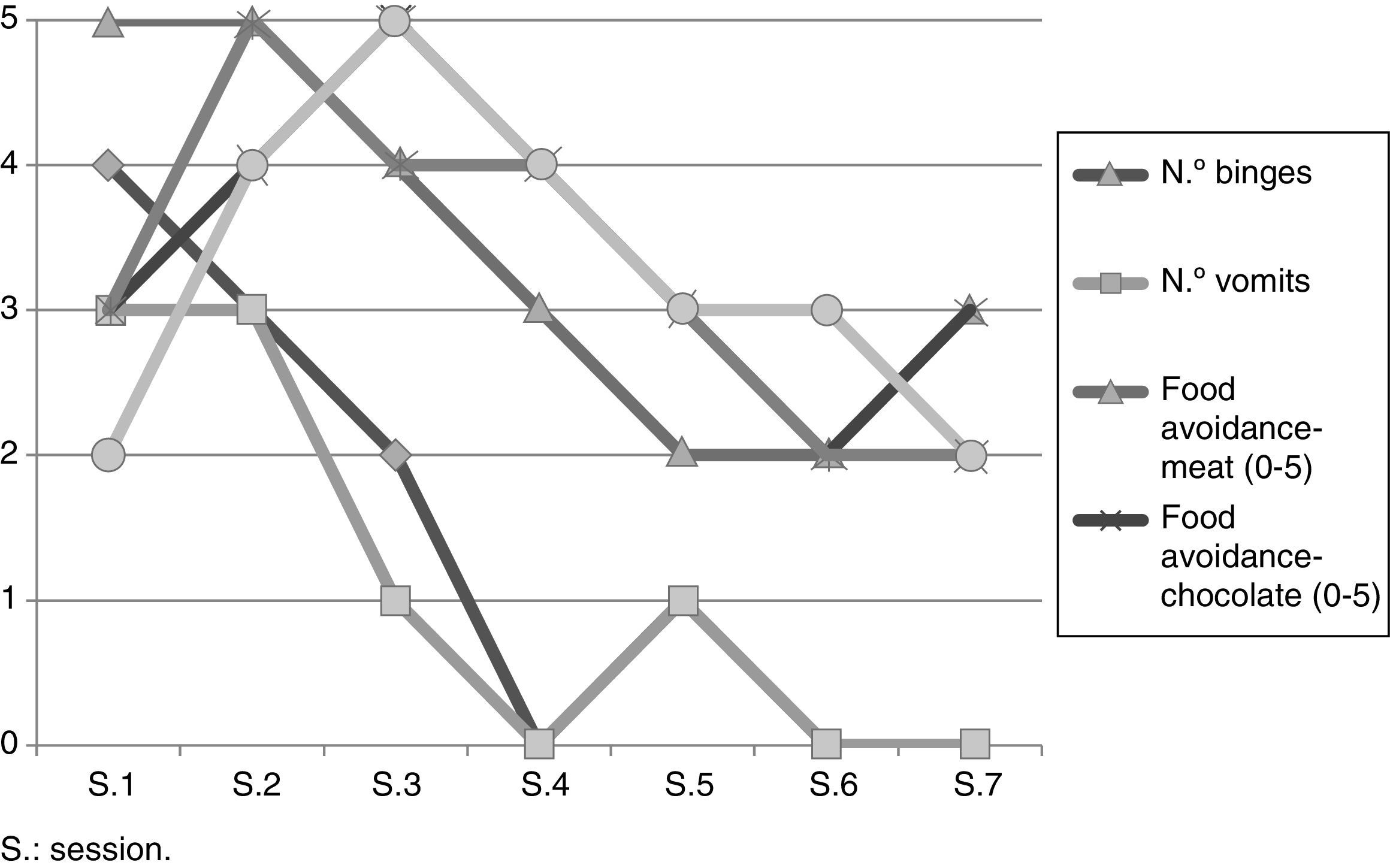
The aim of the present study was to analyze the effects of a virtual reality (VR) component as a therapeutic tool to normalize eating patterns, as part of the cognitive-behavioral treatment of a bulimia nervosa (BN) patient. Results indicated that the patient made significant progress with her eating habits; binges and vomits were eliminated completely. Moreover, when the VR started the patient avoided food, especially meat (5 over 5), and it was reduction of this avoidance in the lasts sessions (2 and 3 over 5). It was also observed a reduction in the avoidance and the fear of eating (from 10 and 9 to 6 and 5 respectively) and increased the impulse control (from 2 to 7). The patient felt that the VR experience seemed real and similar to reality (mean score of 8.3 over 10). Before and after the seven VR sessions, there was a decrease in the drive for thinness, bulimia, ineffectiveness, and BITE symptoms and severity, and in the general psychopathology. Moreover, the patient improved her motivation to change. Results suggest that VR is a relevant and effective complement to traditional treatment in a BN patient. Further studies should continue this line of research by using larger sample sizes with different diagnoses and subtypes and control groups.
