Retained third molars are teeth linked to several conditions of the mouth, therefore, in most cases, surgical extraction is required. Surgical procedures undertaken to extract retained third molars bring about surgical procedures effects. The aim of the present study was to determine healing effectiveness in bone and gingival tissue with use of platelet rich fibrin in surgical procedures involving lower third molar extraction performed at the Surgical Center of the School of Dentistry, Central University of Ecuador in the period comprised May-September 2015. A comparative study was performed of 30 patients meeting inclusion criteria. Eight days after extraction, patients were controlled by means of direct observation of surgical site; 60 days after extraction, a digital panoramic X-ray of the jaws was taken and analyzed with software RadiAnt DICOM Viewer. For soft tissue, healing results were obtained with χ2 test p < 0.001, and for bone tissue results were obtained with t-Student test p = 0.015.
Los terceros molares retenidos son dientes que se encuentran ligados a una serie de patologías en la cavidad bucal, por lo que se requiere su extracción quirúrgica en la mayoría de los casos. Los procedimientos quirúrgicos para extraer terceros molares retenidos, traen consigo efectos propios de la cirugía. El objetivo de este estudio fue determinar la efectividad cicatrizante en tejido óseo y gingival con el uso de la fibrina rica en plaquetas en la cirugía de terceros molares inferiores en el Centro Quirúrgico de la Facultad de Odontología de la Universidad Central del Ecuador en el periodo de mayo-septiembre del 2015, mediante un estudio comparativo realizado en 30 pacientes que cumplieron los criterios de inclusión. Se controló a los pacientes a los ocho días mediante observación directa de las heridas, y a los 60 días posteriores a la intervención quirúrgica una toma radiográfica panorámica digital de maxilares, analizada en el software RadiAnt DICOM Viewer. Los resultados obtenidos en cicatrización de tejido blando fueron mediante la prueba de χ2 p < 0.001 y para tejido óseo mediante la prueba t de Student p = 0.015.
Third molars are teeth most frequently found included. Lower first molars are most frequent, followed by upper first molars.1 Third molar extraction is one of the most common procedures in dentistry.2 Reasons for third molar extraction are varied, ranging from prophylactic measures to patients exhibiting large osteolytic lesions related to third molars.3
Extraction of impacted third molars causes surgery-related effects which represent great patient discomfort, such as pain after surgery, inflammation in the following 24 to 72hours, trismus (lockjaw) suffered due to muscle contraction. «Extraction of third molars has an effect over the periodontal state of the lower second molar. Prevalence of periodontal disease in second molars is 77% before surgery, and 23% after surgical intervention».4 Moreover, pain and post surgical inflammation are intimately linked to the type of surgical wound regeneration and healing (scarring).2
Healing of a socket after extraction, in cases when no filling materials have been used is effected through second intention.5 This healing takes place in three phases: first the inflammatory phase, followed by proliferative phase to end with remodeling.6 Two types of healing are known in dentistry: healing by first intention and by second intention. First intention healing is achieved with use of sutures, second intention healing is effected with spontaneous closing of the surgical wound.7
Tissue preparation of injured tissues in surgery to achieve healing is an important aspect of any surgical procedure, therefore, it is valuable for dental professionals to conduct this type of procedure and be knowledgeable in all aspects of normal tissue repair biology.8
Platelet concentrates have been in use for many years to improve postsurgical circumstances in cases of impacted third molar extractions. These concentrates are obtained from human blood, and subjected to a centrifuging process following different techniques for their procurement.
Dohan et al,9 in their study, report that platelet rich fibrin is a second generation platelet concentrate. Fibrin is a plasmatic fibrinogen active molecule10 which together with platelets improves and accelerates tissue hemostasis and healing.11
Platelet rich fibrin is used to improve processes of bone and gingival tissue neo-formation.12 Bone tissue healing is dictated by intracellular and extracellular processes. Platelets play a fundamental role in wound healing, by forming blood clots and releasing growth factors.13 Its use is based on accelerating healing processes of both soft and hard tissues. Due to its procurement technique, it possesses certain advantages when compared to platelet rich plasma (PRP).
The present study is of a descriptive nature, where evaluation was made of healing in bone and gingival tissue either with or without use of platelet rich fibrin, used as autologous and adjuvant product for healing of wounds inflicted during lower impacted third molar surgery, to thus improve patients’ recovery in a costeffective manner without causing adverse reactions.
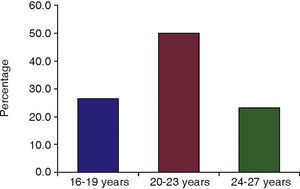
MATERIAL AND METHODSPatient selectionFor the present study, 30 female and male patients were selected, ages ranging 16-27 years, divided into three groups of 16-19, 20-23 and 24-27 years. Patients had undergone impacted lower third molar extraction surgery. The aforementioned age ranges were selected due to the fact that at this age patients attend more frequently the clinic for third molar extraction, because of the complications these impactions cause them. Extracted third molars were in the following positions: mesial angle, distal angle, horizontal, transversal and vertical. Type and class of position were not taken into account according to Pell & Gregory classification. Patients excluded from the study were those who exhibited alterations in platelet recount values, clotting times, hemorrhage time, prothrombin time, thromboplastin partial time, pregnant and nursing patients, patients with underlying systemic alterations, alcoholics, as well as drug and tobacco addicted patients. Patients were treated at the Surgical Center of the School of Dentistry, Central University, Ecuador. All patients were previously informed about the study and signed informed consent waivers.
Study designPlatelet rich fibrin meshes were placed in the socket corresponding to the extracted lower left third molar in order to compare it to the right lower third molar socket which had received no biological material or substance after extraction, the site had only received simple stitch suture points performed with vicryl 3-0 (Ethicon, Johnson and Johnson). Patients were prescribed amoxicillin + clavulanic acid, 875/125 every 12hours and ketorolac, 10mg every 8hours, ingested by mouth. This medication was selected in order to avoid interaction in inflammation and healing processes. Inflammation was controlled with local means such as local ice and damp heat. Wounds were inspected after eight days; 60 days after surgery a digital panoramic radiograph was taken.
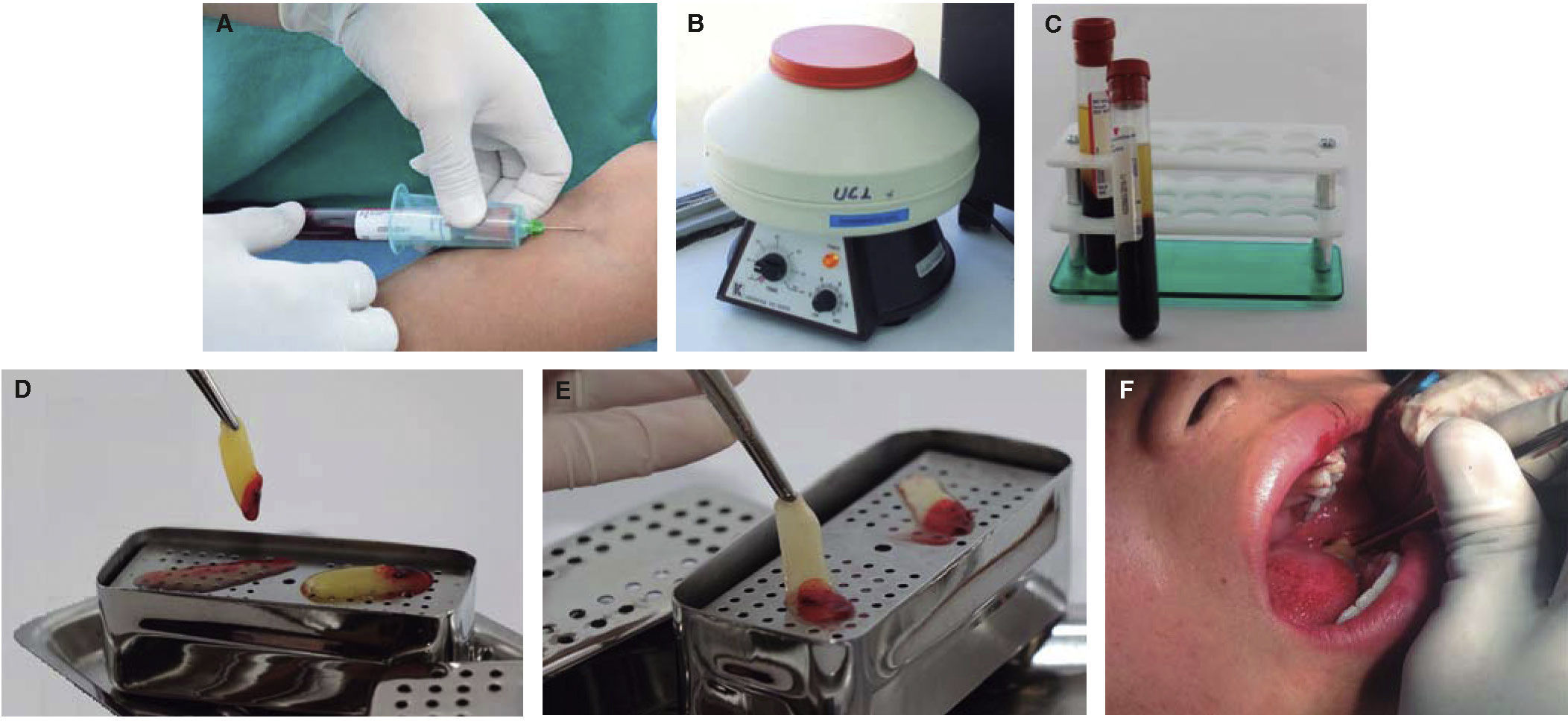
PRF procurementBefore surgical extraction, two 10mL blood samples were harvested and placed in tubes (BD Vacutainer), to be both placed in a 3,000rpm centrifuge appliance during 10minutes15 (centrifuge PLC series). No anticlotting substance was added. The product of the centrifuge process was taken to a tray in order to separate serum from fibrin during one minute. Finally, the fibrin platelet-rich mesh was placed in the socket after the extraction of lower left third molar (Figure 1).
Process of PRF procuration and placement. A) Procuration of blood sample. B) Placement of tubes in centrifuge device. C) Centrifuged tubes after established time. D) Plasma filtering and fibrin modeling. E) Final result of platelet rich fibrin (PRF). F) Placement of PRF in the socket left lower molar socket.
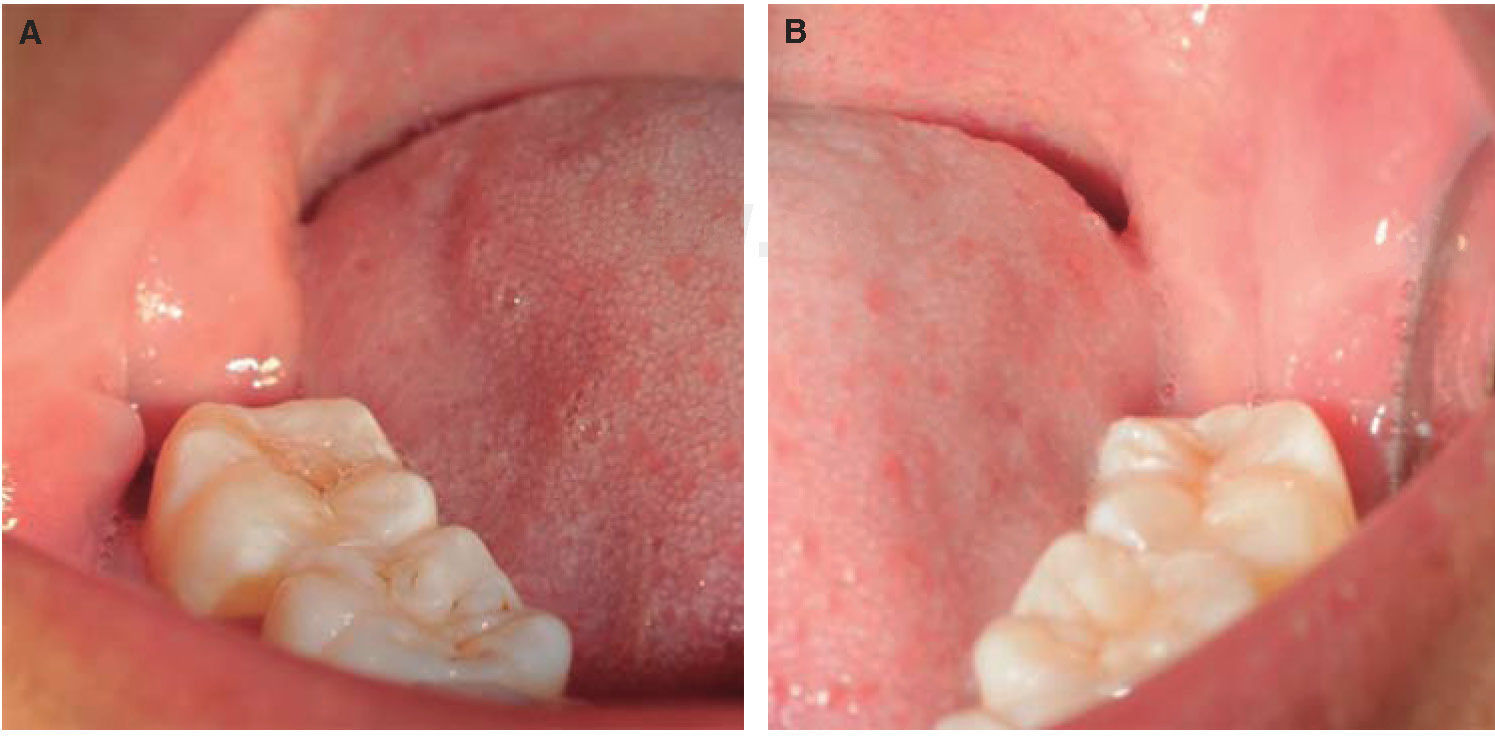
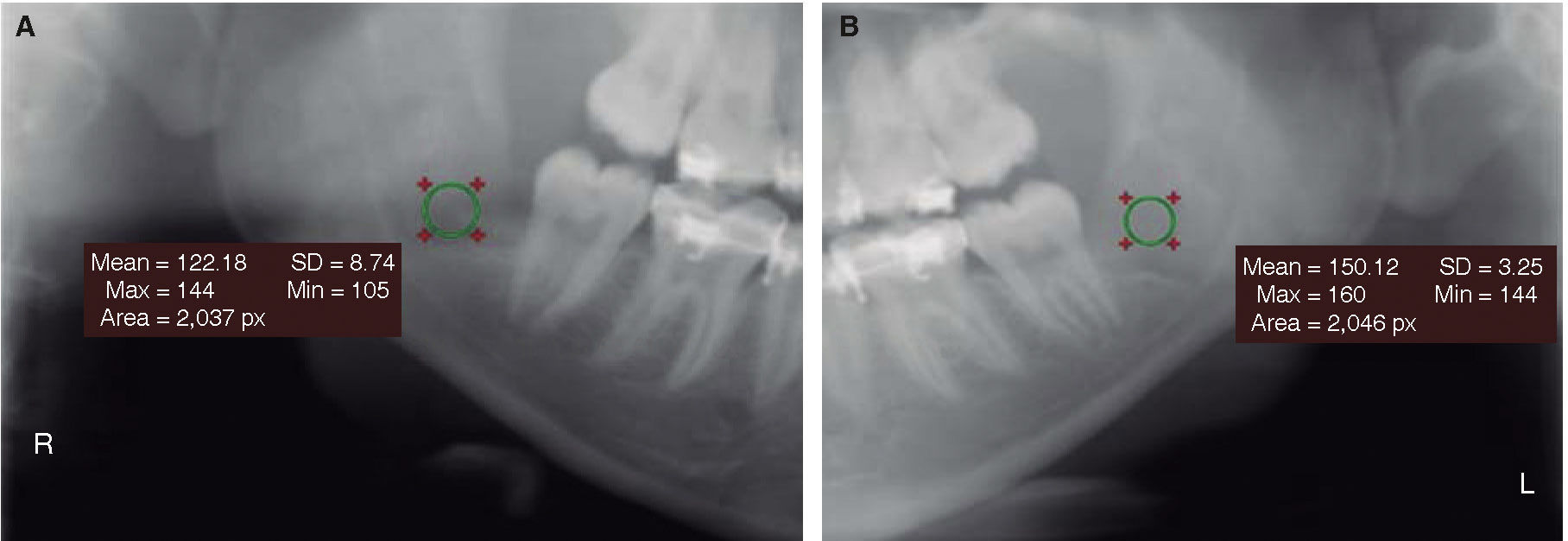
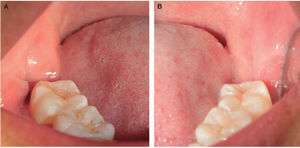
Eight days after surgery, wounds were inspected to ascertain whether they were still open or closing (Figure 2). A digital panoramic radiograph was taken 60 days after surgery. (I-max Touch 3d Owandy Radiology) to be then processed with software RadiAnt DICOM Viewer, version 2.2.9.10728, with Ellipse tool. This is a medical-dental software which quantifies image contrast density with the mean of pixel value or Hounsfield units for computerized axial tomography images (Figure 3).16
Ethical considerationsMethodological, bioethical and legal bases of the present study were analyzed. Study was approved by the Ethics Subcommittee for Research in Human Beings of the Central University, Ecuador.
Statistical analysisThe present study was conducted with Pearson χ2 test for qualitative variables, which, in this case, was wound closure comparing both sides: where PRF was placed and the other side where PRF was not placed. T Student test was used for quantitative variables such as bone healing, which was quantified in software RadiAnt DICOM Viewer.
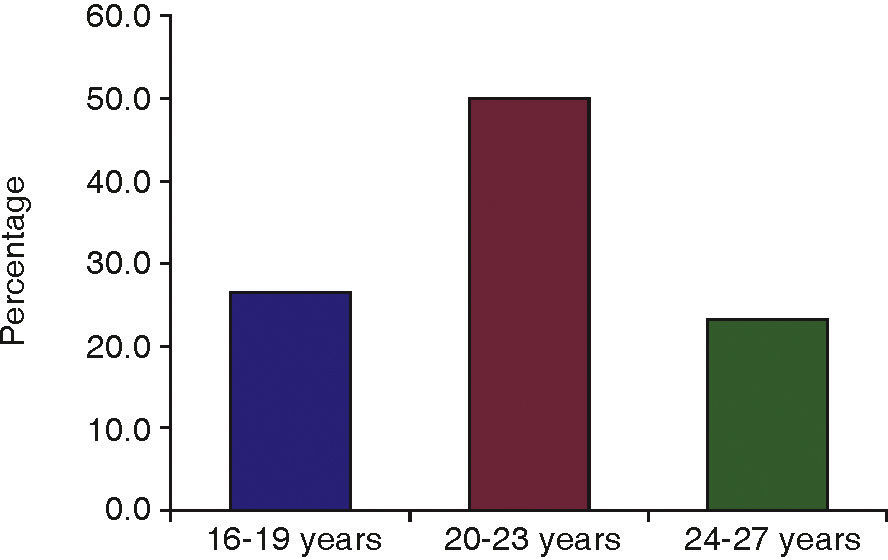
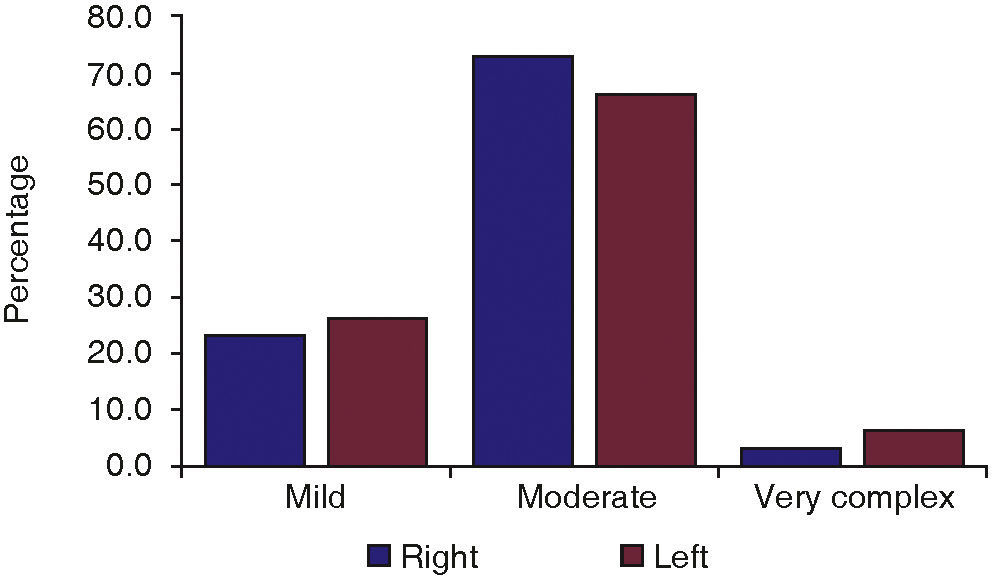
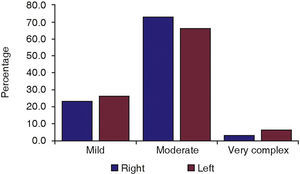
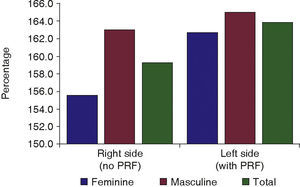
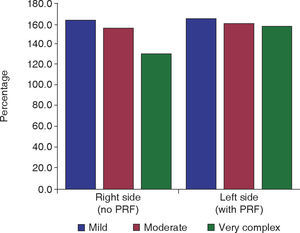
RESULTSThe present study included 30 patients, 15 males and 15 females. Patients were grouped according to age as follows: 8 patients ages 16-19 years, 15 patients aged 20-23 years and 7 patients aged 24-27 years (Figure 4). Pederson classification17 was used to establish extraction difficulty: as mild, moderate and very complex. Results were the following: 7 mild, 22 moderate and one very complex extractions in the right side, and 8 mild, 20 moderate and two very complex extractions in the left side (Figure 5).
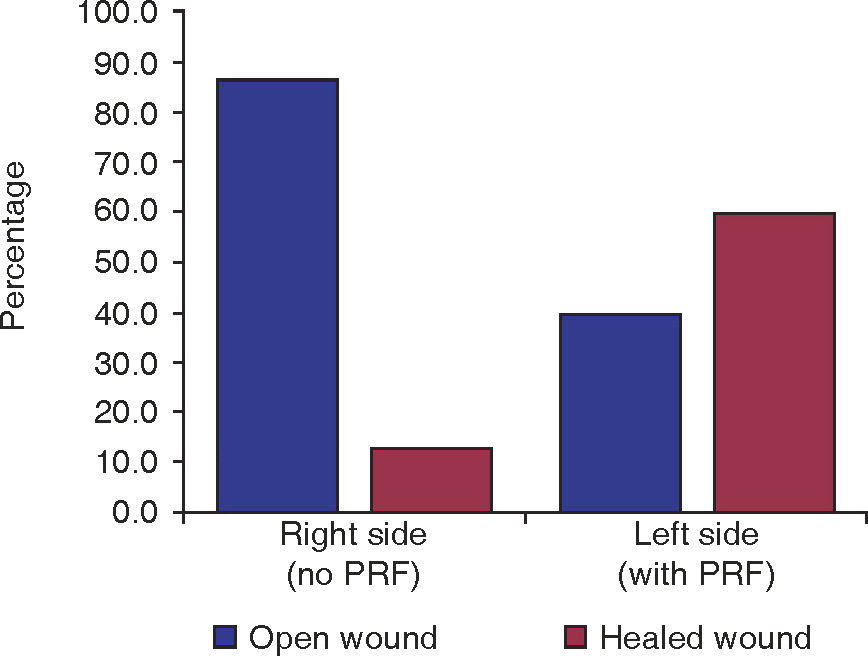
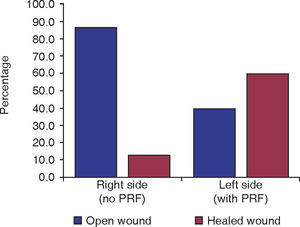
Gingival tissue healing in the surgical wound was as follows: open wound in 26 cases and closed wound in four cases in the control side; compared with 12 open wounds and 18 closed wounds in the left size, where PRF had been placed, showing thus significance of p < 0.001 (Figure 6). No differences were observed with respect to gender p = 1 or age p = 0.49 (Table I).
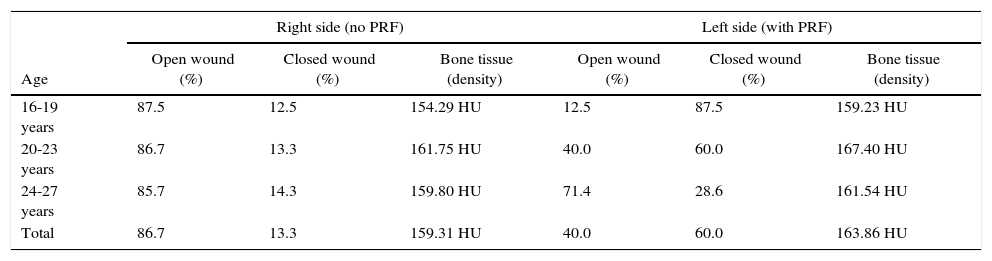
Soft and bone tissue healing with respect to age.
| Age | Right side (no PRF) | Left side (with PRF) | ||||
|---|---|---|---|---|---|---|
| Open wound (%) | Closed wound (%) | Bone tissue (density) | Open wound (%) | Closed wound (%) | Bone tissue (density) | |
| 16-19 years | 87.5 | 12.5 | 154.29 HU | 12.5 | 87.5 | 159.23 HU |
| 20-23 years | 86.7 | 13.3 | 161.75 HU | 40.0 | 60.0 | 167.40 HU |
| 24-27 years | 85.7 | 14.3 | 159.80 HU | 71.4 | 28.6 | 161.54 HU |
| Total | 86.7 | 13.3 | 159.31 HU | 40.0 | 60.0 | 163.86 HU |
Shows results with respect to age. Results did not exhibit differences in soft and bone tissue healing either with or without PRF.
