The case of a 20 year old man with severe class III maloclussion due to mandibular prognathism and maxillary retrusion who also presents severe laterognathia with condylar hyperplasia and deficient zygomatic projection with dental crowding caused by a collapsed maxilla is hereby presented. The treatment objectives were: to establish a correct overbite and overjet, to provide an stable occlusion and correct the sagittal and transversal problems as well as to improve function in order to promote a better quality of life. Treatment consisted in 3 phases: presurgical orthodontics, the surgical procedure and a postsurgical orthodontic phase. The maxilla was advanced 5mm and intruded 3mm in the posterior region with a Le Fort I osteotomy. A vertical osteotomy with an extraoral approach was performed in the mandible for the correction of the laterognathia. Intermaxillar fixation was used after surgery. Treatment results exceeded the expectations for the clinicians and for the patient himself by achieving a correct function and improving significantly the patient’s aesthetics.
Se trató a un paciente de 20 años de edad con maloclusión severa clase III; debido al prognatismo mandibular y a la retrusión maxilar presenta también laterognasia grave con hiperplasia condilar y proyección malar deficiente con apiñamiento dental que fue causado por un colapso maxilar. Los objetivos del tratamiento fueron: proporcionar una oclusión estable y corregir tanto el problema sagital, como el transversal, así como la mejorara de la función; todo ello con el fin de proporcionar una mejor calidad de vida. El tratamiento consistió en tres fases, las cuales fueron: ortodoncia prequirúrgica, procedimiento quirúrgico y ortodoncia postquirúrgica. El maxilar se adelantó 5mm y 3mm de intrusión posterior con osteotomía Le Fort I y con una osteotomía vertical de rama mandibular con abordaje extraoral para realizar la corrección de la laterognasia. Los resultados del tratamiento rebasaron las expectativas del propio paciente y se logró una función correcta además de mejorar significativamente la estética del paciente.
When facial asymmetry is very severe, it can diminish the patient’s quality of life. Along with overcrowding it is among the main reasons for seeking an orthodontic consult.
The age at which the patient arrives for consultation is crucial in the decision for the kind of treatment: when the perio d of active growth has passed and the degree of the problem is too severe the only treatment option is an interdisciplinary procedure between orthodontics and surgery.1
Some patients have problems adapting to significant changes in their facial appearance. This tends to be a bit more problematic for older patients.
An important and influential factor in the short term about the reaction of the patient to the surgical treatment is the degree of awareness between the actual experience and the patient’s expectations.2
Generally patients who are candidates for orthognathic surgery present a natural compensation to their malocclusion which is why it is of great importance to let the patient know at the time when orthodontic decompensation happens, that the asymmetry and the maxillofacial discrepancy will be more noticeable.3
In cases of prognathism and maxillary collapse a transverse compensation of both arches may exist so it is also important to match the size of the dental arches transversally in order to provide a correct oclusion.4
Case reportMale patient of 20 years of age presents to the Clinic of Orthodontics with the following chief complaint: «I do not bite well».
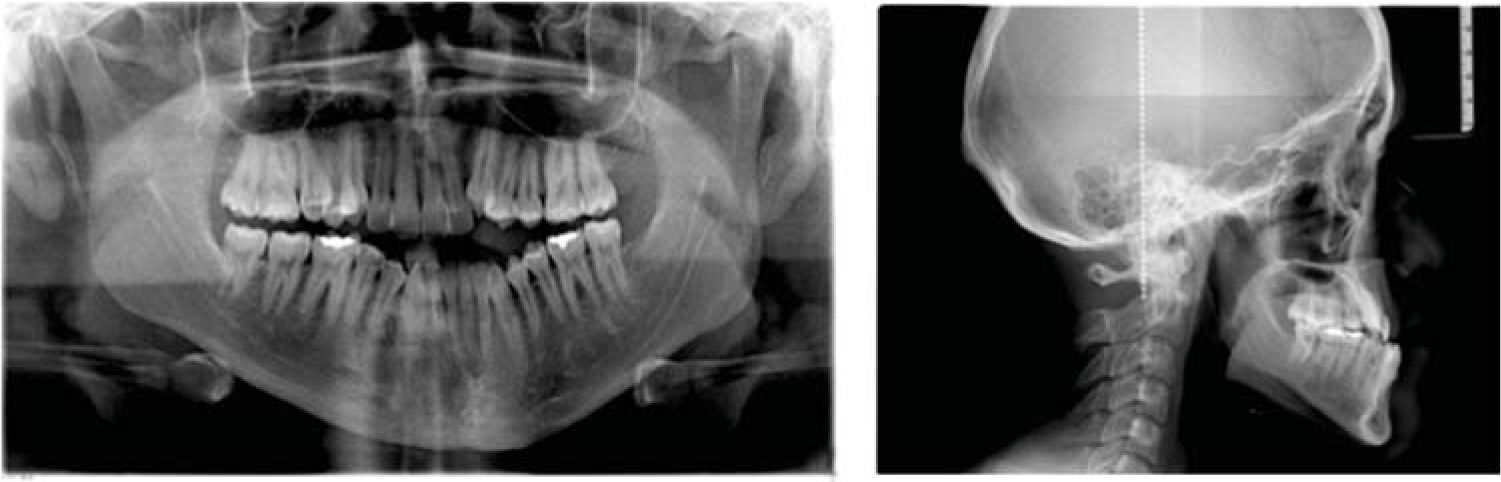
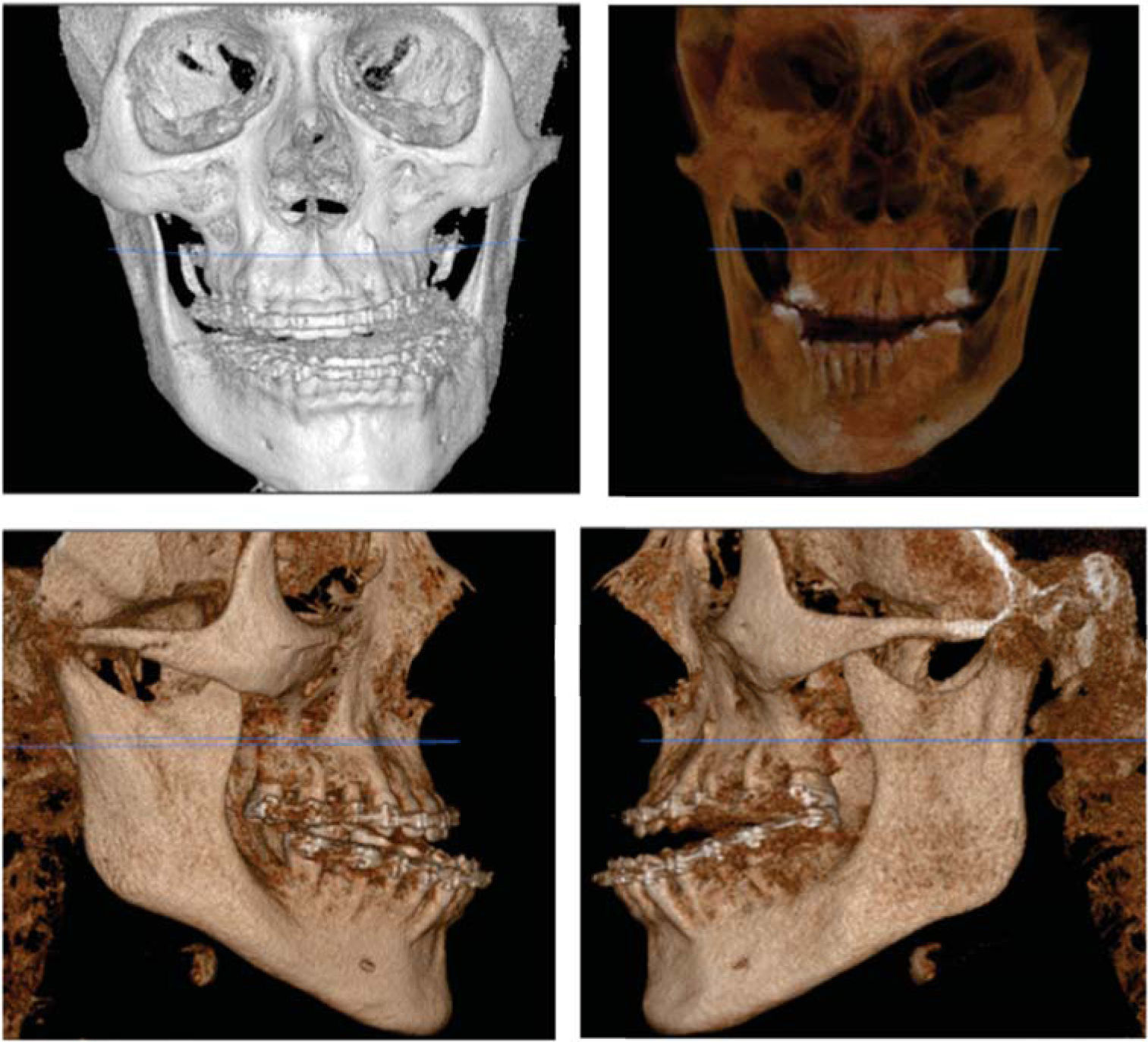
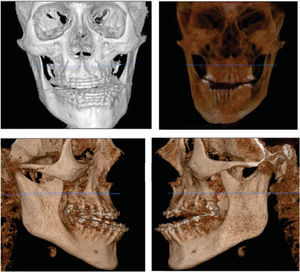
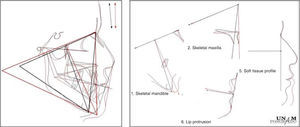
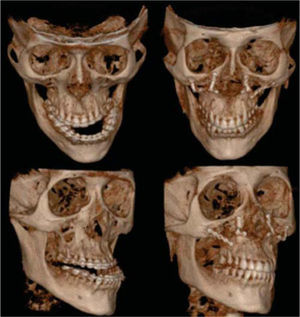
Cephalometrically, a skeletal class III by prognathism and maxillary hypoplasia was observed, a laterognathia with severe unilateral condylar hyperplasia was present and also a zygomatic-malar depression (Figures 1and2).
The treatment consisted of three phases: presurgical orthodontics, orthognathic surgery and post-surgical orthodontics. A 5mm maxillary advancement with a posterior intrusion of 3mm was performed as well as vertical osteotomies of the mandibular ramus with extraoral access. The fixation was intermaxillary.
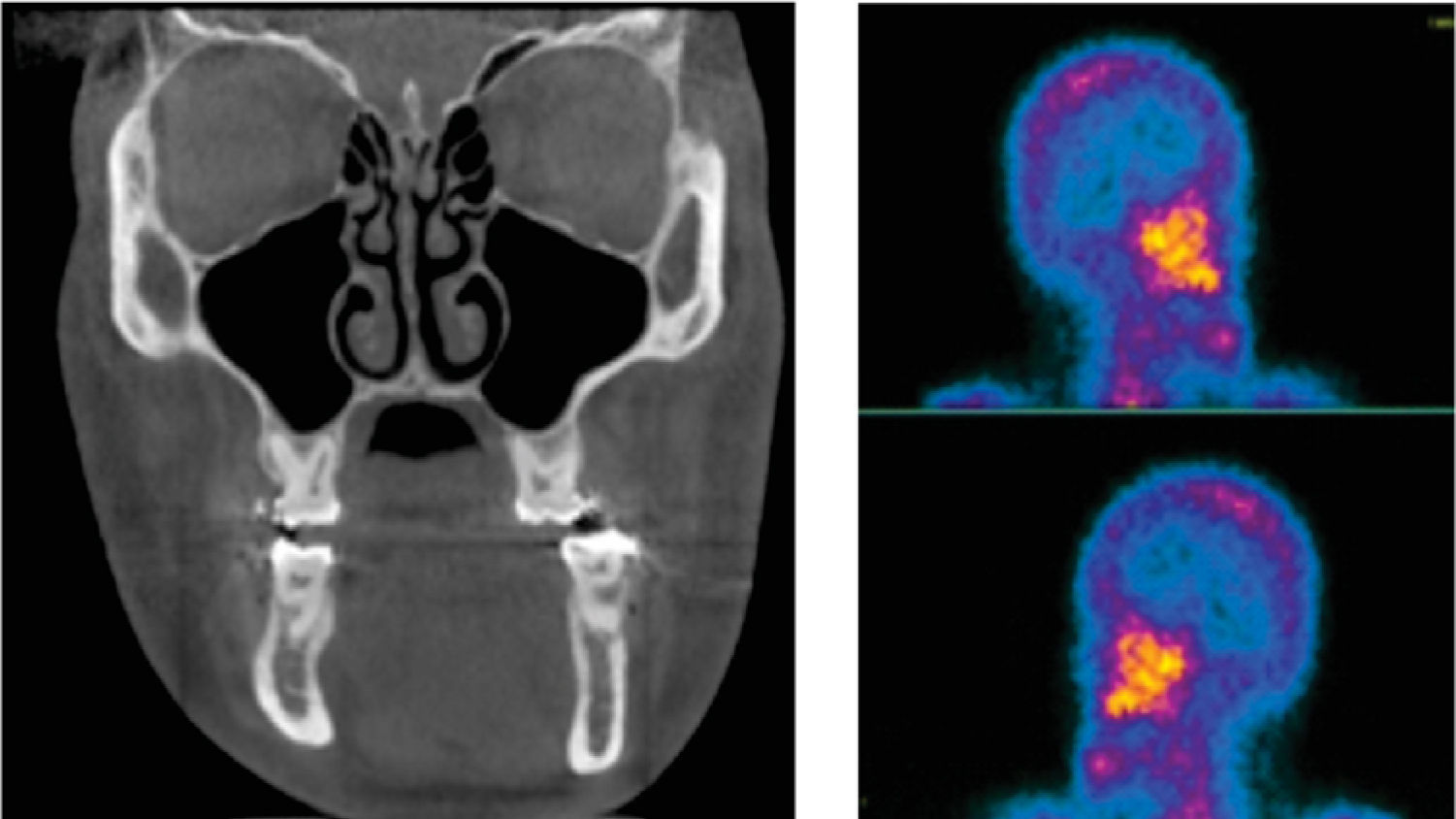
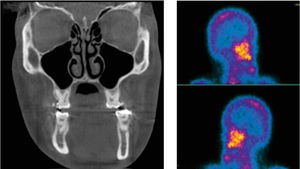
A gammagraphy was requested with the purpose of ruling out active condylar growth (Figure 3).
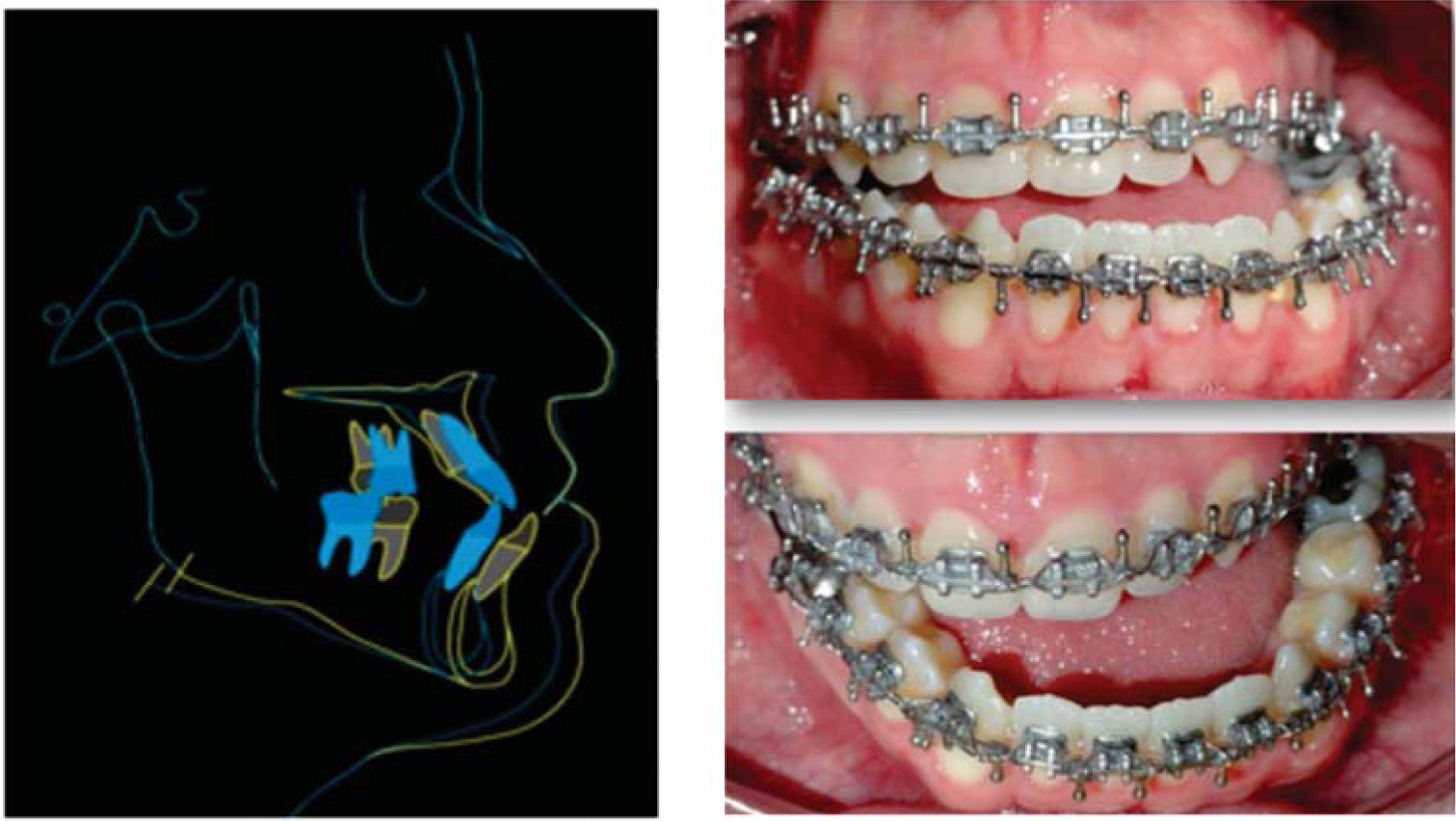
Intraorally, there is a collapsed maxillary dentition with severe crowding in the upper arch and moderate crowding in the lower (Figure 4).
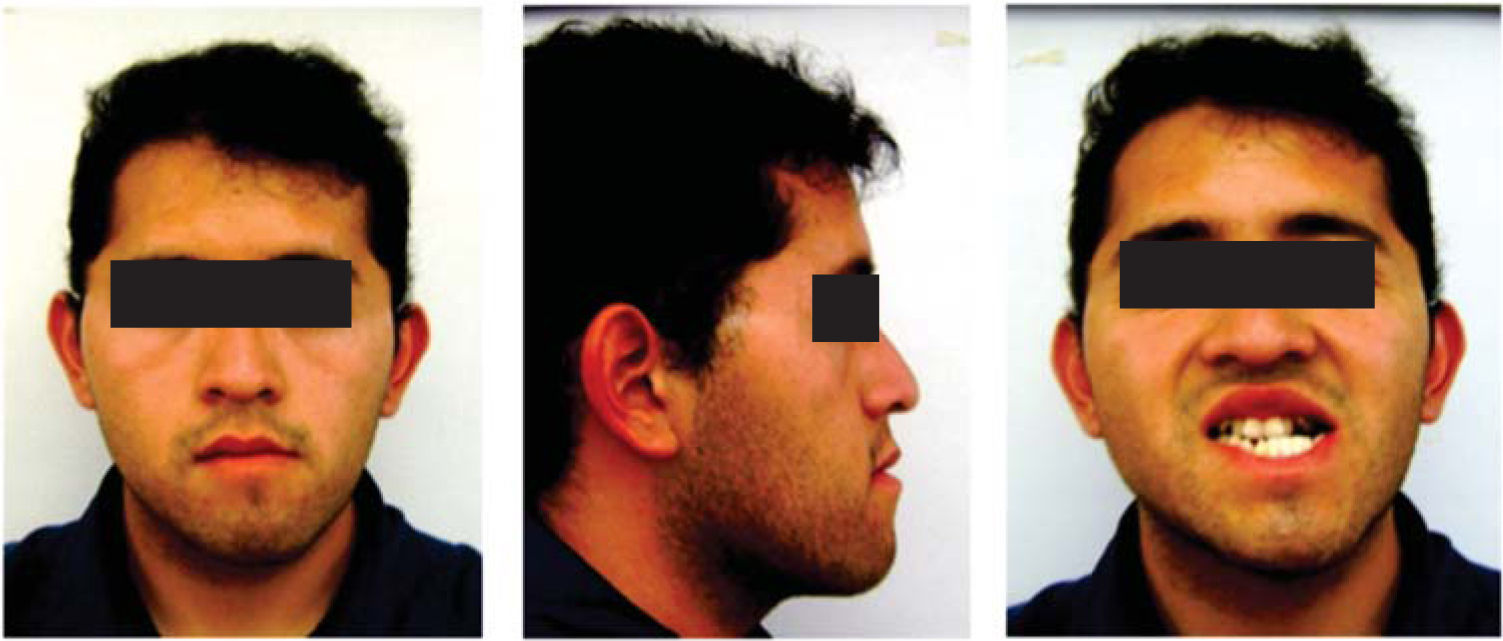
On the facial analysis, a considerable asymmetry and a depression of the middle third is observed (Figure 5).
Treatment optionsDue to the collapsed maxilla, the posterior crossbite and age of the patient at the initial time of treatment, the treatment options were: a SARPE (Surgically Assisted Palatal Expansion) which would resolve the patient’s transverse problem, presurgical orthodontics and a second bimaxillary surgery to solve the sagittal problem.
Faced with the refusal of the patient for a second surgical intervention a second treatment plan is designed: upper premolar extractions to resolve the crowding and upper dental proclination, presurgical orthodontics and bimaxillary surgery followed by postsurgical orthodontics.
Treatment planAfter consulting with the patient, the following treatment plan is chosen:
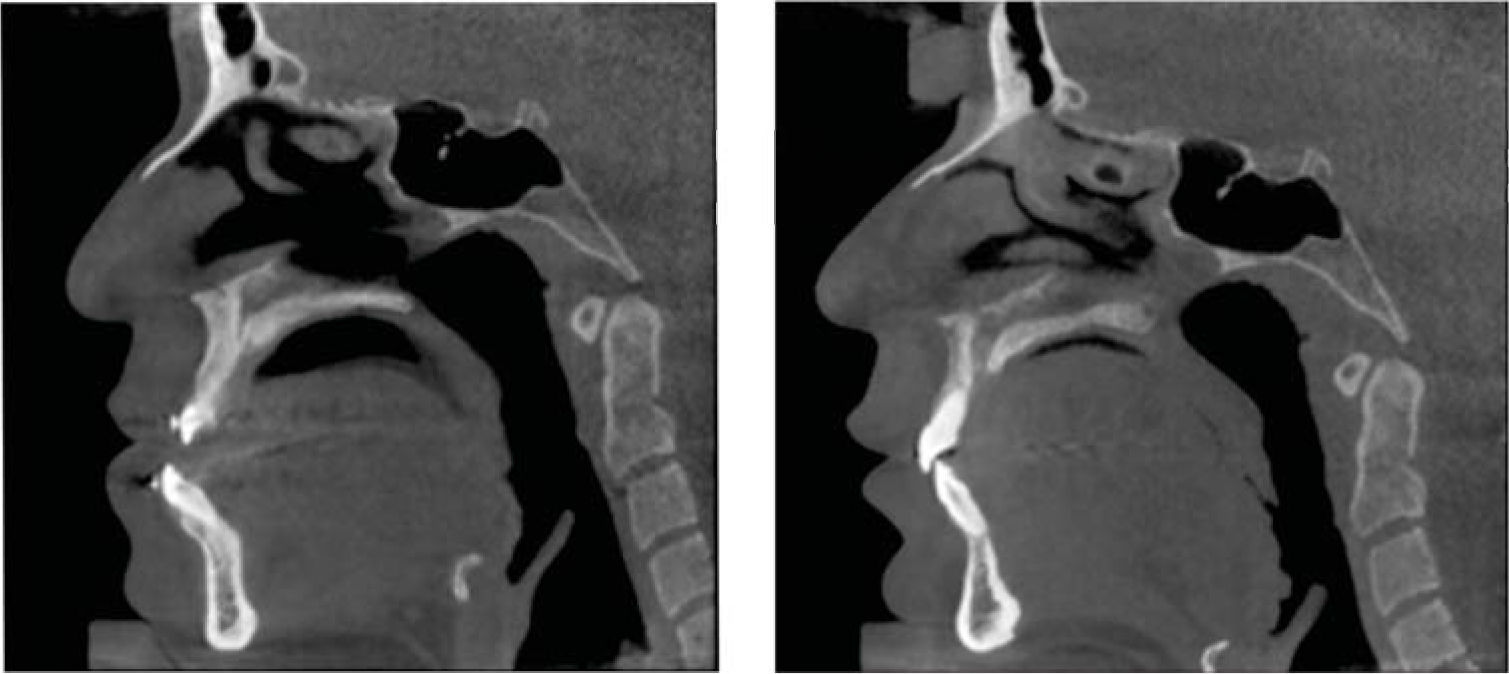
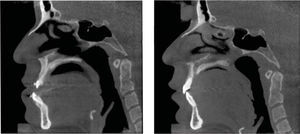
Treatment progressExtractions of the dental organs 15 and 24 were performed and fixed orthodontic appliances, .022 slot Roth prescription, bands in 1st and 2nd molars were placed. With that procedure, the pre-surgical decompensation begins. Alignment and leveling: the dental collapse in the upper arch is eliminated. By correctting the compensation with dental retroclination oftheupperincisorsandproclinationofthelower teeth, they are aligned into their bony bases and ready for surgery. The patient is subjected to a Cone Beam CT scan to be sure that there was no damage to the external cortical of the maxilla. The orthodontic surgical prediction was sent to the Department of Maxillofacial Surgery. Along with the surgery of models, it was arrived to a consensus surgical treatment plan (Figure 6).
Prior to surgery routine laboratory analysis are carried out and additionally, a bone scan (SPECT bone of the skull and facial massif with MDP-Tc-99m) was requested to make sure that there was no active cell proliferation at the level of the condyle which could cause a relapse in the asymmetry and the laterognathia caused by the condylar hyperplasia on the right side.
The surgery was in charge of the maxillofacial surgeon Juan Carlos Lopez Noriega and the fourth-year resident Carlos Acosta Behrends from the department of maxillofacial surgery. In a surgery that lasted four and a half hours under general anesthesia the following was performed: maxillary advancement: 5mm. Posterior intrusion 3mm. A high Le Fort I was performed to correct the zygomatic deficiency. Vertical osteotomies of the mandibular ramus with extraoral access were performed to correct the asymmetry and check the verticality of the patient. An intermaxillary fixation was placed and the patient had his mouth closed for four weeks (Figure 7).
A week after surgery, the patient is referred to the orthodontics clinic for intermaxillary elastic control of the patient’s tendency towards mandibular deviation recalling that although at that time the discrepancy had been corrected, the patient continues to have a laterognathic musculature. Thus, it was necessary to keep the jaw in a stable position to avoid postsurgical relapse.
During surgery and the post-surgery weeks several brackets debonded so it was to order a panoramic radiograph to reposition and replace the lost appliances.
Prior to the withdrawal of the appliances, a braided .019×.025 upper archwire and short 5/16” 4.5 oz elastics are placed to allow occlusal settlement.
After debonding the appliances, final models are taken for the confection of the retainers.
In the lower arch, 3 to 3 fixed retention was placed with twisted wire .0175. In the upper arch, a circumferential retainer was placed.
In addition, a miofunctional retainer was made for use at night as a reminder for the patient’s asymmetrical musculature.
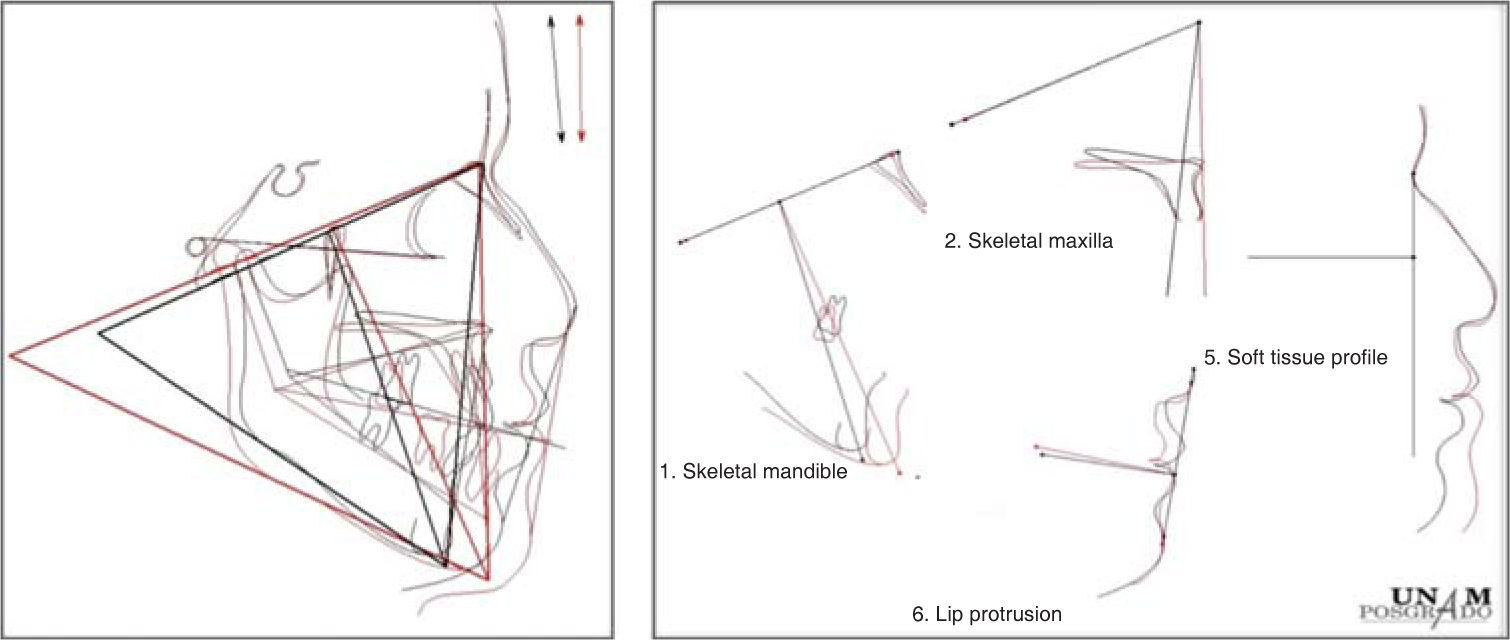
ResultsThe extra and intraoral photographs show positive results. The facial asymmetry was corrected, the midface depression and the zygomatic- malar deficiency improved. The profile changed significantly due to the maxillary advancement and the mandibular retrusion. Cephalometrically, the dental compensation was corrected and the verticality of the patient decreased due to the maxillary intrusion and mandibular auto rotation (Figure 8).
Oclussally, the bilateral posterior crossbite was corrected. Canine class I and an adequate posterior intercusp relationship in functional molar class II were obtained as well as a correct overbite and overjet and canine guidance as a disoclussion system. The facial and dental aesthetics improved (Figure 9).
DiscussionA high Le Fort I osteotomy is favorable for the correction of maxillary deficiencies and lack of zygomatic projection. At the same time, the choice of vertical osteotomies in the mandible along with the posterior maxillary intrusion allowed the redirection of the mandible by counter-clockwise rotation (Figure 10).5
Beyond the dramatic changes that were observed both facial and dentally, we observed positive changes in the patient’s attitude and self-esteem thus improving his quality of life. It is of the utmost importance to identify the patient’s expectations as well as the limitations that the case might have (Figure 11).
At present, a 6-month follow-up is being conducted and afterwards, a 1-year follow-up to observe the case’s stability degree.
ConclusionsA correct diagnosis as well as the correct interdisciplinary planning is essential for a successful treatment. We must take into consideration the limitations that a treatment may have when it is performed only by orthodontic camouflage, as well as the anatomical limitations that orthognathic surgery has in severe discrepancies such as the present case.
It is important to psychologically prepare the patient to accept the major changes that occur during and after the surgical-orthodontic treatment (Figure 12).
Retention in this type of treatment must be strict and use in addition to the conventional retainer a miofunctional appliance to prevent relapse since even though the treatment objectives were achieved, it must be remembered that the patient’s musculature continues to be laterognathic and must be adapted to the new functional demands.