El objetivo del presente estudio fue analizar el efecto de un componente de realidad virtual (RV) como una herramienta de terapia para la normalización de la ingesta, como parte de un tratamiento cognitivo conductual para la bulimia nerviosa (BN). Después de un módulo de 7 sesiones de RV, la paciente tuvo un progreso significativo en sus hábitos alimentarios. Los atracones y vómitos se eliminaron completamente. Además, al inicio de las sesiones, la paciente evitaba la comida, especialmente la carne (5 sobre 5), observándose una reducción de la evitación en las últimas sesiones (2 y 3 sobre 5). También se redujeron la evitación y el miedo a comer (de 10 y 9 a 6 y 5, respectivamente) y aumentó el control del impulso (de 2 a 7). La paciente sintió como real la experiencia virtual y fue evaluada como similar a lo que experimenta en la vida real (puntuación media de 8,3 sobre 10). Después de las 7 sesiones de RV, hubo una reducción en el impulso por adelgazar, bulimia, ineficacia, en los síntomas y la gravedad del BITE, y en la psicopatología general. Además, la motivación al cambio mejoró en la paciente. Los resultados indican que la RV es un complemento relevante y efectivo en el tratamiento tradicional en una paciente con BN. Se requieren futuros estudios en esta línea muestras más amplias con diferentes diagnósticos y subtipos y grupo control.
In the past 20 years, there has been increasing interest in the use of virtual reality (VR), a computational technology, in the mental health area. Virtual environments have been created for clinical use to expose patients to their fears (Bush, 2008). This technology allows clinicians to create a safe environment that can be customized and adapted to each patient under the strict supervision of the therapist (Wiederhold et al., 2002). VR is supposed to be a prior step to in vivo exposure (Riva, 2009), but it is less likely to be rejected by the patient (Olatunji, Cisler, & Deacon, 2010).
Regarding the treatment of eating disorders (ED), the most widely-accepted form of psychotherapy, mainly for bulimia nervosa and binge eating disorder, is cognitive-behavioral therapy (CBT; NIMH, 2014). In CBT, patients are trained to change their patterns of thinking and behaving to prepare them to face their fears. However, in spite of the progress being made, the severity, the tendency toward chronicity, and the complications observed in these disorders show that we still do not have any treatments that are completely capable of dealing with their complexity (Wilson, 2010; Villarejo et al., 2012). One of the many difficulties for patients lies in stabilizing their eating patterns in order to achieve weight regulation and start the cognitive work about the implications of food-related beliefs. Therapeutic tools such as VR components may be effective in optimizing these therapeutic strategies (Hart, Abraham, Franklin, & Russell, 2011).
VR has mainly been applied in the evaluation and treatment of body image disturbances (Cesa et al., 2013; Gutiérrez-Maldonado, Ferrer-García, Caqueo-Urízar, & Moreno, 2010; Marco, Perpiñá, & Botella, 2013; Perpiñá et al., 1999; Perpiñá, Marco, Botella, & Baños, 2004; Riva, Bacchetta, Baruffi, Rinaldi, & Molinari, 1999; Riva et al., 2000; Riva, 2011), with satisfactory results not only in the case of body image, but also on psychopathology-related indices. However, recently some studies have shown that exposure to virtual food produces the same sensations as exposure to real food in non-immersive and immersive environments (Ferrer-García, Gutiérrez-Maldonado, Caqueo-Urízar, & Moreno, 2009; Ferrer-Garcia, Gutierrez-Maldonado, Treasure, Vilalta-Abella, 2015; Ferrer-Garcia et al., 2014; Gorini, Griez, Petrova, & Riva, 2010). Thus, the next step in the use of VR for the treatment of ED was to test virtual environments (VE) as a therapeutic tool in another essential aspect of the treatment of ED patients: normalizing eating patterns. A validated non-immersive Virtual Environment with a virtual kitchen (Perpiñá et al., 2013) has been used in two clinical cases with positive results. In both cases, one patient with anorexia nervosa-restrictive type and another with anorexia nervosa-purgative type, this VE was used to provide graded exposure to feared foods as an add-on to their respective treatments (Maudsley Model of treatment for adults with anorexia nervosa and cognitive behavioral treatment, respectively). Results showed that both patients normalized their eating patterns and introduced avoided foods into their real daily intakes. In the patient with anorexia nervosa-restrictive type, the anxiety level and fears related to food were reduced, as were binges and vomiting in the anorexia nervosa-purgative type. Moreover, their ED symptoms were reduced, and their body mass index increased significantly (Cardi, Krug, Perpiñá, Mataix-Cols, Roncero, & Treasure, 2011; Perpiñá, Ferrero, Carrió, & Roncero, 2012).
In the case of bulimia nervosa (BN), in previous studies VR has been used as a tool to improve body image and reduce the craving to binge. However, as far as we know, there are no data on the use of VR to normalize eating. VEs are expected to help to normalize the eating pattern and treat emotional eating, as in the case of anorexia nervosa patients. Thus, the aim of the present study was to analyze the effects of a VR component as a therapeutic tool to normalize eating patterns, as part of the cognitive-behavioral treatment for a BN patient.
Case illustrationPatient identificationB was a 17-year-old woman with a body mass index of 22.2. She was single and living with her parents and an older brother and older sister. B was enrolled in the last year of high school. She wanted to start university studies the following year. She had a medium socio-economic level.
Reason for the consultationB asked for treatment, but was pushed by her mother. She was not sure she had a problem, but she complained about her frequent intrusive thoughts about food, and she wanted to eliminate the binges and vomiting. She recognized that her eating habits were not healthy. She was having 3-4 binges followed by vomiting per week, and she described strong feelings of guilt, shame and disgust. She also had a sense of losing control. She was not satisfied with her weight, and she wanted to lose at least 8kg in order to reach a weight of 55kg. This was her objective because at that weight (when she was 16 years old) she felt nice and proud of herself, “people use to tell me how nice I looked”. B had low insight about the disorder.
She did not present any physical alterations, except a slight Russell's sign on her right hand, and there was no swelling of the parotid glands. Her blood count and biochemical analyses were normal. At a cognitive level, B complained that her thoughts about food did not allow her to concentrate on other things, but her academic performance was not impaired. The patient presented depression and anxiety symptoms. She spent the day at school and the evening studying at home. B was very motivated to obtain high grades. She wanted to earn a medical degree and was encouraged by her mother, who was a nurse.
History of the problemB has one brother – 6 years older, and a sister – 3 years older. Her brother, sister and mother were all overweight. When she was 14, she began to worry about becoming overweight like them. At 15 years old, B started to follow restrictive diets, and she lost 6kg in 6 months. Her family would tell her that she had to eat more because she was very thin and looked disgusting, but she thought they were envious of her. Soon she started binging, followed by vomiting, once a week, and the binges and vomiting had increased in number to 3-4 per week in the previous 6 months, approximately. The patient's mother sought help at the local Mental Health Care Unit.
Assessment and diagnosisThe patient was diagnosed by her clinician in the outpatient mental-health center using the Structured Clinical Interview for DSM-IV-TR. In a second session, B was asked to complete a set of self-reports, listed below, at baseline and after the 7 sessions of VR. This study received the approval of the Ethics Committees of the University of Valencia and the outpatient mental-health center. Before completing the protocol, the patient signed an informed consent form.
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996). This self-report evaluates the presence and severity of depressive symptoms. It consists of 21 items rated on a 4-point Likert scale (from 0 to 3). Psychometric properties of the Spanish version are adequate (Cronbach's alpha of 0.89; Sanz, Perdigón, & Vázquez, 2003).
Beck Anxiety Inventory (BAI; Beck & Steer, 1993). This self-report evaluates the severity of anxiety somatic symptoms with 21 items, using a 4-point Likert scale (from 0 to 3). For the present study, the Spanish version of Comeche, Diaz and Vallejo (1995) was used, which has shown satisfactory psychometric properties (Cronbach's alpha of 0.88).
Eating Disorders Inventory-II (EDI-II; Garner, 1991; Spanish version: Corral, González, Pereña, & Seisdedos, 1998). This inventory consists of 91 items grouped in 11 sub-scales that evaluate attitudes, behaviors, and more general aspects associated with ED: Drive for thinness, bulimia, body dissatisfaction, ineffectiveness, perfectionism, interpersonal distrust, interoceptive awareness, maturity fears, asceticism, impulse regulation and social insecurity. The psychometric properties in Spanish population are satisfactory (Cronbach's alpha range from 0.83 to 0.92, except for maturity fears=0.65).
Attitudes Toward Change in eating disorders (ACTA; Beato-Fernández & Rodriguez-Cano, 2003). This self-report evaluates ED patients’ attitudes toward change, following the Prochasca and DiClemente trans-theoretical model. It consists of 59 items, rated from 1 “never” to 5 “always”, and grouped in 6 sub-scales: pre-contemplation, contemplation, decision, action, maintenance and relapse. In the present study, the last two factors were not included because they were not relevant to the patient's situation. The psychometric properties in the original study with a Spanish population are satisfactory (Cronbach's alpha range from 0.74 to 0.90).
Bulimic Investigatory Test, Edinburgh (BITE; Henderson & Freeman, 1987; Spanish version: Rivas, Bersabé, & Jiménez, 2004). This 33-item self-report was designed to evaluate bulimic and binge-eating symptoms. The instrument has two sub-scales: a severity scale that evaluates the presence of symptoms, and a severity scale that measures the severity of binges and purges based on the frequency. The Spanish validation has shown satisfactory psychometric properties (Cronbach's alpha for symptoms: 0.96 and 0.62 for severity).
Regarding the measures to control the outcome of the virtual reality component, the patient filled out the following questionnaires:
Ad-hoc intra-session questionnaire. During the virtual experience, the patient was asked, using a Likert format (0: not at all–10: absolutely), about the experience of virtual eating before and after eating: emotions (well-being, fear, nervousness, guilt, and discomfort), how appetizing it was, her control over the urge to eat it, and the desire to avoid the food.
Weekly evaluation. Between VR sessions, the patient was asked to report the number of binges and purges. She also had to rate from 0 (“nothing”) to 10 (“extremely”) to what extent she had avoided food, and the degree of interference the disorder caused in her daily activities.
At the time of the assessment, B met the DSM-IV (APA, 2000) criteria for Bulimia Nervosa (BN) purgative subtype. Based on the DSM-5 (2013), she would have met the criteria for BN with mild-moderate severity.
Treatment interventionB received Fairburn's Cognitive-Behavioral Therapy (CBT) for BN (see Fairburn, Marcus, & Wilson, 1993 for detailed description) at her corresponding national health outpatient service. Due to her low insight and motivation to change, the decision was made to include a VR module containing seven sessions, parallel to Phases I and II of the CBT sessions. The purpose of this first stage of CBT is to normalize the eating pattern, and this would also be the main objective of the VR sessions. In the VR sessions, the patient would practice the issues introduced in the CBT sessions in order to regain control over food, practice healthy eating habits (enjoy meals, always eat in the same place, etc.), and plan meals by controlling stimuli to avoid binges. Then, in Phase II, the patient would gradually be exposed to forbidden food, practice alternative behaviors, and replace negative thoughts with positive self-instructions.
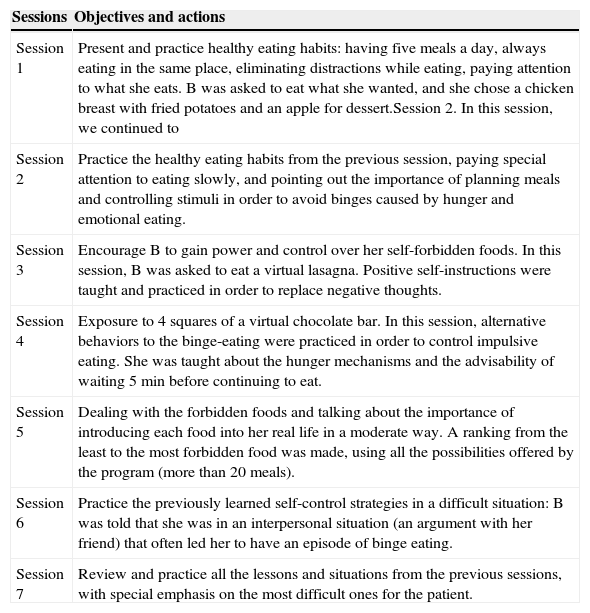
A total of seven VR sessions were included in this therapy module. The sessions were designed for patients with BN, specifically to be used with Fairburn's CBT. They lasted approximately 60min each, and there was an interval of one/two weeks between sessions. Sessions had specific objectives and contents, described in Table 1.
Description of sessions.
| Sessions | Objectives and actions |
|---|---|
| Session 1 | Present and practice healthy eating habits: having five meals a day, always eating in the same place, eliminating distractions while eating, paying attention to what she eats. B was asked to eat what she wanted, and she chose a chicken breast with fried potatoes and an apple for dessert.Session 2. In this session, we continued to |
| Session 2 | Practice the healthy eating habits from the previous session, paying special attention to eating slowly, and pointing out the importance of planning meals and controlling stimuli in order to avoid binges caused by hunger and emotional eating. |
| Session 3 | Encourage B to gain power and control over her self-forbidden foods. In this session, B was asked to eat a virtual lasagna. Positive self-instructions were taught and practiced in order to replace negative thoughts. |
| Session 4 | Exposure to 4 squares of a virtual chocolate bar. In this session, alternative behaviors to the binge-eating were practiced in order to control impulsive eating. She was taught about the hunger mechanisms and the advisability of waiting 5min before continuing to eat. |
| Session 5 | Dealing with the forbidden foods and talking about the importance of introducing each food into her real life in a moderate way. A ranking from the least to the most forbidden food was made, using all the possibilities offered by the program (more than 20 meals). |
| Session 6 | Practice the previously learned self-control strategies in a difficult situation: B was told that she was in an interpersonal situation (an argument with her friend) that often led her to have an episode of binge eating. |
| Session 7 | Review and practice all the lessons and situations from the previous sessions, with special emphasis on the most difficult ones for the patient. |
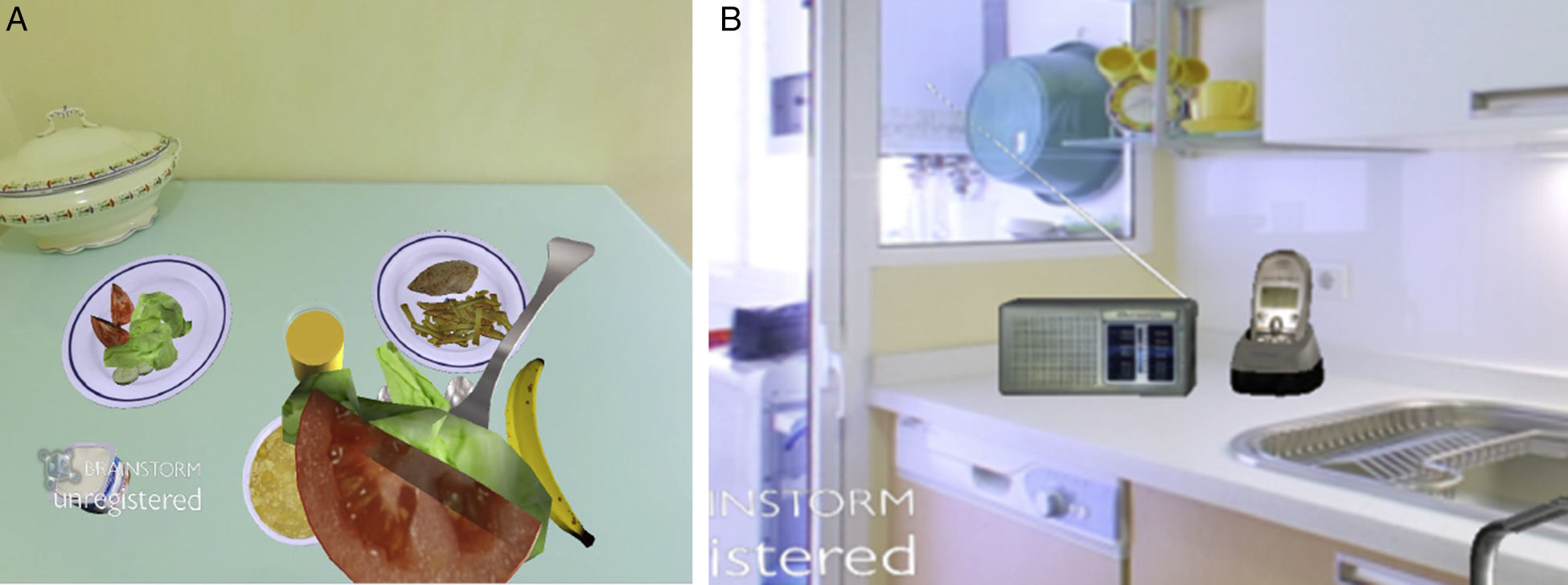
The non-immersive virtual environment consists of a kitchen with two areas that contain all the necessary elements to cook, drink and eat: countertop, cabinets, stove, fridge, table, and chair (see Fig. 1). The foods are located in the fridge, cabinets and shelves, and the patient can access them freely or block them if desired. The eating style can be set at fast or slow. The size of certain foods (chocolate, potatoes, pizza, etc.) can be increased (occupying the entire screen) or decreased (until vanishing). Alternative behaviors can be performed, such as making a phone call or listening to music. In addition, negative and positive thoughts can be addressed, and training is given in positive self-instructions. As reinforcement, the software allows the therapist to show positive or negative consequences of the decision or behavior that the patient has just displayed (image of happy vs. sad body organs).
The VE was displayed on a 3-GHz Pentium V laptop with 1 GB RAM, a 256Mb graphic card, a 19-in. monitor and a 2D mouse. The patient was comfortably seated in front of the monitor-screen, located at a distance of 50cm, next to the clinician, and in a dimly lit room.
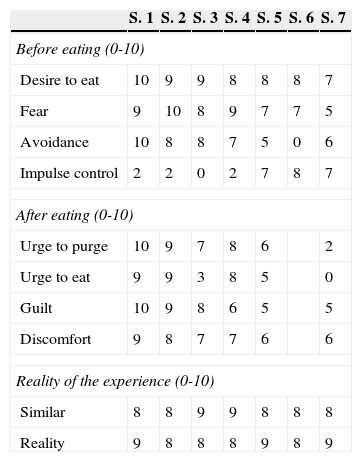
ResultsThroughout the VR sessions, it could be observed that, before eating virtually, the desire to eat was quite high and stable over the weeks; however, the fear and avoidance decreased, and the impulse control increased (see Table 2). It is also noteworthy that after the virtual eating, the urge to purge and eat and the negative consequences gradually decreased. Regarding the evaluation of the sense of presence, during the seven sessions, the patient felt that the VR experience seemed real and similar to reality.
Data collected during the virtual session.
| S. 1 | S. 2 | S. 3 | S. 4 | S. 5 | S. 6 | S. 7 | |
|---|---|---|---|---|---|---|---|
| Before eating (0-10) | |||||||
| Desire to eat | 10 | 9 | 9 | 8 | 8 | 8 | 7 |
| Fear | 9 | 10 | 8 | 9 | 7 | 7 | 5 |
| Avoidance | 10 | 8 | 8 | 7 | 5 | 0 | 6 |
| Impulse control | 2 | 2 | 0 | 2 | 7 | 8 | 7 |
| After eating (0-10) | |||||||
| Urge to purge | 10 | 9 | 7 | 8 | 6 | 2 | |
| Urge to eat | 9 | 9 | 3 | 8 | 5 | 0 | |
| Guilt | 10 | 9 | 8 | 6 | 5 | 5 | |
| Discomfort | 9 | 8 | 7 | 7 | 6 | 6 | |
| Reality of the experience (0-10) | |||||||
| Similar | 8 | 8 | 9 | 9 | 8 | 8 | 8 |
| Reality | 9 | 8 | 8 | 8 | 9 | 8 | 9 |
Note: S.=session.
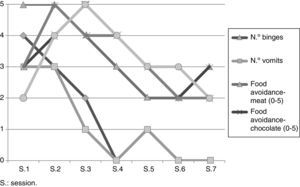
Fig. 2 shows the weekly inter-session evaluations. In her daily life, B made significant progress with her eating habits, experiencing a gradual decrease in binges, vomiting and food avoidance. There was also a noteworthy decrease in the interference caused by the disorder. B was very aware of the VR in her day-to-day life, which was demonstrated by comments such as: “Every time I eat, I see myself in the VR kitchen eating slowly and enjoying each bite”; “when the thought of binging comes to my mind, I remember you (her therapist) in the VR telling me to take control of the food and make the size of the chocolate bar smaller and smaller, so that it loses its power over me”.
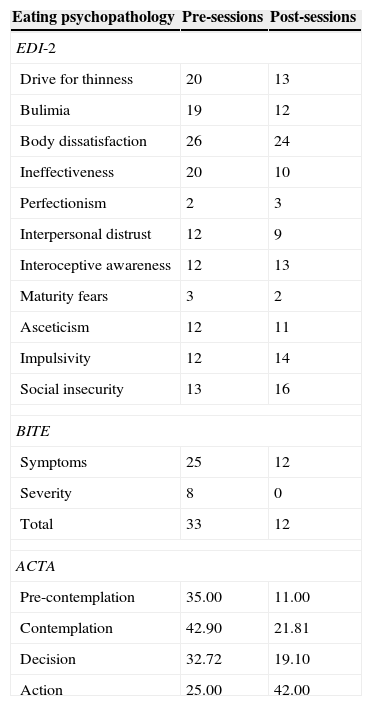
The comparison of the psychopathology measures taken before and after the seven VR sessions showed a general improvement. There was a noteworthy decrease in the drive for thinness, bulimia, ineffectiveness, and BITE symptoms and severity. Regarding the motivation to change, B was mainly in the contemplation and relapse stages in the pre-sessions, and in the action stage at the end of the VR sessions. The general psychopathology also decreased (see Table 3).
Eating and general psychopathology measures pre- and post-VR sessions.
| Eating psychopathology | Pre-sessions | Post-sessions |
|---|---|---|
| EDI-2 | ||
| Drive for thinness | 20 | 13 |
| Bulimia | 19 | 12 |
| Body dissatisfaction | 26 | 24 |
| Ineffectiveness | 20 | 10 |
| Perfectionism | 2 | 3 |
| Interpersonal distrust | 12 | 9 |
| Interoceptive awareness | 12 | 13 |
| Maturity fears | 3 | 2 |
| Asceticism | 12 | 11 |
| Impulsivity | 12 | 14 |
| Social insecurity | 13 | 16 |
| BITE | ||
| Symptoms | 25 | 12 |
| Severity | 8 | 0 |
| Total | 33 | 12 |
| ACTA | ||
| Pre-contemplation | 35.00 | 11.00 |
| Contemplation | 42.90 | 21.81 |
| Decision | 32.72 | 19.10 |
| Action | 25.00 | 42.00 |
| General psychopathology | Pre-sessions | Post-sessions |
|---|---|---|
| BDI-II | 32 | 18 |
| BAI | 38 | 24 |
EDI-2: Eating Disorder Inventory; BITE: ACTA: Attitudes Toward Change in eating disorders; BDI-II: Beck Depression Inventory-II; BAI: Beck Anxiety Inventory.
The main objective of this study was to analyze the effect of a VR component as a therapeutic tool to normalize eating patterns, as part of the cognitive-behavioral treatment for a BN patient. Results of this case study indicated that VR had a positive effect on her eating habits. The patient showed a reduction in binges, purges and food avoidance, and more importantly, the disorder's interference in her life also decreased.
Regarding the VR experience, B demonstrated a gradual improvement in her control over the urge to binge and purge after virtually eating food, even though the desire to eat was stable and high across sessions. It is noteworthy that the similarity to real life and the sense of reality felt by the patient was very high from the first session on. Her feeling of presence and the attribution of reality were probably due to the relevance and clinical significance of the virtual environment in her disorder, making the environment emotionally significant for her. This effect has been observed when comparing the VR exposure of clinical and non-clinical individuals to relevant virtual environments designed for their disorders (Perpiñá, Botella, & Baños, 2003; Perpiñá et al., 2013). In turn, this sense of reality helps patients to generalize the VR treatment to real life (Botella et al., 2004). B stated that the VR sessions helped her to create a visual image of herself as successful in controlling the impulse to binge and vomit. At the end of the sessions, B also introduced more healthy foods that she had avoided for years into her real diet, such as red meat. The most important achievement for her was that she managed to eat a piece of chocolate cake, which scared her because she was not confident that she could control the impulse to eat the entire cake. In fact, in the first VR session, B told the therapist that she would not eat the virtual chocolate cake. However, as the sessions progressed, B felt more confident, making it possible to work with her emotions, thoughts and fears in a secure environment at the precise moment of eating a highly feared food. Again, VR functioned as a previous step to real life, as occurred when using VR in other ED diagnoses, such as anorexia nervosa restrictive and purgative subtypes (Cardi et al., 2011; Perpiñá et al., 2012). As Pla-Sanjuanelo et al. (2015) stated, by simulating real-world environments where binging occurs, virtual reality exposure therapy achieves greater ecological validity than in vivo exposure conducted in the therapist's office.
There was also a noticeable improvement in the ED symptoms when comparing the pre- and post-VR sessions, especially in the drive for thinness, bulimia, and ineffectiveness factors of the EDI-II, and in the severity of the BN measured by the BITE. One of the most remarkable results was the change in the motivational stage of the patient before and after the seven VR sessions. The pre-VR evaluation showed that B was mainly in a Contemplation stage, i.e. she began to consider that she had a problem but did not have the determination to correct it. However, at the post-VR evaluation, B was clearly positioned in the Action stage, where the patient experiences a change in three areas: cognitive, with positive thoughts about change; behavioral, with changes in her habits; and affective, where the disorder is perceived as unpleasant (Beato-Fernández & Rodriguez-Cano, 2003). This result demonstrates – once again – the positive effect of VR on self-efficacy and motivation to change (Riva et al., 1999). This is especially relevant in ED because patients’ ambivalence makes them reluctant to receive treatment, and the attrition rate is very high.
The present study, although consisting of a single case report, takes another step in the study of the efficacy of the use of a VR component in the general treatment for normalizing the ED eating pattern. As mentioned above, the virtual food seems to have the same emotional impact on ED patients. Because VR seems capable of producing anxiety and food avoidance and the awakening of the urge to eat, opportunities arise to design components to prevent and manage binging and emotional eating in ED patients, not only for use in treatments, but also to construct efficient virtual labs for studying eating behavior.
In sum, our results suggest that the VE was a relevant and effective complement to traditional CBT treatment in a BN patient. However, without control groups it is not possible to affirm to what extent the benefits are due to the VR component or to the CBT. Moreover, we have no data about the follow-up. Further studies should continue this line of research by using larger sample sizes with different diagnoses and control groups, in order to compare differences in the reactions to and results of the VR component in the clinical setting, and their generalization to real life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare no conflict of interest.
Supported by the Spanish Ministerio de Sanidad (FIS-PI051937), Conselleria de Sanidad (SMI 3/2008), and Conselleria d’Educació, Cultura i Esport, Generalitat Valenciana (PROMETEO/2013/066). Centro de Investigación Biomédica en Red Fisiopatología de la Obesidad y Nutrición, initiative of ISCIII. Gobierno de Aragón (dpto. de industria e innovación). Fondo Social Europeo.
Peer Review under the responsibility of Universidad Nacional Autónoma de México.