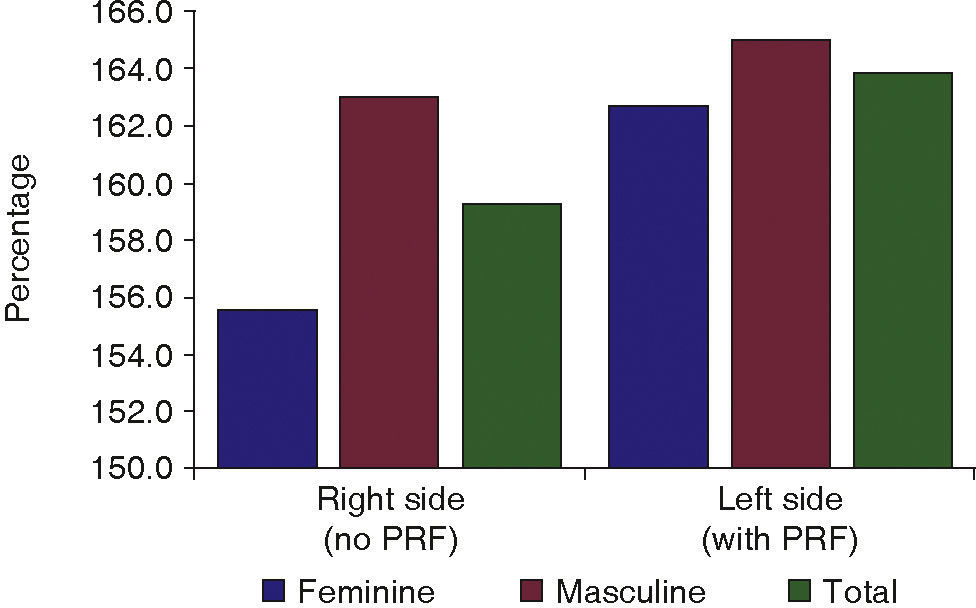
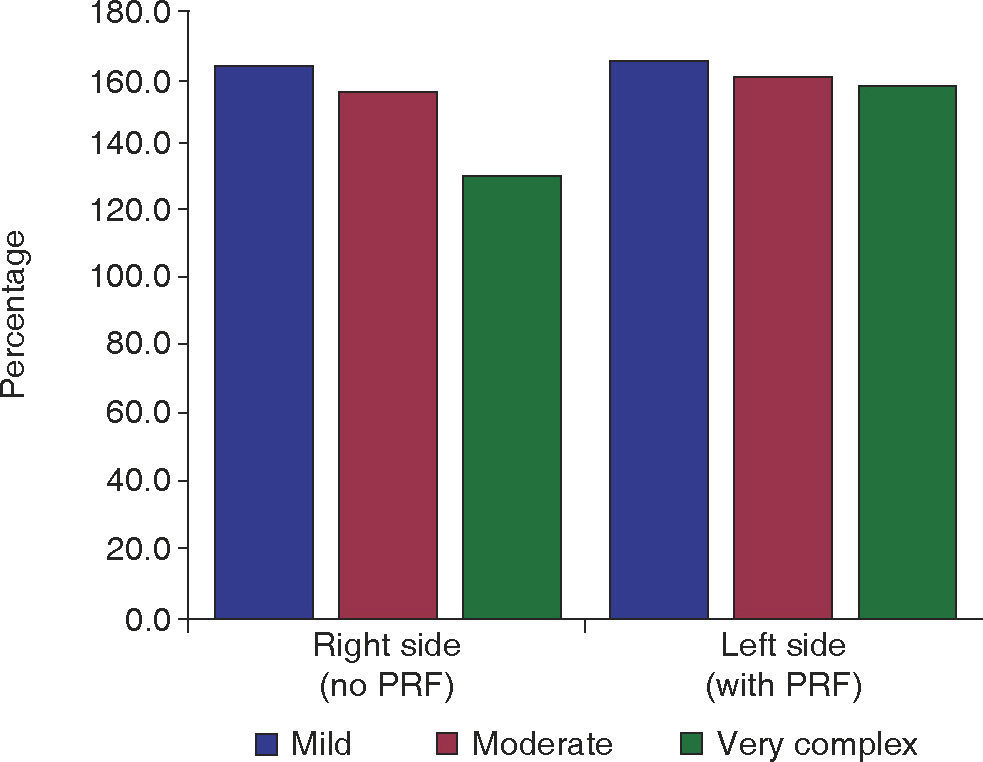
Bone tissue healing obtained better punctuation on the experimental side, with density values of 163 HU when compared to the control side where 159.3 HU were encountered (Figure 7); t Student test provided results of p = 0.015. No differences were observed with respect to gender and age (Table I). According to Pederson's punctuation scale and criteria proposal, with respect to difficulty of extraction, best results were obtained for groups with mild extraction complexity (Figure 8).
