar and second premolar at 2, 5, 8 and 11mm from the alveolar crest; between the second premolar and first premolar at 8mm and between lateral incisor and canine at 5, 8 and 11mm.
To Laboratorio Chopo San Borja for granting us access to their database and 3D Tec Venezuela for their program.
Third-year resident of the Orthodontics Specialty at the Post-Graduate Studies and Research Division.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia