The aim of this work was to compare the distribution of disordered eating behaviors (DEB) in Mexican adult patients, with and without type 2 diabetes. A cross-sectional descriptive and comparative field research was carried out in a sample of 169 subjects (54% females; 46% males) with a mean age of 47.9 years. The sample was matched in two groups: patients with type 2 diabetes and patients without diabetes. DEB were assessed with a valid Mexican scale named EFRATA (Escala de Factores de Riesgo Asociados a Trastornos Alimentarios). Results confirmed significant differences in food and weight concern (t=4.15, df 152.09, p=0.000), normal eating behavior (t=4.03, df 151.45, p=0.000) and emotional eating (t=1.93, df 160.76, p<0.05), EFRATA's factors in which diabetic subjects obtained higher values in comparison with no diabetic patients. Subjects without diabetes achieved higher value only in binge eating behavior with statistically significant difference (t=2.11, df 128.8, p<0.05) in contrast with diabetic patients. Since these findings have been open the possibility to propose specific strategies that encourage healthy eating behaviors, both in adult patients with and without diabetes.
El objetivo de este estudio consistió en comparar la distribución de conductas alimentarias de riesgo en pacientes mexicanos adultos con y sin diabetes tipo 2. Se efectuó un estudio de campo de tipo descriptivo y comparativo en una muestra de 169 sujetos (54% mujeres; 46% hombres) con una media de edad de 47,9 años. Los sujetos fueron divididos en 2 grupos: pacientes con diabetes y pacientes sin diabetes. Para medir las conductas alimentarias de riesgo se empleó la Escala de Factores de Riesgo Asociados a Trastornos Alimentarios (EFRATA). Los resultados confirmaron diferencias significativas en preocupación por el peso y la comida (t=4,15, df 152,09, p=0,000), conducta alimentaria normal (t=4,03, df 151,45, p=0,000) y en comer por compensación psicológica (t=1,93, df 160,76, p<0,05), factores de la EFRATA en los que los pacientes diabéticos registraron valores más altos. En contraste con los pacientes diabéticos, los sujetos sin diabetes alcanzaron el valor más alto con diferencia estadísticamente significativa en el factor comer compulsivo (t=2,11, df 128,8, p<0,05). A partir de estos hallazgos se abre la posibilidad de proponer estrategias puntuales que favorezcan conductas alimentarias saludables, tanto para pacientes adultos diabéticos como sin diabetes.
Diabetes is one of the most devastating diseases of the century, with an economic burden both on families and on society. The incidence and prevalence of this disease have increased progressively in the entire world, and particularly in America (World Health Organization, 2004). The International Diabetes Federation (2011) estimates that there are 366 million people with diabetes and another 280 million are at identifiably high risk of developing diabetes, such that there will be more than 552 million with diabetes and an additional 398 million people at high risk by 2030. Moreover three out of four people with diabetes now live in low and middle-income countries. Further the World Diabetes Foundation estimates that 1.1 million people died of diabetes in 2005. Nearly 80% of deaths related to diabetes occur in countries with low and middle income; approximately half of deaths by diabetes occur in people under 70 years old and 55% of them are women (American Diabetes Association, 2009).
In Mexico, diabetes represents a public health problem (Hernández-Ávila, Gutiérrez, & Reynoso-Noverón, 2013) that affects all social classes (Evaristo-Neto, Foss-Freitas, & Foss, 2010; Genz et al., 2014; International Diabetes Federation, 2013). The National Health and Nutrition Survey (ENSANUT 2006; Olaiz-Fernández et al., 2006) reported a prevalence of diabetes of 14% in the 20–79 age group, which represents 8 million Mexicans with diabetes in the country. In Hidalgo State, the prevalence of diabetes in adults older than 20 years was 7.1%, being higher in women (7.9%) than in men (5.9%). Recently, ENSANUT 2012 (Gutiérrez et al., 2012) has reported that adults’ proportion with a prior diagnosis of diabetes was 9.2%, showing an important increase compared to ENSANUT 2006 (7%; Olaiz-Fernández et al., 2006).
On the other hand, some researchers had proposed that disordered eating behaviors (DEB) could instigate, at least theoretically, the onset of type 2 diabetes mellitus (Cleator et al., 2013; Mannucci et al., 1997). Furthermore, there have been suggestions that binge eating behaviors may contribute to earlier onset of this disease, possibly via its impact on weight (Khalida, 2008; Mannucci et al., 2002). It is important to underline that DEB are abnormal eating behaviors that include binge eating with loss of control and extreme weight control behaviors (i.e., self-induced vomiting, dietary restraint and use of diet, pills, laxatives, or diuretics) associated with an increased subsequent apparition of an eating disorders (ED) as anorexia nervosa, bulimia nervosa or binge eating disorder (Asociación Americana de Psiquiatría, 2002).
Few studies have addressed DEB in patients with type 2 diabetes; besides they have been performed on only a small number of patients (Kenardy, Mensch, Bowen, & Pearson, 1994) or in an obese subpopulation (Mannucci et al., 2002). Binge eating has been reported to be frequent among type 2 diabetic patients (Mannucci et al., 1997) or to have a significant positive relationship with this pathology (Papelbaum et al., 2005).
Goebel-Fabbri (2008) has proposed that DEB are often well hidden and denied by diabetic patients; also they decrease their frequency of glucose monitoring, “forget” to bring blood glucose records to medical appointments, and also find ways to influence blood glucose meters so that they record in-range blood sugars. Additionally, Goebel-Fabbri has identified that the current goals of diabetes management increase the risk to present DEB, precursors of ED.
Even if it is unclear whether DEB are predominant among patients with type 2 diabetes, these have a deleterious effect on glycemic control, increasing the risk for hypoglycemia, hyperglycemia and diabetic ketoacidosis (Affenito et al., 1997), as well as chronic microvascular and macrovascular complications, one of the most important causes of mortality in diabetic patients (Lee, 2013). Thus, early detection of DEB appears to be crucial in the evaluation and treatment of diabetes (Pérez, Barriguete, & Rivera, 2005).
Therefore, the aim of this work was to compare the distribution of disordered eating behaviors (DEB) in a sample of Mexican adult patients, with and without type 2 diabetes. It is hypothesized that there will be a higher prevalence of DEB among patients with type 2 diabetes in comparison to patients without the pathology. In addition, we evaluated the association between body mass index (BMI) and waist circumference (WC), with DEB in both groups.
MethodParticipantsMexican patients were recruited from two health centers in Hidalgo State (Pachuca and Actopan). A cross-sectional descriptive and comparative field research was carried out in a sample of 169 subjects (54% females; 46% males) with a mean age of 47.9 years (SD=±17.6). The sample was matched in two groups: patients with type 2 diabetes (46 females, 39 males); and patients without diabetes (46 females, 38 males). To classify participants, the presence of diabetes was considered when the fasting blood glucose level was ≤126mg/dL and confirmed by the percentage of Glycosylated Hemoglobin (HbA1c) (no diabetes<6%, diabetes≥6%), as recommend the American Diabetes Association (2009). The HbA1c was measured by NycoCard HbA1c-U-albumin-CRP test (recertified by National Glycohemoglobine Standardization Program).
Disordered eating assessment toolDisordered eating behaviors (DEB) were assessed with the EFRATA (Escala de Factores de Riesgo Asociados a Trastornos Alimentarios). This self-reporting instrument was developed and validated for Mexican population by Gómez Pérez-Mitré (2000). The EFRATA has demonstrated good reliability (Cronbach's Alpha 0.86 for males and 0.89 for females) and validity (criterion validity for the single factors ranging from 0.61 to 0.86). The five crucial factors evaluated with EFRATA scale are: binge eating, food and weight concern, normal eating behavior, emotional eating, and dietary restraint. EFRATA is a Likert scale with five response options: (1) never; (2) sometimes; (3) frequently (50% of the time); (4) very frequently (75% of the time); (5) always. Higher scores indicate eating problems, except for a normal eating behavior factor, in which a high score points out no risk. However, when this behavior is not followed correctly, it could become a risk eating behavior.
It is important to point out that the binge eating factor was assessed according to the diagnostic criterion of DSM-IV (Asociación Americana de Psiquiatría, 2002). Food and weight concern is assessed with questions about avoidable foods, such as “tortillas”, pasta and bread. Normal eating behavior is measured as a joint of behaviors that help to maintain or improve general health, such as, increased consumption of vegetables, fruits, whole grains and water when it is followed daily. Emotional eating refers to eat in response to clearly labeled emotions such as sadness, depression or anxiety. As a final point, dietary restraint denotes different unhealthy weight control behaviors such as skipping meals, eating very little or eliminating foods considered “to be fattening” by the subject. For Body Mass Index (BMI) and waist circumference (WC), the categories recommended by the World Health Organization (2006) were used.
The project was approved by the Comité d’étique de la recherché avec les êtres humains de la Faculté des études supérieures et de la recherché (n° dossier 0708-092), Université de Moncton, Canada. Participants were evaluated by two trained nutritionists to ensure the collection of reliable data. All participants signed an informed consent form, and were treated according to the Helsinki declaration (Asociación Médica Mundial, 2009). The subjects were recruited and participated on a voluntary basis and all of them approved using their data for research purposes. Comparisons between psychometric scores by factors were included, as this could enhance the power to detect differences between groups.
Statistical analysisThe software used for data entry and statistical analyses was SPSS version 20 for Windows. EFRATA's factors were transformed into an index. To get this index, the items that formed each factor were averaged; then each average was re-categorized considering the original rating of the instrument (<1.5=1; 1.5–2.5=2; 2.6–3.5=3; >3.5=4). For comparison between groups (patients with and without diabetes) student t test was used with a significance threshold of p<0.05. Spearman's correlation coefficients were applied to identify the relationship between DEB and the nutritional status indicators.
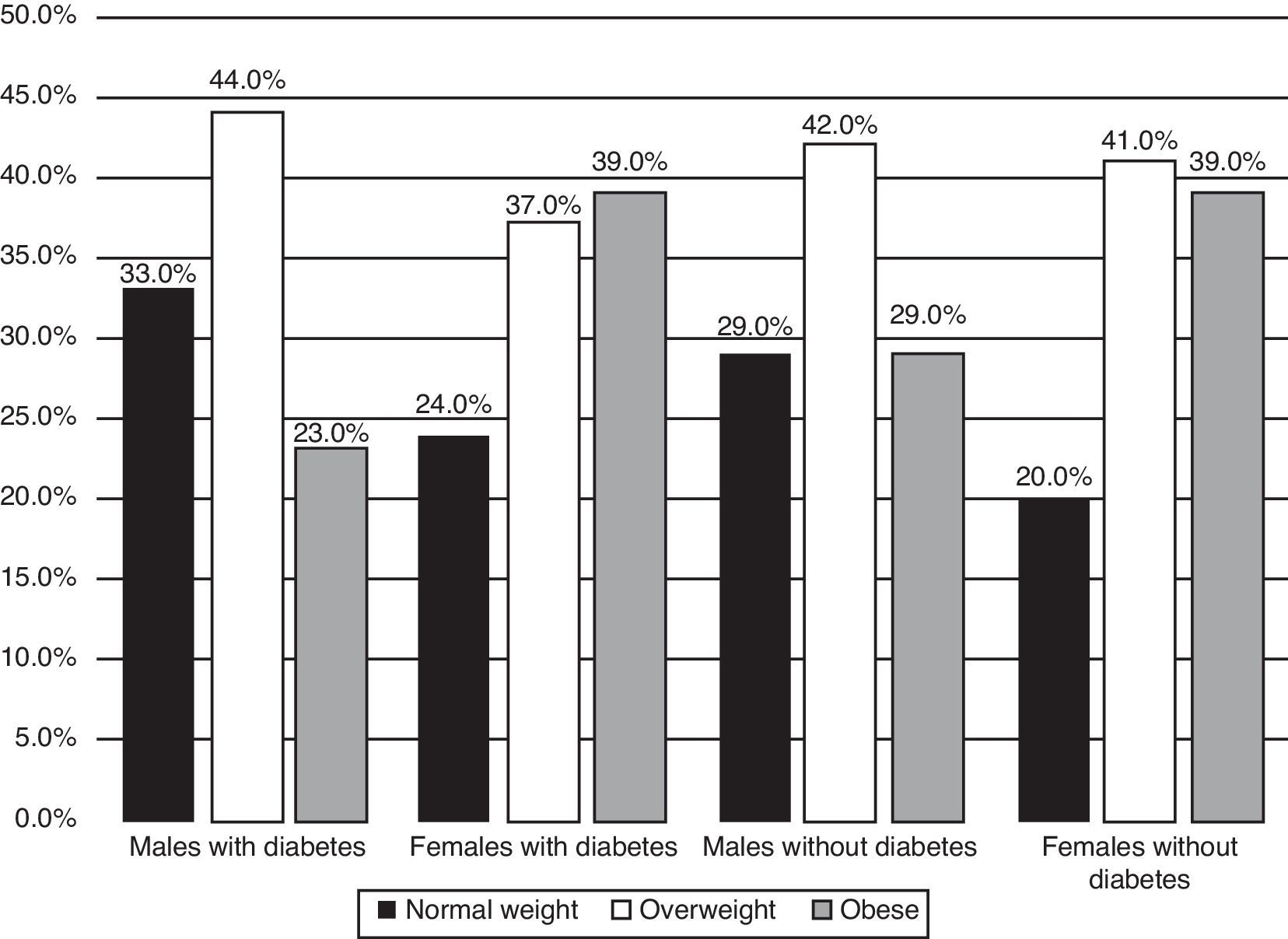
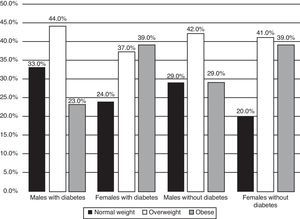
ResultsIn total sample, BMI distribution reported 26% normal weight, 41% overweight and 33% obese. BMI mean in patients with diabetes was 28.29kg/m2 meanwhile in non-diabetic subjects was 28.09kg/m2, there were no statistical differences. It is important to point out that were found similar percentages of patients with and without diabetes (overweight and obese) outstanding 39% of women with obesity in both groups. Underweight subjects were not found. The distribution of BMI by sex and by group is shown in Fig. 1.
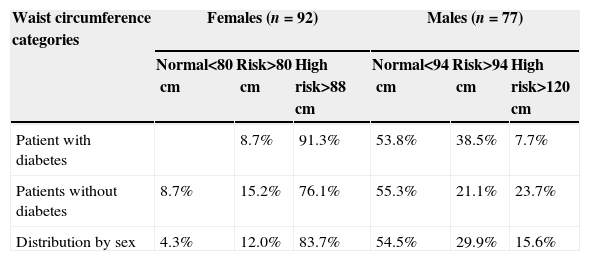
The WC distribution in Table 1 displays that females with and without diabetes reached the highest values of high risk to develop cardiovascular diseases (91.3%, 76.1%, respectively). In males, participants with diabetes reported the highest percentage (38.5%) of risk to develop cardiovascular diseases.
Percentage distribution of waist circumference by group and by sex.
| Waist circumference categories | Females (n=92) | Males (n=77) | ||||
|---|---|---|---|---|---|---|
| Normal<80cm | Risk>80cm | High risk>88cm | Normal<94cm | Risk>94cm | High risk>120cm | |
| Patient with diabetes | 8.7% | 91.3% | 53.8% | 38.5% | 7.7% | |
| Patients without diabetes | 8.7% | 15.2% | 76.1% | 55.3% | 21.1% | 23.7% |
| Distribution by sex | 4.3% | 12.0% | 83.7% | 54.5% | 29.9% | 15.6% |
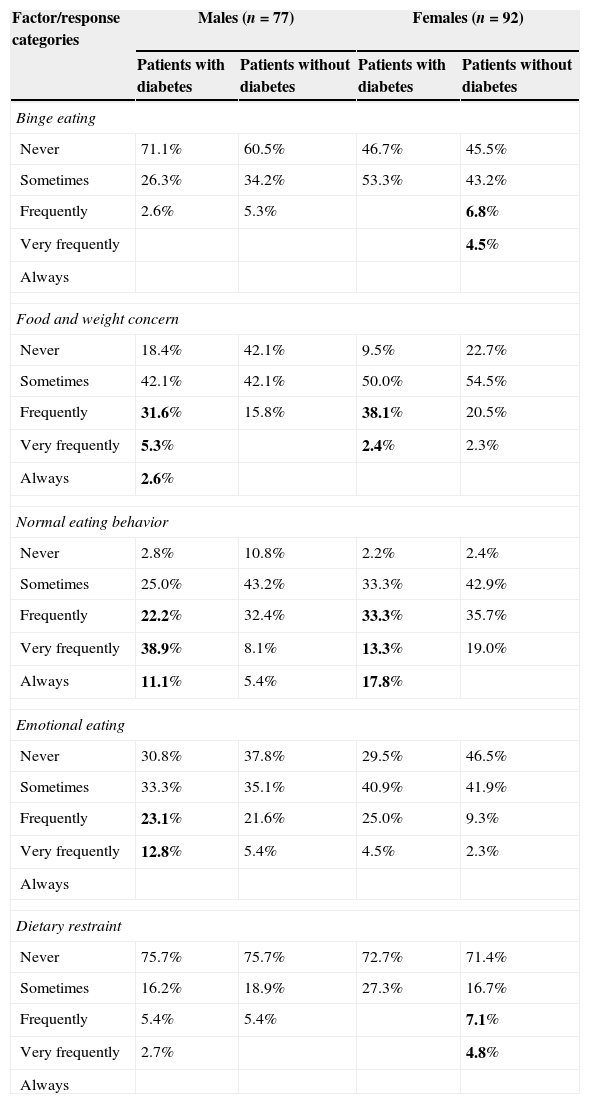
Table 2 shows the percentage distribution of DEB measured by EFRATA. In the group with diabetes, the food and weight concern factor achieved the highest frequency as well as normal eating behavior. Males with diabetes reported the highest frequencies for emotional eating behavior. Lastly, females without diabetes reported binge eating and dietary restraint most frequently.
Distribution of disordered eating behaviors in patients with and without diabetes by sex.
| Factor/response categories | Males (n=77) | Females (n=92) | ||
|---|---|---|---|---|
| Patients with diabetes | Patients without diabetes | Patients with diabetes | Patients without diabetes | |
| Binge eating | ||||
| Never | 71.1% | 60.5% | 46.7% | 45.5% |
| Sometimes | 26.3% | 34.2% | 53.3% | 43.2% |
| Frequently | 2.6% | 5.3% | 6.8% | |
| Very frequently | 4.5% | |||
| Always | ||||
| Food and weight concern | ||||
| Never | 18.4% | 42.1% | 9.5% | 22.7% |
| Sometimes | 42.1% | 42.1% | 50.0% | 54.5% |
| Frequently | 31.6% | 15.8% | 38.1% | 20.5% |
| Very frequently | 5.3% | 2.4% | 2.3% | |
| Always | 2.6% | |||
| Normal eating behavior | ||||
| Never | 2.8% | 10.8% | 2.2% | 2.4% |
| Sometimes | 25.0% | 43.2% | 33.3% | 42.9% |
| Frequently | 22.2% | 32.4% | 33.3% | 35.7% |
| Very frequently | 38.9% | 8.1% | 13.3% | 19.0% |
| Always | 11.1% | 5.4% | 17.8% | |
| Emotional eating | ||||
| Never | 30.8% | 37.8% | 29.5% | 46.5% |
| Sometimes | 33.3% | 35.1% | 40.9% | 41.9% |
| Frequently | 23.1% | 21.6% | 25.0% | 9.3% |
| Very frequently | 12.8% | 5.4% | 4.5% | 2.3% |
| Always | ||||
| Dietary restraint | ||||
| Never | 75.7% | 75.7% | 72.7% | 71.4% |
| Sometimes | 16.2% | 18.9% | 27.3% | 16.7% |
| Frequently | 5.4% | 5.4% | 7.1% | |
| Very frequently | 2.7% | 4.8% | ||
| Always | ||||
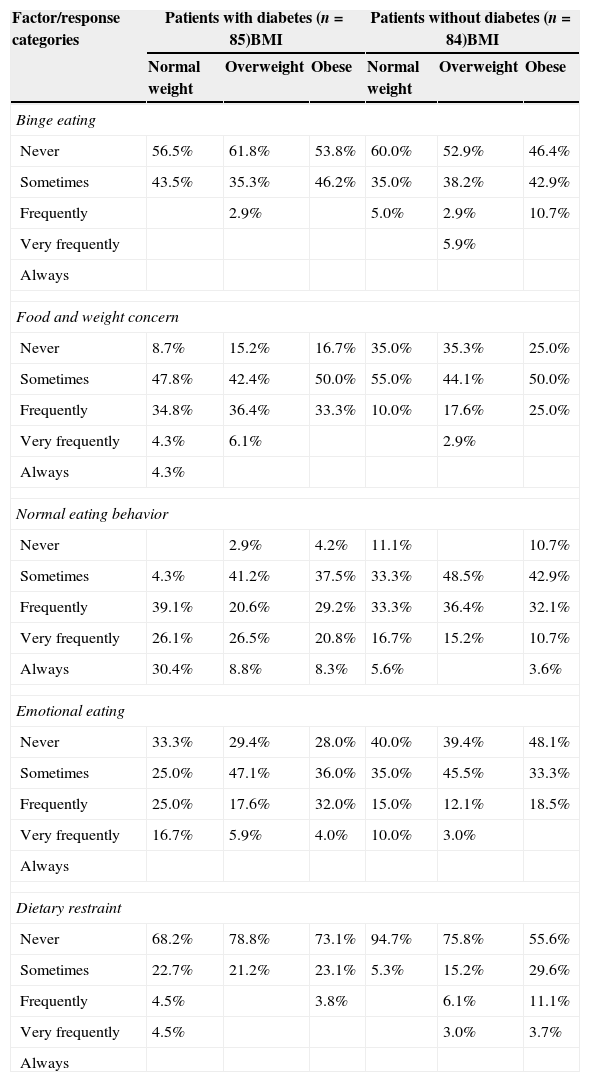
Based on the BMI, Table 3 reveals that patients with diabetes, both normal weight and overweight, reported most often to have food and weight concern. Additionally, normal weight patients with diabetes reported the highest frequencies of normal eating behavior and emotional eating. In the group without diabetes, participants in overweight and obese classes reported the highest percentages for binge eating and dietary restraint rather than diabetic patients in the same BMI categories.
Percentage distribution of patients with disordered eating behaviors based on diabetic status and BMI.
| Factor/response categories | Patients with diabetes (n=85)BMI | Patients without diabetes (n=84)BMI | ||||
|---|---|---|---|---|---|---|
| Normal weight | Overweight | Obese | Normal weight | Overweight | Obese | |
| Binge eating | ||||||
| Never | 56.5% | 61.8% | 53.8% | 60.0% | 52.9% | 46.4% |
| Sometimes | 43.5% | 35.3% | 46.2% | 35.0% | 38.2% | 42.9% |
| Frequently | 2.9% | 5.0% | 2.9% | 10.7% | ||
| Very frequently | 5.9% | |||||
| Always | ||||||
| Food and weight concern | ||||||
| Never | 8.7% | 15.2% | 16.7% | 35.0% | 35.3% | 25.0% |
| Sometimes | 47.8% | 42.4% | 50.0% | 55.0% | 44.1% | 50.0% |
| Frequently | 34.8% | 36.4% | 33.3% | 10.0% | 17.6% | 25.0% |
| Very frequently | 4.3% | 6.1% | 2.9% | |||
| Always | 4.3% | |||||
| Normal eating behavior | ||||||
| Never | 2.9% | 4.2% | 11.1% | 10.7% | ||
| Sometimes | 4.3% | 41.2% | 37.5% | 33.3% | 48.5% | 42.9% |
| Frequently | 39.1% | 20.6% | 29.2% | 33.3% | 36.4% | 32.1% |
| Very frequently | 26.1% | 26.5% | 20.8% | 16.7% | 15.2% | 10.7% |
| Always | 30.4% | 8.8% | 8.3% | 5.6% | 3.6% | |
| Emotional eating | ||||||
| Never | 33.3% | 29.4% | 28.0% | 40.0% | 39.4% | 48.1% |
| Sometimes | 25.0% | 47.1% | 36.0% | 35.0% | 45.5% | 33.3% |
| Frequently | 25.0% | 17.6% | 32.0% | 15.0% | 12.1% | 18.5% |
| Very frequently | 16.7% | 5.9% | 4.0% | 10.0% | 3.0% | |
| Always | ||||||
| Dietary restraint | ||||||
| Never | 68.2% | 78.8% | 73.1% | 94.7% | 75.8% | 55.6% |
| Sometimes | 22.7% | 21.2% | 23.1% | 5.3% | 15.2% | 29.6% |
| Frequently | 4.5% | 3.8% | 6.1% | 11.1% | ||
| Very frequently | 4.5% | 3.0% | 3.7% | |||
| Always | ||||||
To identify statistically significant differences between patients with and without diabetes, student t test was used. Findings confirmed significant differences in food and weight concern (t=4.15, df 152.09, p=0.000), normal eating behavior (t=4.03, df 151.45, p=0.000) and emotional eating (t=1.93, df 160.76, p<0.05), factors in which subjects with diabetes obtained higher values in comparison with no diabetic patients. Subjects without diabetes got higher value only in binge eating behavior with statistical differences (t=2.11, df 128.8, p<0.05) in contrast with diabetic patients.
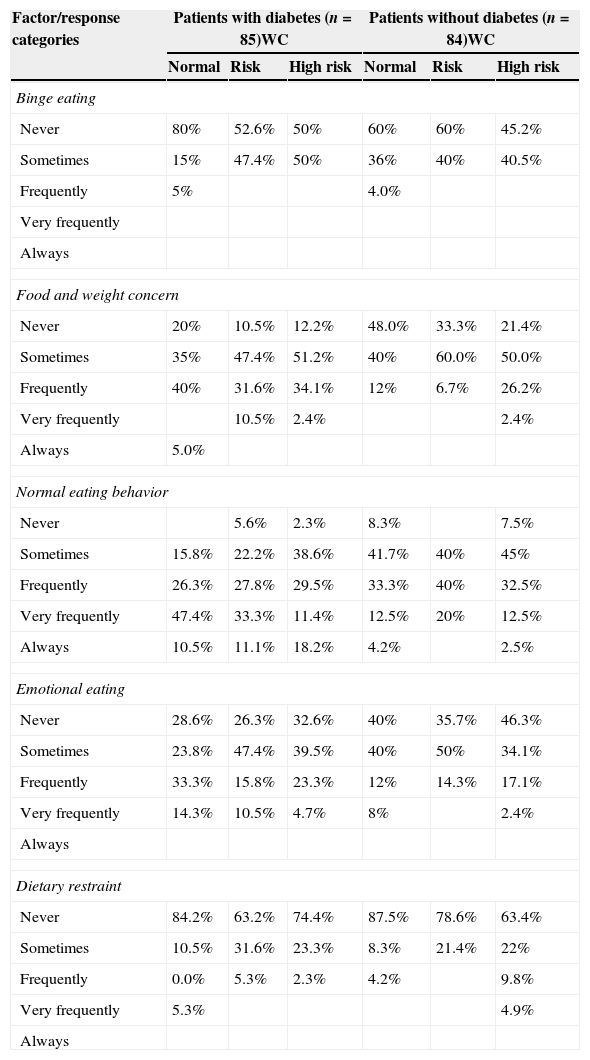
Table 4 reveals that patients with and without diabetes and with normal WC frequently have a binge eating behavior in similar percentage (5% and 4%, respectively). At the same time, patients with diabetes with normal WC reported the highest percentages for food and weight concern, for normal eating behaviors and for emotional eating. On the other side, participants without diabetes and with high risk of cardiovascular diseases reported the highest frequencies in dietary restraint in comparison with no diabetic patients.
Percentage distribution of patients with disordered eating behaviors based on diabetic status and WC.
| Factor/response categories | Patients with diabetes (n=85)WC | Patients without diabetes (n=84)WC | ||||
|---|---|---|---|---|---|---|
| Normal | Risk | High risk | Normal | Risk | High risk | |
| Binge eating | ||||||
| Never | 80% | 52.6% | 50% | 60% | 60% | 45.2% |
| Sometimes | 15% | 47.4% | 50% | 36% | 40% | 40.5% |
| Frequently | 5% | 4.0% | ||||
| Very frequently | ||||||
| Always | ||||||
| Food and weight concern | ||||||
| Never | 20% | 10.5% | 12.2% | 48.0% | 33.3% | 21.4% |
| Sometimes | 35% | 47.4% | 51.2% | 40% | 60.0% | 50.0% |
| Frequently | 40% | 31.6% | 34.1% | 12% | 6.7% | 26.2% |
| Very frequently | 10.5% | 2.4% | 2.4% | |||
| Always | 5.0% | |||||
| Normal eating behavior | ||||||
| Never | 5.6% | 2.3% | 8.3% | 7.5% | ||
| Sometimes | 15.8% | 22.2% | 38.6% | 41.7% | 40% | 45% |
| Frequently | 26.3% | 27.8% | 29.5% | 33.3% | 40% | 32.5% |
| Very frequently | 47.4% | 33.3% | 11.4% | 12.5% | 20% | 12.5% |
| Always | 10.5% | 11.1% | 18.2% | 4.2% | 2.5% | |
| Emotional eating | ||||||
| Never | 28.6% | 26.3% | 32.6% | 40% | 35.7% | 46.3% |
| Sometimes | 23.8% | 47.4% | 39.5% | 40% | 50% | 34.1% |
| Frequently | 33.3% | 15.8% | 23.3% | 12% | 14.3% | 17.1% |
| Very frequently | 14.3% | 10.5% | 4.7% | 8% | 2.4% | |
| Always | ||||||
| Dietary restraint | ||||||
| Never | 84.2% | 63.2% | 74.4% | 87.5% | 78.6% | 63.4% |
| Sometimes | 10.5% | 31.6% | 23.3% | 8.3% | 21.4% | 22% |
| Frequently | 0.0% | 5.3% | 2.3% | 4.2% | 9.8% | |
| Very frequently | 5.3% | 4.9% | ||||
| Always | ||||||
Finally, to confirm relationship between age and DEB, Spearman's correlations were carried out. Patients with diabetes showed a positive significant correlation between age and normal eating behavior (r=0.275, p<0.01). Meanwhile negative significant correlations were found between this same behavior and BMI (r=−0.270, p<0.05) and WC (r=−0.370, p<0.01). In participants without diabetes a significant correlation emerged between age and emotional eating (r=0.312, p<0.01). Regarding BMI, in patients without diabetes significant associations were identified with binge eating (r=0.245, p<0.05), food and weight concern (r=0.273, p<0.05) and dietary restraint (r=0.319, p<0.01). In this same group the DEB which achieved significant correlations with WC were over again, binge eating (r=0.224, p<0.05), food and weight concern (r=0.350, p<0.01) and dietary restraint (r=0.274, p<0.05).
DiscussionPercentage distribution of BMI was similar in patients with and without diabetes (overweight and obese) but near to 40% of women reported obesity in both groups. According to sample age, it cannot be overlooked that women may be at menopause stage, situation that in many occasions promotes body fat modification and weight gain (Lovejoy, Champagne, Jonge, Xie, & Smith, 2008).
Although some studies (Mannucci et al., 1997) reported that DEB are very frequent in patients with type 2 diabetes, mainly binge eating (Kenardy et al., 2001), our research hypothesis must be rejected, since the data of this research showed other differences between patients with and without diabetes. For example, binge eating was higher in subjects without diabetes, mainly in obese participants. This was also the case for dietary restraint. It must underline that diabetic and non-diabetic overweight subjects in the response option “frequently” (50% of the times) achieved the same percentage (2.9%) of binge eating, confirming the results of Mannucci et al. (2002) who did not find differences in the prevalence of this behavior between overweight diabetic and non-diabetic subjects, suggesting that type 2 diabetes is not a risk factor for binge eating, as well as Kenardy et al. (2001) who proposed that binge eating may be an independent risk factor to type 2 diabetes mellitus.
Nevertheless, to have identified both DEB (binge eating and dietary restraint) resulted essential, because published literature often argues that a tendency toward overeating may cause to increase food intake (mainly foods high in carbohydrates) and weight gain (Johnson, Pratt, & Wardle, 2011) and many people after a binge eating enrolls in a dietary restraint which also causes instability in weight and probably in glycemic levels. Also, certain researchers had proposed that DEB could be precursors of type 2 diabetes because not only could cause obesity but also could precede the type 2 diabetes (Khalida, 2008; Papelbaum et al., 2005).
Normal weight and overweight participants with diabetes reported most frequently having food and weight concern. This can be explained by the fact that patients with diabetes know that weight gain and diet can affect blood glucose control. For the same reason, they may be more conscious of the kinds of foods they should eat. On the other hand, diabetic patients with normal weight reported more normal eating behavior than subjects without diabetes; this event could explain that 33% of males and 24% of females reported normal BMI, higher values in contrast with non-diabetic patients (29% males, 20% females). Usually, when individuals have been diagnosed with the pathology, they change their lifestyle patterns, beginning by food intake, since that reducing energy intake with diet is the first, and probably most important therapeutic measure in the treatment of diabetes, mainly because overweight and obesity are closely linked to it (American Diabetes Association, 2008). However, the relationship between body mass index, energy balance and diabetes seems even more complex if one considers that spontaneous weight loss often occurs with poorly controlled diabetes (Weir & Bonner-Weir, 2004).