DISCUSSIONImproved and uncomplicated healing of wounds is highly desirable for patients after retained third molar extraction surgery processes. This fact has prompted research of related physicians and dentists in the area.18 Tissue repair processes take place due to growth factors found in platelet rich fibrin.19
So-called fibrin sealers are derived from human plasma; they replicate the final stages of blood clotting. These biocompatible and biodegradable compounds have been used for hemostasis and tissue healing.20
The following were factors that might have influenced results of the present study: age, gender, surgery complexity, bacterial plaque control, patient's routine and feeding habits. Gender, age and surgery complexity were selected out of all the aforementioned factors due to their reliability and availability for data collection.
The present study included 30 healthy patients, male and female, distributed in an equal percentage (50%) for each group. Patients were divided according to age into groups of 16-19 years, 20-23 years and 24-27 years. In all patients, left side of the mouth was considered the experimental group and the right side was considered control group. The left side was considered experimental due to the fact of reduced visibility for surgery when compared to the right side which normally exhibits better field of vision for the surgeon as well as easier approach for surgery.
Results of the present study were assessed through direct observation for tissue healing, and through panoramic X-rays for bone tissue. These X-rays were analyzed with software Radiant DICOM Viewer in order to calculate imaging density of the socket after extraction.
PRF use in our study exhibited a result of p < 0.001, thus indicating based on statistical data obtained, that soft tissue healing is enhanced with use of this compound.
Analysis of soft tissue healing according to gender showed p = 1, it was thus concluded that wound closing was not dependent on patient's gender. When data were processed according to age, χ2 test determined that in the experimental group age did not bear influence on soft tissue healing, showing a result of p = 0.49.
The present study concurred with similar studies conducted by Celio-Mariano et al,19 where platelet rich plasma, a PRF-like platelet concentrate, was placed. The study was performed on 15 volunteer patients, 7 male and 8 female, aged 18-22 years, where experimental group exhibited greater radiographic bone density after one, two and three months, p < 0.05.
In contrast to results obtained in the Kumar et al study21 conducted in 31 patients with average age of 26.1 years, the experimental group which received PRF in the socket after lower third molar extraction was composed of 16 patients; bone density assessed three months after third molar surgery exhibited a value of p = 0.083. Our study showed p values of p < 0.015 observed sixty days after third molar extraction surgery, interpreting thus this value as statistical data indicating that use of PRF bears influence on bone healing of control group.
Differences found among these results can be influenced by the manner in which bone density was evaluated, we used digital assessment in our study, whereas Kumar et al21 conducted analog evaluation by means of parameters studying directly panoramic X-rays.
In the Gürbützer et al study PRF application was assessed by means of bone gammagraphy four weeks after surgery, nevertheless no detectable results were observed in this examination. This difference with the results of other studies could be due to PRF preparation technique used, with a centrifuge device at 2,030rpm during 10minutes, as mentioned by Kumar et al.21
Obtained data on bone tissue healing were distributed according to age and gender similarly to soft tissue data. In the first group male gender exhibited better mean values, both with and without PRF. These values were 163.0 and 165.0 HU respectively; female gender group exhibited mean values of 155.6 HU without PRF use and 162.7 HU with PRF use.
Results were similar in the study conducted by Celio-Meriano,19 both in control and experimental groups male gender exhibited higher mean values than female gender.
Age was distributed into three groups, comparatively, in bone tissue healing, best mean values were observed for age groups in the experimental group, when compared to the control group, group of patients 20-23 years old exhibited best values in all groups.
Finally, tooth extraction difficulty was calculated according to Pedersen scale.17 The experimental group exhibited best mean values, as well as the subgroup called mild complexity extraction, nevertheless it was observed that complexity of surgery did not exhibit statistical influence with bone healing.
Finally, with use of t-Student test, significant difference was observed in the mean value of imaging density of the socket after extraction in digital X-rays. Results were improved when using PRF, since p = 0.015.
CONCLUSIONThe present study showed that soft and bone tissue healing improves with use of PRF, endorsing thus its effectiveness. When age groups were analyzed, the 20-23 years group exhibited better bone healing when compared to the 16-19 years group, which in turn exhibited better soft tissue healing. When comparing genders, males exhibited better healing than females. Finally, when analyzing third molar extraction difficulty, healing was not significantly influenced in all cases, either complex, of medium complexity or those cases where surgery became fast and easy.