Despite more normal eating behavior was reported by the group with diabetes, the glucose and HbA1c levels of this group were above normal (152.5mg/dL and 8.5% for males; 143.4mg/dL and 8% for females), reflecting poor control. This finding could be related to high scores of emotional eating as a way of coping with the guilty and anxiety that follows poor self-control and other negative emotions caused by the diagnosis of diabetes, and worries of future development of complications (Choi, Rush, & Henry, 2013).
The significant correlation between age and normal eating behavior in patients with diabetes might be because older people want to avoid further complications associated with diabetes and therefore change to a better lifestyle. With respect to BMI and WC and its negative association with normal eating behavior, some studies have reported that irregular mealtimes increase the presence of high BMI and WC too (Newby et al., 2003).
In participants without diabetes, significant correlations were obtained (age and emotional eating, BMI with binge eating, food and weight concern and dietary restraint). These findings agree with other Mexican studies conducted with adolescents and young adults, in which data revealed a trend to present higher percentages of DEB as BMI and age increased (Saucedo-Molina & Unikel Santoncini, 2010; Saucedo-Molina, Escamilla-Talón, Portillo-Noriega, Peña-Irecta, & Calderón-Ramos, 2008; Unikel, Saucedo-Molina, Villatoro, & Fleiz, 2002).
As we know, WC is one of the best anthropometric indicators of abdominal visceral fat. Although the cause-and-effect association has not been definitively established, the available evidence indicates that visceral fat is an important link between the many facets of the metabolic syndrome: obesity, glucose intolerance, hypertension, dyslipidemia, insulin resistance, decreased HDL cholesterol concentrations and atherosclerotic cardiovascular disease (Wajchenberg, 2000). For this reason, it is relevant to point out the high percentage of participants without diabetes who fell in the high risk category according to their WC. Between them 76.1% are females and 23% are males in which other significant correlations were found with DEB (binge eating, food and weight concern and dietary restraint). These findings allow to propose that, if these subjects did not modify their eating behaviors, lose weight, and in general change their lifestyle they would soon be patients with type 2 diabetes, not only because the excess of visceral abdominal fat and high BMI are associated with this disease, but also because DEB have been proposed as a precursor of the pathology (Kenardy et al., 2001; Khalida, 2008; Papelbaum et al., 2005).
ConclusionThe results obtained demonstrate the need to continue working in this field on the Mexican population, in which type 2 diabetes mellitus is a major public health problem (Hernández-Ávila et al., 2013; Olaiz-Fernández et al., 2006; Gutiérrez et al., 2012).
Through these findings, it is possible to identify potential shortcomings (DEB is often overlooked in diabetes education counseling sessions) and beneficial factors to propose strategies that encourage healthy eating and lifestyle behaviors, both in patients with and without diabetes. For example, it will be possible to tailor counseling sessions to include psychotherapy, by a certified therapist, to address the emotional and psychological well-being of patients with diabetes, or of patients with and without diabetes who are overweight, obese or have a large WC. It will also be possible to include discussion on psychological issues during individual consultations and during group counseling sessions with a multidisciplinary team (nutritionist, nurses, doctors and psychotherapists) with patients with diabetes or patients who are overweight, obese or have a large WC.
The current study has limitations. First, due to the cross-sectional study design, causal relationships cannot be established. Second, the findings cannot be generalized to Hidalgo State's population because the study was not carried out with a probabilistic sample of subjects with and without diabetes. Another limitation of this study is the lack of information about the type and frequency of physical activity, on medication (e.g. meglitinides and sulfonylureas, biguanides, α-glucosidase inhibitors, thiazolidinediones), or nutritional supplements taken by the participants that can affect mood or eating behaviors (e.g. antidepressants, anxiolytics or appetite suppressants). Finally, the evolution and chronicity of the diabetes were not identified in the sample. Regardless of these limitations, the contributions of this research are important because it is the first study of this kind in Hidalgo State and it has led to a new perspective in type 2 diabetes.
Sources of supportThis work was supported by the Faculté des études supérieures et de la recherche, Université de Moncton, Canada.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestThe authors declare no conflict of interest.
We thank the participants in this study and the research assistant Lidiana Tavares Almeida, Master student at Université de Moncton in Canada, who conducted the data collection. Appreciation is also extended to the Faculty of Graduate Studies and the International Mobility Service, Université de Moncton, for research funds and mobility scholarship for Lidiana Tavares Almeida. We also thank PhD Gilda Gómez Pérez-Mitré for allowing us to use the EFRATA.
Peer Review under the responsibility of Universidad Nacional Autónoma de México.